Abstract
We investigated whether eldecalcitol has further significant effects on bone metabolic markers and bone mineral density (BMD) in osteoporosis patients having undergone long-term bisphosphonate treatment. Eldecalcitol treatment was initiated in 48 postmenopausal osteoporosis patients who had undergone bisphosphonate treatment with or without alfacalcidol treatment for more than 2 years (average period 6.3 years). Age, height, weight, total muscle volume, total fat volume, estimated glomerular filtration rate, and BMD at the lumbar spine, total hip, and distal third of the radius were measured as background data for each patient. Serum alkaline phosphatase, tartrate-resistant acid phosphatase 5b, calcium, and phosphate levels were measured at the baseline and 3 and 12 months after the initiation of eldecalcitol treatment, and BMD was measured at the baseline and 12 months after the initiation of eldecalcitol treatment. Tartrate-resistant acid phosphatase 5b level was significantly decreased at 3 and 12 months after the initiation of eldecalcitol treatment in comparison with the baseline level. There were no significant changes in alkaline phosphatase, calcium, or phosphate levels in comparison with the baseline levels. In addition, the lumbar spine BMD at 12 months after the initiation of treatment was significantly increased in comparison with the baseline level, although no significant changes in BMD at the total hip and distal third of the radius were observed. Eldecalcitol demonstrated significant effects in additionally decreasing the level of the bone resorption marker tartrate-resistant acid phosphatase 5b and increasing BMD at the lumbar spine, even in osteoporosis patients having undergone long-term bisphosphonate treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Eldecalcitol is a new active vitamin D3 analogue (1,25-dihydroxyvitamin D3) and has been shown to significantly increase lumbar spine and total hip bone mineral density (BMD) [1]. In addition, eldecalcitol has been found to decrease the incidence of both vertebral and wrist fractures in comparison with alfacalcidol [2, 3]. The effect of eldecalcitol on the risk of osteoporotic fracture has been shown to be dependent on the potent effect of eldecalcitol on BMD, bone structure, and bone turnover [3]. Regarding its effects on bone turnover, eldecalcitol has been demonstrated to suppress bone resorption markers such as urinary collagen N-telopeptide, the level of which was decreased by 20 % at 3 months after the start of treatment in comparison with the baseline level [1], and by 23 % at 3 years in comparison with that in patients undergoing alfacalcidol treatment [2]. On the basis of these results, eldecalcitol was approved for the treatment of osteoporosis in Japan.
A previous study using an animal model demonstrated that the inhibitory effect of eldecalcitol on bone resorption is related to the suppression of receptor activator of nuclear factor κB ligand (RANKL) expression in osteoblasts, the mechanism of which differs from that of other antiresorptive agents such as bisphosphonates [4]. Additionally, recent studies have demonstrated that the suppressive effect of eldecalcitol on bone resorption was additive to that of alendronate or raloxifene in an ovariectomized rat model [5, 6]. Therefore, we hypothesized that eldecalcitol would have an inhibitory effect on bone resorption even in osteoporosis patients who had undergone long-term bisphosphonate treatment. In this study, we investigated whether eldecalcitol has further effects on bone metabolic markers and BMD in postmenopausal osteoporosis patients having already undergone long-term bisphosphonate treatment.
Materials and methods
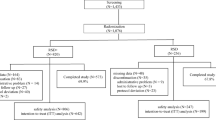
From July 2012 to July 2014, there were 73 postmenopausal osteoporosis patients receiving treatment in the outpatient clinic of our hospital who satisfied the following criteria:
-
1.
The patients had already undergone bisphosphonate treatment, including alendronate treatment (5 mg/day or 35 mg/week) or risedronate treatment (2.5 mg/day or 17.5 mg/week) with or without alfacalcidol treatment (1.0 μg/day), or alfacalcidol monotherapy for more than 2 years (average period 6.3 years; range 2–11 years). All patients were prescribed calcium lactate (3.0 g/day).
-
2.
They had no metabolic bone disease, such as hyperparathyroidism, Cushing’s syndrome, rheumatoid arthritis, diabetes mellitus, or renal disease, and had not received glucocorticoids or other antiosteoporosis agents according to their medical records.
-
3.
The absence of clinical fractures for 6 months before the start of eldecalcitol treatment had been monitored by plain radiographs.
-
4.
No significant changes in bone metabolic makers or BMD were observed regardless of bisphosphonate or alfacalcidol treatment for more than 2 years before the start of eldecalcitol treatment.
For all patients, we decided that the minimum significant change of serum tartrate-resistant acid phosphatase 5b (TRAP5b) level was more than 12.4 % according to the guidelines of the Japan Osteoporosis Society [7] and a significant increase of BMD was more than 3 % of the young adult mean in Japanese women. Seventy-three patients were asked to begin eldecalcitol treatment (0.75 μg/day), and consent was received from 65 patients. Institutional Review Board approval was obtained for this study.
The patients were divided into three subgroups on the basis of the drugs prescribed before the start of eldecalcitol treatment; the alfacalcidol group (ALF group; n = 17) changed from alfacalcidol monotherapy to eldecalcitol monotherapy, the bisphosphonate plus alfacalcidol group (ALF + BP group; n = 28) changed from bisphosphonate and alfacalcidol therapy to bisphosphonate and eldecalcitol therapy, and the bisphosphonate group (BP group; n = 20) had eldecalcitol added to bisphosphonate monotherapy. The duration of bisphosphonate or alfacalcidol administration before the start of eldecalcitol treatment was 8.4 ± 4.2 years (mean ± standard deviation) in the ALF group, 5.2 ± 2.3 years in the ALF + BP group, and 5.1 ± 2.9 years in the BP group.
Before the start of eldecalcitol treatment, the age, height, weight, total muscle mass, total fat mass, and BMD at the lumbar spine (L2–L4), total hip, and distal third of the radius were measured (QDR4500; Hologic, Waltham, MA, USA) as background data for each patient. Body composition was measured by a whole-body scan with the same machine as used for BMD measurement, with the system software providing estimates of lean and fat mass. Estimated glomerular filtration rate was calculated from the creatinine level for the assessment of renal function. The serum levels of total alkaline phosphatase (ALP; reference range 110–370 IU/l) and TRAP5b (reference range 120–420 mU/dl), as bone metabolic markers, as well as the serum levels of calcium (reference range 8.4–10.4 mg/dl), which was corrected against serum albumin level, and phosphate (reference range 2.5–4.5 mg/dl) were measured at the baseline and 3 and 12 months after the initiation of eldecalcitol treatment, whereas BMD was measured at the baseline and 12 months after the initiation of treatment. All data were collected prospectively. The average age was 72.0 ± 8.7 years (mean ± standard deviation; range 60–92 years). Informed consent was obtained from each patient before enrollment in the study, and the study was approved by the Institutional Review Board of the university.
The results are expressed as mean ± standard deviation. Statistical analyses for background data were performed with a one-way ANOVA, and for multiple comparisons, homogeneity of variances was assessed by Levene tests and Tukey’s post hoc tests. To compare the responses after the initiation of eldecalcitol treatment, two-way repeated measures ANOVA and Bonferroni’s multiple comparison tests were used. A p value of less than 0.05 was considered significant. Furthermore, for multiple comparisons of seven variables of serum level (ALP, TRAP5b, Ca, P) and BMD (LS, Hip, 1/3R), Bonferroni correction was applied and the cutoff of significance was set to 0.0063 (0.05/7). All analyses were performed with IBM SPSS Statistics version 22.
Results
Table 1 gives the background data for the patients, with no significant differences observed among the three subgroups except that the BMD at both the total hip and the distal third of the radius in the ALF group was significantly higher than that in the ALF + BP and BP groups (Table 1). For the patients in this study, the TRAP5b levels in the ALF + BP and BP groups were relatively high regardless of long-term bisphosphonate treatment (Table 1). The serum TRAP5b levels in all groups were significantly decreased at 3 months (ALF group, 326.5 ± 90.6 mU/dl; ALF + BP group, 268.7 ± 112.4 mU/dl; BP group, 275.3 ± 92.5 mU/dl) and 12 months (ALF group, 309.6 ± 113.8 mU/dl; ALF + BP group, 274.4 ± 117.7 mU/dl; BP group, 272.4 ± 121.6 mU/dl) after the initiation of eldecalcitol treatment in comparison with the baseline levels (Fig. 1). No significant changes in serum ALP levels at 3 months (ALF group, 204.0 ± 64.7 IU/l; ALF + BP group, 188.0 ± 70.0 IU/l; BP group, 204.0 ± 63.9 IU/l) and 12 months (ALF group, 191.3 ± 53.1 IU/l; ALF + BP group, 182.5 ± 67.8 IU/l; BP group, 205.7 ± 63.8 IU/l) (Fig. 2), calcium levels at 3 months (ALF group, 9.7 ± 0.93 mg/dl; ALF + BP group, 9.5 ± 0.49 mg/dl; BP group; 9.5 ± 0.47 mg/dl) and 12 months (ALF group, 9.6 ± 0.61 mg/dl; ALF + BP group, 9.4 ± 0.51 mg/dl; BP group, 9.5 ± 0.47 mg/dl) (Fig. 3), or phosphate levels at 3 months (ALF group, 3.5 ± 0.41 mg/dl; ALF + BP group, 3.3 ± 057 mg/dl; BP group, 3.7 ± 0.49 mg/dl) and 12 months (ALF group, 3.5 ± 0.54 mg/dl; ALF + BP group, 3.3 ± 0.51 mg/dl; BP group, 3.7 ± 0.5 mg/dl) (Fig. 4) after initiation of treatment were observed in comparison with the baseline levels. In addition, the lumbar spine BMD at 12 months after initiation of treatment was significantly increased in comparison with the baseline level in all groups (Table 2).
Changes in tartrate-resistant acid phosphatase 5b (TRAP5b) level before and after the initiation of eldecalcitol treatment. Serum TRAP5b levels in all groups were significantly decreased at 3 and 12 months after the initiation of eldecalcitol treatment in comparison with the baseline levels. One asterisk p < 0.005, two asterisks p < 0.001, diamonds alfacalcidol group, squares alfacalcidol plus bisphosphonate group, triangles bisphosphonate group
Changes in alkaline phosphatase (ALP) level before and after the initiation of eldecalcitol treatment. No significant changes in the serum level of ALP in any groups were observed at 3 and 12 months after the initiation of eldecalcitol treatment in comparison with the baseline levels. Diamonds alfacalcidol group, squares alfacalcidol plus bisphosphonate group, triangles bisphosphonate group
Changes in calcium level before and after the initiation of eldecalcitol treatment. No significant changes in the serum level of calcium in all groups were observed at 3 and 12 months after the initiation of eldecalcitol treatment in comparison with the baseline levels. Diamonds alfacalcidol group, squares alfacalcidol plus bisphosphonate group, triangles bisphosphonate group
Changes in phosphate (P) level before and after the initiation of eldecalcitol treatment. No significant changes in the serum level of phosphate in any group were observed at 3 and 12 months after the initiation of eldecalcitol treatment in comparison with the baseline levels. Diamonds alfacalcidol group, squares alfacalcidol plus bisphosphonate group, triangles bisphosphonate group
Discussion
Recent studies have demonstrated that eldecalcitol is more effective than alfacalcidol in preventing osteoporotic fractures, with a significant reduction in bone resorption markers observed in osteoporosis patients with vitamin D sufficiency [2, 3]. In this study, we showed that the substitution of eldecalcitol therapy for alfacalcitol monotherapy afforded further significant effects via a decrease in TRAP5b levels and an increase of BMD in patients who had previously undergone long-term alfacalcidol monotherapy. Notably, we demonstrated that eldecalcitol showed significant effects on TRAP5b levels and BMD even in patients who had undergone bisphosphonate treatment for more than 2 years. Moreover, the substitution of eldecalcitol therapy for alfacalcidol therapy also demonstrated these significant effects in patients receiving alfacalcidol and bisphosphonate combination treatment for more than 2 years. We therefore consider that the results of this study provide new information regarding the further significant effects of eldecalcitol on bone resorption markers and BMD in osteoporosis patients having undergone long-term bisphosphonate treatment.
Bisphosphonate is well known as a potent antiresorptive agent that inhibits the bone resorptive capacity of mature osteoclasts and may also induce osteoclast apoptosis [8]. However, this study showed that eldecalcitol significantly inhibited TRAP5b levels in osteoporosis patients despite long-term bisphosphonate treatment. A previous study demonstrated that eldecalcitol and alendronate combination treatment improved the mechanical properties of the lumbar spine and femur in an ovariectomized rat model, and also indicated that the mechanism underlying this improvement was based on the additive effect of combined therapy with the two antiresorptive agents while maintaining bone formation [5]. These studies suggested that the inhibitory effect of eldecalcitol on bone resorption could proceed via a pathway different from that for bisphosphonate, and these results seemed to correspond with those of our study.
Several studies using animal models have shown that the inhibitory effect of eldecalcitol on bone resorption is based on the suppression of osteoclast number, activity, and function without promoting osteoclast apoptosis [4, 9, 10]. A recent study also demonstrated that eldecalcitol administration significantly suppressed RANKL expression and reduced the RANKL-positive cell surface perimeter of bones in mice [4]. Takahashi et al. [10, 11] also identified the direct osteoclast progenitors, called “cell-cycle-arrested quiescent osteoclast precursors” (QOPs), and detected QOPs in bone marrow and peripheral blood. QOPs are committed osteoclast precursors, and some QOPs circulate in the blood vessels to locate to appropriate sites for osteoclast formation [10]. Kikuta et al. [12] demonstrated that eldecalcitol controls osteoclastogenesis and bone resorption by blocking the migration and positioning of osteoclasts in bone tissues and increasing the circulation of osteoclast precursors. These studies indicated that the pathway by which eldecalcitol inhibits osteoclast formation and function differs from that of bisphosphonate. We therefore speculated that eldecalcitol would have an additional inhibitory effect on bone resorption, which might be associated with an increase in BMD, in osteoporosis patients even after long-term bisphosphonate treatment.
The distinctive significant effects of eldecalcitol (i.e., a decrease in TRAP5b level and an increase in BMD) were observed in the patients in all of the study groups. On the other hand, long-term bisphosphonate treatment before the start of eldecalcitol treatment had no significant effects on bone metabolic markers or BMD for more than 2 years. We therefore believe that the additional prescription of eldecalcitol is a practical treatment for cases in which long-term bisphosphonate treatment has been found to be ineffective.
A previous report indicated that the serum TRAP5b level is minimally affected by renal dysfunction although a high prevalence of chronic kidney disease has been increasingly recognized in elderly female patients [7], which is consistent with our results. With regard to hypercalcemia as the most careful adverse event by eldecalcitol treatment, we did not find a significant change of serum calcium levels in all groups at 3 and 12 months after the initiation of eldecalcitol treatment in comparison with the baseline levels. On the other hand, in further studies the serum calcium level needs to be measured within 1 month after the additional administration of eldecalcitol because the serum calcium level might be increased in early phase after treatment [13].
No significant changes in ALP level or overreductions in TRAP5b level after the initiation of eldecalcitol treatment were observed in any of the three groups. These results suggest that simultaneous treatment with two antiresorptive agents such as bisphosphonate and eldecalcitol does not lead to an oversuppression of bone turnover even in osteoporosis patients who have undergone long-term bisphosphonate treatment.
The total pool of ALP in serum consists of several isozymes from various tissues, although isozymes from bone tissue account for almost 50 % of the total ALP pool [7]. We therefore need to assess further the serum levels of bone ALP or N-terminal propeptide of type I procollagen to conclude whether eldecalcitol had any effect on bone formation in these patients.
We believe that the administration of eldecalcitol is worthwhile because of the expected further suppression of bone resorption markers and increase in BMD, even in patients who have previously undergone long-term bisphosphonate treatment. In this study, we demonstrated the effectiveness of eldecalcitol on bone metabolic markers and BMD; however, we also need to investigate the long-term effects of eldecalcitol on bone metabolic markers, BMD, and fracture prevalence in these patients in further studies.
There were several limitations to this study. First, we measured bone metabolic markers at 3 and 12 months after the initiation of eldecalcitol treatment. Ideally, we should also perform the measurement within 3 months of and at more than 1 year after initiation of treatment to evaluate the effects in both the early stage or the late stage. Second, we did not evaluate the effect on the incidence of osteoporotic fractures. Third, serum ALP, TRAP5b, calcium and phosphate levels were not measured at the same time because the samples were individually taken from patient blood samples at the time of examination in the clinic. Fourth, we did not measure serum intact parathyroid hormone levels, which might have affected the serum calcium level, because the measurement is not covered by health insurance for the treatment of primary osteoporosis patients.
In conclusion, we demonstrated that eldecalcitol has further significant effects on the level of the bone resorption marker TRAP5b (decrease) and BMD (increase) at the lumbar spine after the start of treatment in postmenopausal osteoporosis patients who have previously undergone long-term bisphosphonate treatment.
References
Matsumoto T, Miki T, Hagino H, Sugimoto T, Okamoto S, Hirota T, Tanigawara Y, Hayashi Y, Fukunaga M, Shiraki M, Nakamura T (2005) A new active vitamin D, ED-71, increases bone mass in osteoporotic patients under vitamin D supplementation: a randomized, double-blind, placebo-controlled clinical trial. J Clin Endocrinol Metab 90:5031–5036
Matsumoto T, Ito M, Hayashi Y, Hirota T, Tanigawara Y, Sone T, Fukunaga M, Shiraki M, Nakamura T (2011) A new active vitamin D3 analog, eldecalcitol, prevents the risk of osteoporotic fractures — a randomized, active comparator, double-blind study. Bone 49:605–612
Nakamura T, Takano T, Fukunaga M, Shiraki M, Matsumoto T (2013) Eldecalcitol is more effective for the prevention of osteoporotic fractures than alfacalcidol. J Bone Miner Metab 31:417–422
Harada S, Mizoguchi T, Kobayashi Y, Nakamichi Y, Takeda S, Sakai S, Takahashi F, Saito H, Yasuda H, Udagawa N, Suda T, Takahashi N (2012) Daily administration of eldecalcitol (ED-71), an active vitamin D analog, increases bone mineral density by suppressing RANKL expression in mouse trabecular bone. J Bone Miner Res 27:461–473
Sakai S, Endo K, Takeda S, Mihara M, Shiraishi A (2012) Combination therapy with eldecalcitol and alendronate has therapeutic advantages over monotherapy by improving bone strength. Bone 50:1054–1063
Takeda S, Sakai S, Shiraishi A, Koike N, Mihara M, Endo K (2012) Combination treatment with eldecalcitol (ED-71) and raloxifenen improves bone mechanical strength by suppressing bone turnover and increasing bone mineral density in ovariectomized rats. Bone 53:167–173
Nishizawa Y, Ohta H, Miura M, Inaba M, Ichimura S, Shiraki M, Takada J, Chaki O, Hagino H, Fujiwara S, Fukunaga M, Miki T, Yoshimura N (2013) Guidelines for the use of metabolic markers in the diagnosis and treatment of osteoporosis (2012 edition). J Bone Miner Metab 31:1–15
Azuma Y, Oue Y, Kanatani H, Ohta T, Kiyoki M, Komoriya K (1998) Effects of continuous alendronate treatment on bone mass and mechanical properties in ovariectomized rats: comparison with pamidronate and etidronate in growing rats. J Pharmacol Exp Ther 286:128–135
de Freitas PH, Hasegawa T, Takeda S, Sasaki M, Tabata C, Oda K, Li M, Saito H, Amizuka N (2011) Elcecalcitol, a second-generation vitamin D analog, drives bone minimodeling and reduces osteoclastic number in trabecular bone of ovariectomized rats. Bone 49:335–342
Takahashi N (2013) Mechanism of inhibitory action of eldecalcitol, an active vitamin D analog, on bone resorption in vivo. J Steroid Biochem Mol Biol 136:171–174
Muto A, Mizoguchi T, Udagawa N, Ito S, Kawahara I, Abiko Y, Arai A, Harada S, Kobayashi Y, Nakamichi Y, Penninger JM, Noguchi T, Takahashi N (2011) Lineage-committed osteoclast precursors circulate in blood and settle down into bone. J Bone Miner Res 26:2978–2990
Kikuta J, Kawamura S, Okiji F, Shirazaki M, Sakai S, Saito H, Ishii M (2013) Sphingosine-1-phosphate-mediated osteoclast precursor monocyte migration is a critical point of control in antibone-resorptive action of active vitamin D. Proc Natl Acad Sci U S A 110:7009–7013
Sasaki N, Tsunoda M, Ikee R, Hashimoto N (2015) Efficacy and safety of eldecalcitol, a new active vitamin D3 analog, in the bone metabolism of postmenopausal women receiving maintenance hemodialysis. J Bone Miner Metab 33:213–220
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that have no conflict of interest.
About this article
Cite this article
Iba, K., Sonoda, T., Takada, J. et al. Further significant effects of eldecalcitol on bone resorption markers and bone mineral density in postmenopausal osteoporosis patients having undergone long-term bisphosphonate treatment. J Bone Miner Metab 35, 171–176 (2017). https://doi.org/10.1007/s00774-016-0738-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-016-0738-y