Abstract
Bone mineral density (BMD) seems not to be decreased in young patients given long-term suppressive doses of levothyroxine (LT4), but information regarding the bone microstructure in these patients is lacking. The aim of this study was to determine whether supraphysiologic doses of LT4, initiated during childhood or adolescence for treatment of differentiated thyroid carcinoma (DTC), have any detrimental effects on bone microarchitecture as evaluated by high-resolution peripheral quantitative computed tomography (HR-pQCT). Seventeen patients (27.3 ± 7.1 years old) with DTC with subclinical hyperthyroidism since adolescence and 34 healthy volunteers matched for age, sex, and body mass index were studied by dual-energy X-ray absorptiometry (DXA) to determine the areal BMD at the lumbar spine, hip, and proximal third of the radius. Volumetric BMD and structural parameters of the trabecular and cortical bone were assessed by HR-pQCT of the distal radius and distal tibia. DTC patients were given suppressive doses of LT4 starting at a mean age of 12.6 years, and the mean duration of treatment was 14.2 years. In DTC patients, clinical parameters did not correlate with DXA or HR-pQCT parameters. No differences were found between the patients and controls with respect to BMD and Z scores at any site evaluated by DXA, and no differences were found in the bone microstructure parameters evaluated by HR-pQCT. This cross-sectional study suggests that long-standing suppressive therapy with LT4 during the attainment of peak bone mass may have no significant adverse effects on bone density or microarchitecture.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Differentiated thyroid carcinoma (DTC), both papillary and follicular, is rare in pediatric patients, with an incidence between 2.6 and 12.9 % [1]. Primary treatment comprises thyroidectomy followed by radioiodine ablation and supraphysiologic doses of levothyroxine (LT4) with the purpose of suppressing serum TSH and therefore inhibiting the growth of residual neoplastic tissue and preventing progression of thyroid cancer and relapse. Despite increased relapse-free survival, long-term subclinical hyperthyroidism may be related to side effects on bone mineral density (BMD) and cardiac function, especially in the elderly [2].
TSH-suppressive therapy has not been associated with decreased BMD in premenopausal women and men as evaluated by dual-energy X-ray absorptiometry (DXA) [3–6]. A study with young patients also did not suggest a detrimental effect of LT4 on the attainment of peak bone mass [7]. However, DXA is based on a two-dimensional interpretation of a three-dimensional structure, and cannot evaluate bone microarchitecture.
To our knowledge, no study has addressed whether suppressive doses of LT4 for treatment of thyroid cancer, initiated before the attainment of peak bone mass, affects the three-dimensional microstructure of bone using the new technique of high-resolution peripheral quantitative computed tomography (HR-pQCT), and this is the purpose of our study.
Materials and methods
This cross-sectional observational study was conducted from December 2011 until July 2012 in non-Caucasian patients with DTC by the National Institute of Cancer in Rio de Janeiro, Brazil. The strict selection criteria were as follows: (1) age 20–50 years, and all women needed to have regular menses; (2) diagnosis and surgical treatment of DTC before age 16 years; (3) treatment with LT4 at suppressive doses for at least 5 years before entry to the study. All patients underwent total thyroidectomy plus 131I ablation and were counseled to maintain suppressive LT4 therapy. They were reevaluated two to three times per year, and LT4 doses were adjusted to maintain serum TSH levels under 0.1 mU/l and free thyroxine (FT4) levels within the normal range. Age- and sex-matched healthy individuals, who did not have a history of thyroid dysfunction and had serum TSH levels within the reference range, were recruited as a control group. The exclusion criteria for all participants were as follows: pregnancy, alcoholism, chronic gastrointestinal diseases, renal or hepatic impairment, and exposure to medications that affect bone (anticonvulsants, glucocorticoids, or antiosteoporotic drugs). The National Institute of Cancer and the Federal University of Rio de Janeiro ethics committees approved the study, and all participants provided informed consent.
Body mass index (weight divided by the square of height) was calculated. Serum TSH levels were measured in the control group to confirm normality. In DTC patients, mean serum TSH and FT4 levels during the last 5 years of follow-up were recorded for analysis. TSH and FT4 were measured using third-generation chemiluminescent immunometric assays (Immulite® 2000; Siemens Healthcare, Camberley, UK); the reference ranges were 0.4–4.0 µIU/ml and 0.8–1.9 ng/dl, respectively.
The BMD at the lumbar spine (L1–L4), femoral neck, total femur, and proximal third of the radius of the nondominant arm was measured by DXA with a Prodigy-GE densitometer (GE Lunar Prodigy Advance; GE Healthcare, Madison, WI, USA). BMD was expressed in absolute values (g/cm2) and as standard deviations (SD) from the expected BMD for the age-matched population (Z score) according to the National Health and Nutrition Examination Survey III (NHANES III) database. The criteria for low bone mass for age was a Z score of −2 SD or lower [18]. The coefficient of variation for the BMD measurements in normal subjects at our institution is 1.5 % in the lumbar spine and 1.8 % in the femoral neck.
The volumetric BMD and the microarchitecture were measured in the nondominant distal radius and the distal tibia using a three-dimensional HR-pQCT system (XtremeCT; Scanco Medical, Brüttisellen, Switzerland). This system uses a two-dimensional detector array combined with a 0.08-mm point-focus X-ray tube, thus making possible the simultaneous acquisition of a stack of parallel computed tomography slices with a nominal resolution (voxel size) of 82 µm. From each skeletal site, 110 slices were obtained, and these produced a three-dimensional representation of approximately 9 mm in the axial direction. An anteroposterior scout view was used to define the measured region, and a reference line was manually placed at the endplate of the radius and tibia. The first computed tomography slice was 9.5 and 22.5 mm proximal to the reference line for the distal radius and the distal tibia, respectively. The attenuation data were converted to equivalent hydroxyapatite densities. The scans were evaluated and excluded if motion artifacts were discovered.
The outcome variables that were used in our analysis included the volumetric BMD (grams of hydroxyapatite per cubic centimeter) for the entire, trabecular, and cortical regions; the cortical thickness (CtTh; mm); and the trabecular bone volume (BV) fraction [ratio of BV to total volume (TV); %], trabecular thickness (TbTh; mm), trabecular number (TbN; mm−1), trabecular separation (TbSp; mm), and SD of the TbSp (mm). TbN is defined as the inverse of the mean distance between the midline of the trabeculae. TbTh and TbSp are calculated on the basis of TbN and the derived BV/TV [i.e., TbTh = BV/TV/TbN and TbSp = (1 − BV/TV)/TbN]. For the cortical region, the mean CtTh was calculated as the cortical volume divided by the outer bone surface. The reproducibility of density-based measurements is generally less than 1 %, and is typically between 3 and 5 % for bone structure parameters [8].
Statistical analysis
Data were analyzed using SPSS for Mac OS, version 20 (SPSS, Chicago, IL,USA) and are expressed as the mean ± SD. The Kolmogorov–Smirnov test was performed to analyze the distribution pattern of numerical variables. The groups were compared using an unpaired t test or a Mann–Whitney U test, as appropriate. The Spearman rank-order test was performed to evaluate the correlations between clinical parameters (age at onset of TSH-suppressive therapy, duration of subclinical hyperthyroidism, and mean TSH levels) and all DXA and HR-pQCT parameters. A level of 0.05 or below was considered significant in all statistical procedures.
Results
Among the 830 patients with DTC regularly seen in the National Institute of Cancer in Rio de Janeiro, 65 underwent surgery before they were16 years old. Twenty-three DTC patients fulfilled the inclusion criteria, and six were excluded (one was pregnant, one had uncompensated hypoparathyroidism and used LT4 irregularly, and four refused to participate). Therefore, the DTC group comprised 16 patients with papillary carcinoma and one patient with follicular carcinoma. Fifteen of the patients were women and two were men, aged 20–42 years (mean 27.3 ± 7.1 years) at the start of the study. They were given TSH-suppressive therapy starting at a mean age of 12.6 ± 2.2 years, and therapy was maintained for 14.2 ± 7.2 years. The minimal and maximal LT4 doses to achieve effective TSH suppression were 1.98 and 3.64 µg/kg/day, respectively. The mean TSH and FT4 levels in the last 5 years were 0.17 ± 0.16 µIU/ml, and 1.59 ± 0.14 ng/dl, respectively. The control group comprised 34 healthy individuals (31 females and 3 males, aged 20–43 years). None of the participants were taking calcium or vitamin D supplements.
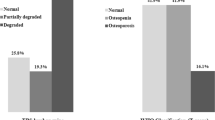
No differences were found between DTC patients and controls concerning age, anthropometric data, and densitometric data, even after the exclusion of the male patients. None of the participants, regardless of the group, had lower than expected BMD at any site evaluated by DXA (Table 1).
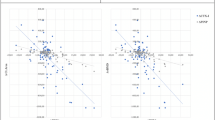
No significant correlations were found between age at onset of TSH-suppressive therapy, duration of subclinical hyperthyroidism, and mean TSH levels in the last 5 years and bone parameters namely, absolute BMDs, BMD Z scores, and HR-pQCT data, even after the exclusion of the male patients.
Microstructure parameters did not significantly differ between groups, even after the exclusion of the male patients (Table 2).
Discussion
This is the first study to evaluate whether suppressive doses of LT4 initiated during adolescence to treat DTC affect BMD as well as bone microarchitecture using HR-pQCT. The hypothesis was that the subclinical hyperthyroidism in childhood and adolescence could limit the acquisition of optimal peak bone mass. The results confirm no effect on BMD or bone structure.
Childhood and adolescence are periods of rapid skeletal growth and bone mineral accrual, through modeling and remodeling. In childhood, bone acquisition occurs slowly, whereas the greatest acquisition of bone occurs during puberty: approximately 85–90 % of final adult bone mass is acquired before the age of 20 years [9]. After this peak, BMD remains relatively stable in men and until menopause in women [10]. A lower than expected bone mass during puberty contributes to osteoporosis in later life [9, 10].
Overt hyperthyroidism is clearly detrimental to bone. Osteoporosis has traditionally been attributed to the high circulating levels of thyroid hormone and results from high bone turnover, with a disproportionate increase in bone resorption compared with bone formation. Studies in both adults [11, 12] and children [13, 14] with untreated hyperthyroidism demonstrated significantly decreased BMD compared with the levels in healthy controls. In these patients, decreased BMD occurs particularly in areas rich in cortical bone [14–16]. However, the skeletal effects of subclinical hyperthyroidism are a matter of debate.
Previous studies in patients with well-differentiated thyroid cancer receiving suppressive LT4 therapy have shown conflicting results: no decrease in BMD at any age [5, 6], bone loss only in postmenopausal women [17], or deleterious effects in both premenopausa and postmenopausal patients [18, 19]. Systematic reviews of BMD in these patients have reported diverse conclusions [3, 4].
There are very few data addressing subclinical hyperthyroidism and bone mass in pediatric patients. Radetti et al. [20] showed a significant reduction of bone mineral content in 20 children and adolescent girls taking high doses of LT4 (120 µg/m2/kg) for 6–96 months for nontoxic goiter, Hashimoto’s thyroiditis, or thyroid cancer compared with controls. On the other hand, 1 year of therapy with LT4 in doses of 1.2–1.5 mg/kg (adjusted to keep TSH levels in the normal to low range and FT4 levels in the normal to high range) had no negative impact on bone density and remodeling in a group of 21 adolescent girls with euthyroid diffuse goiter [21]. In the last two studies, the patients were younger than 20 years and had not yet achieved peak bone mass. Our results agree with those of Poomthavorn et al. [7], who reported no detrimental effect on peak bone mass attainment in 18 young adults receiving suppressive doses of LT4 during adolescence for Hashimoto’s thyroiditis and euthyroid goiter.
Published data on bone microarchitecture and hyperthyroidism are limited. Histomorphometric analyses of iliac crest biopsy specimens in 22 hyperthyroid patients demonstrated a preponderance of osteoclastic resorption in cortical bone, leading to an increase of cortical porosity, which improved after 4 months of antithyroid medication. The amount of trabecular bone was unchanged [15].
Quantitative computed tomography (QCT) is a three-dimensional tool for imaging bone density that permits the investigator to distinguish between cortical and trabecular bone. Two studies assessed bone mass in patients with hyperthyroidism using QCT. Numbenjapon et al. [14] assessed 18 children and adolescents using QCT performed before the start of antithyroid therapy, and showed that cortical bone density was significantly lower in the patients than in the controls. In another study, Numbenjapon et al. [16] studied 15 children and adolescents undergoing treatment with antithyroid medication and analyzed them with QCT before treatment and 1 and 2 years after treatment; they demonstrated a significant improvement and normalization of cortical bone density after 1 and 2 years, respectively.
HR-pQCT is a new medical imaging tool that evaluates the bone microstructure at the distal radius and distal tibia, and it is thus considered to be a virtual bone biopsy. Its allows the measurement of volumetric BMD and details of the trabecular and cortical bone components, such as trabecular BV fraction (BV/TV), TbTh, TbN, TpSp, and CtTh. HR-pQCT has been used to identify modifications of the bone structure that are not captured by BMD measurements [8]. For these reasons, we believe that HR-pQCT would be able to detect early and discrete alterations in the bone microarchitecture of the young patients included in our study.
Our study had certain limitations. The cross-sectional study design did not allow us to ensure that all patients maintained adequate TSH suppression during the critical period of peak bone mass acquisition. Owing to the rarity of DTC in the pediatric population, the sample size was small, which may have made a beta error in data interpretation. We thus speculate if the alterations in cortical bone microstructure would be significant in larger samples.
In conclusion, the present study shows that long-standing TSH suppression for treatment of DTC since childhood or adolescence may have no significant adverse effects on bone density accrual or bone microarchitecture. More prospective studies are needed to confirm these findings.
References
Vaisman F, Bulzico DA, Pessoa CHCN, Bordallo MAN, Mendonça UBT, Dias FL, Coeli CM, Corbo R, Vaisman M (2011) Prognostic factors of a good response to initial therapy in children and adolescents with differentiated thyroid cancer. Clinics 66:1–6
Biondi B, Cooper DS (2010) Benefits of thyrotropin suppression versus the risks of adverse effects in differentiated thyroid cancer. Thyroid 20:135–146
Murphy E, Williams GR (2004) The thyroid and the skeleton. Clin Endocrinol (Oxf) 61:285–298
Heemstra KA, Hamdy NAT, Romijn JA, Smit JWA (2006) The effects of thyrotropin-suppressive therapy on bone metabolism in patients with well-differentiated thyroid carcinoma. Thyroid 16:583–591
Reverter JL, Colome E, Holgado S, Aguilera E, Soldevila B, Mateo L, Sanmartí A (2010) Bone mineral density and bone fracture in male patients receiving long-term suppressive levothyroxine treatment for differentiated thyroid carcinoma. Endocrine 37:467–472
Reverter JL, Holgado S, Alonso N, Salinas I, Granada ML, Sanmartí A (2005) A lack of deleterious effect on bone mineral density of long-term thyroxine suppressive therapy for differentiated thyroid carcinoma. Endocr Relat Cancer 12:973–981
Poomthavorn P, Mahachoklertwattana P, Ongphiphadhanakul B, Preeyasombat C, Rajatanavin R (2005) Exogenous subclinical hyperthyroidism during adolescence: effect on peak bone mass. J Pediatr Endocrinol Metab 18:463–469
Madeira M, Neto LV, de Paula Paranhos Neto F, Barbosa Lima IC, Carvalho de Mendonça LM, Gadelha MR, Fleiuss de Farias ML (2013) Acromegaly has a negative influence on trabecular bone, but not on cortical bone, as assessed by high-resolution peripheral quantitative computed tomography. J Clin Endocrinol Metab 98:1734–1741
Heaney RP, Abrams S, Dawson-Hughes B, Looker A, Marcus R, Matkovic V, Weaver C (2000) Peak bone mass. Osteoporos Int 11:985–1009
Simon LS (2005) osteoporosis. Clin Geriatr Med 21:603–629
Karga H, Papapetrou PD, Korakovouni A, Papandroulaki F, Polymeris A, Pampouras G (2004) Bone mineral density in hyperthyroidism. Clin Endocrinol (Oxf) 61:466–472
Jodar E, Munoz-Torres M, Escobar-Jimenez F, Quesada M, Luna JD, Olea N (1997) Antiresorptive therapy in hyperthyroid patients: longitudinal changes in bone and mineral metabolism. J Clin Endocrinol Metab 82:1989–1994
Lucidarme N, Ruiz JC, Czernidrow P, Leger J (2000) Reduced bone mineral density at diagnosis and bone mineral recovery during treatment in children with Graves’ disease. J Pediatr 137:56–62
Numbenjapon N, Costin G, Gilsanz V, Pitukcheewanont P (2007) Low cortical bone density measured by computed tomography in children and adolescents with untreated hyperthyroidism. J Pediatr 150:527–530
Mosekilde L, Melsen F (1978) Effect of antithyroid treatment on calcium–phosphorus metabolism in hyperthyroidism. II: bone histomorphometry. Acta Endocrinol 87:751–758
Numbenjapon N, Costin G, Pitukcheewanont P (2011) Normalization of cortical bone density in children and adolescents with hyperthyroidism treated with antithyroid medication. Osteoporos Int 23:2277–2282
Stepan JJ, Limanova Z (1992) Biochemical assessment of bone loss in patients on long-term thyroid hormone treatment. Bone Miner 17:377–388
Diamond T, Nery L, Hales I (1991) A therapeutic dilemma: suppressive doses of thyroxine significantly reduce bone mineral measurements in both premenopausal and postmenopausal with thyroid carcinoma. J Clin Endocrinol Metab 72:1184–1188
Jodar E, Begona LM, Garcia L, Rigopoulou D, Martinez G, Hawkins F (1998) Bone changes in pre- and postmenopausal women with thyroid cancer on levothyroxine therapy: evolution of axial and appendicular bone mass. Osteoporos Int 8:311–316
Radetti G, Castellan C, Tato L, Platter R, Gentili L, Adani S (1993) Bone mineral density in children and adolescent females treated with high doses of l-thyroxine. Horm Res 39:127–131
Matusik P, Małecka-Tendera E, Franek E, Januszek-Trzciąkowska A (2010) Bone mineral density and metabolism in levothyroxine-treated adolescent girls with euthyroid diffuse goiter. Pol J Endocrinol 61:14–19
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Mendonça Monteiro de Barros, G., Madeira, M., Vieira Neto, L. et al. Bone mineral density and bone microarchitecture after long-term suppressive levothyroxine treatment of differentiated thyroid carcinoma in young adult patients. J Bone Miner Metab 34, 417–421 (2016). https://doi.org/10.1007/s00774-015-0680-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-015-0680-4