Abstract
A significant minority of women can suffer from postpartum posttraumatic stress disorder (PP-PTSD) following childbirth, in particular if involving obstetrical complications. While peritraumatic dissociation has been repeatedly shown to play a significant role in coping in the aftermath of trauma, little is known about peritraumatic dissociation in relation to positive adaptation following childbirth or failure thereof. We studied a large sample of 846 women who were on average 3 months postpartum. Participants completed an anonymous survey with psychometric measures pertaining to peritraumatic dissociation, PP-PTSD, postpartum depression, and other psychiatric symptoms. Women who had assisted vaginal deliveries or unscheduled Cesareans reported higher peritraumatic dissociation levels than those who had regular vaginal deliveries or scheduled Cesareans. Peritraumatic dissociation predicted PP-PTSD above and beyond premorbid and other childbirth-related factors. In contrast, we found that when controlling for PP-PTSD symptoms, higher levels of peritraumatic dissociation were associated with lower depression and other psychiatric symptom severity. Childbirth can evoke a dissociative response for some women. Rather than the mere focus on the mode of delivery and premorbid health, our findings highlight the role of the women’s immediate emotional response in PP-PTSD. Screening women for dissociative responses immediately following childbirth may offer a tool for identifying women at risk for PP-PTSD. The multifaceted role of peritraumatic dissociation in psychological adaptation as potentially adaptive on the one hand, and maladaptive on the other, warrants future scientific attention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Pregnancy and childbirth represent a period of psychological vulnerability and pose a high risk for psychiatric disorders for some women. While postpartum depression has received empirical attention in the past and has been documented as the most frequent childbirth complication (O’Hara and McCabe 2013; Segre et al. 2007), it is not the only psychological outcome of childbirth. Recent studies indicate that some women can suffer from childbirth-related postpartum posttraumatic stress disorder (PP-PTSD) following highly stressful childbirth experiences (Ayers et al. 2016; Dekel et al. 2017; Thiel et al. 2018; Yildiz et al. 2017). While PP-PTSD has gained growing empirical attention over the previous years, childbirth-related symptoms of posttraumatic stress were already described by French psychiatrist Louis Victor Marcé in the nineteenth century (Marcè 1858). In the first months postpartum, around a quarter of women report PP-PTSD symptoms and up to 6% endorse the full condition (Cook et al. 2018; Dekel et al. 2017), impairing functioning and well-being (McKenzie-McHarg et al. 2015). With around 138 million women giving birth (World Health Organization 2015), up to 34.5 million women may suffer the clinically relevant consequences of traumatic birth experiences every year, highlighting PP-PTSD as a global public health issue.
Peritraumatic dissociation (i.e., dissociation during a traumatic event) is defined as “a disruption and/or discontinuity in the normal integration of consciousness, memory, identity, emotion, perception, body representation, motor control, and behavior” (American Psychiatric Association [APA] 2013 p 291). Acute dissociative responses to trauma exposure play a central role in the development of PTSD (e.g., Briere et al. 2005). Ozer et al. (2003) conducted a comprehensive meta-analysis on PTSD predictors, including 16 empirical studies focusing on the role of peritraumatic dissociation in non-childbirth-related samples. Peritraumatic dissociation was the strongest predictor of non-childbirth-related PTSD (Ozer et al. 2003). Additionally, peritraumatic dissociation has been associated with other negative mental health outcomes such as hostility and depression (Punamäki et al. 2005). The most common explanation for the association between peritraumatic dissociation and PTSD is that peritraumatic dissociation interferes with the processing and encoding of the traumatic memory, hereby increasing the risk for PTSD (Koopman et al. 1994; van der Kolk and van der Hart 1989).
In contrast, peritraumatic dissociation may be viewed as a protective factor against emotional and physical pain and distress in light of exposure to traumatic stressors (e.g., Spiegel 1991). Following this reasoning, objectively amplified stressogenic, i.e., traumatic childbirth experiences, for instance assisted vaginal deliveries and unscheduled Cesareans, may be associated with higher rates of peritraumatic dissociation as a means of temporarily disconnecting from the stressful experience. Employed as a strategy to cope with the stressful experience, peritraumatic dissociation could then relate to better mental health outcomes in the wake of traumatic birth experiences. It has been argued that the chronic use of dissociative mechanisms in coping with the traumatic event, rather than peritraumatic dissociation during the event per se, may lead to the proposed interference in processing and encoding of the traumatic memory (Briere et al. 2005; Koopman et al. 1994). Thus, if dissociative reactions to the traumatic childbirth memory persist, memory processing and encoding may be disrupted, increasing the risk for the development of PTSD and comorbid psychiatric symptoms.
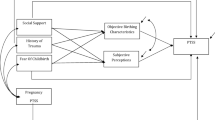
Ayers’ (2004) diathesis-stress model of the etiology of birth-related posttraumatic stress disorder conceptualizes PP-PTSD as the outcome of an interplay between pre-birth vulnerability, immediate birth-related, as well as post-birth factors (Ayers et al. 2016). Maternal mental health before birth and negative appraisal of the birth experience have been reported as commonly endorsed risk factors (e.g., Andersen et al. 2012). Nonetheless, a recent meta-analysis found peritraumatic dissociation during birth to be one of the risk factors most strongly associated with PP-PTSD (Ayers et al. 2016). Initial investigations into the role of peritraumatic dissociation in the development of PP-PTSD have not yielded homogenous findings. While some report peritraumatic dissociation to predict PP-PTSD symptoms (e.g., Haagen et al. 2015; Lev-Wiesel and Daphna-Tekoah 2010; Olde et al. 2005), another study found no such link (Vossbeck-Elsebusch et al. 2014). To the best of our knowledge, no prior study has investigated peritraumatic dissociation as a potentially adaptive factor in the context of postpartum psychological adaptation. We therefore have focused our investigation on dissociative responses in relation to childbirth, examining peritraumatic dissociation across different modes of delivery and its contribution to the development of postpartum psychopathology.
The present study aims to investigate the role of peritraumatic dissociation during childbirth in postpartum mental health. Specifically, we aim to shed light on the relationship between peritraumatic dissociation and PP-PTSD symptoms and other psychiatric symptoms. To this end, we hypothesize that (1) levels of peritraumatic dissociation differ across modes of delivery with higher levels reported for more stressogenic modes; (2) peritraumatic dissociation predicts PP-PTSD symptom levels above and beyond premorbid and other childbirth-related factors; (3) peritraumatic dissociation is associated with PP-PTSD and other postpartum psychiatric symptoms; however, (4) when controlling for PP-PTSD symptoms, peritraumatic dissociation is associated with less psychiatric symptoms.
Methods
Participants and procedure
The current study is part of a larger project on psychological outcomes of childbirth (Dekel et al. under review). We recruited participants through announcements on postpartum websites (e.g., Postpartum Progress website) between November 2016 and April 2017. As the survey was in English, announcements were made on English-language postpartum websites. Inclusion criteria pertained to being at least 18 years old and having given birth to a live baby within the past 6 months. Participants were informed that they were implying consent by completing the anonymous online survey pertaining to their childbirth experience and mental health. The project met the Partners Human Research Committee’s (PHRC) criteria for exemption.
Measures
Peritraumatic dissociation
We assessed peritraumatic dissociation with the Peritraumatic Dissociative Experiences Questionnaire (PDEQ; Marmar et al. 1997). The PDEQ is a 10-item self-report measure assessing acute dissociative responses. Participants rated dissociative symptoms (e.g., “What was happening seemed unreal to me”) on a 5-point Likert scale, ranging from 1 (not at all true) to 5 (extremely true), with total scores ranging from 10 to 50. Scores of 16 or above are indicative of significant dissociative responses. We created three peritraumatic dissociation level groups (low, moderate, high) based on the 33.3rd and 66.6th percentiles of PDEQ scores. The PDEQ offers good psychometric properties (Birmes et al. 2005; Bui et al. 2011) and has previously been used to assess childbirth-related dissociation (Boudou et al. 2007; Choi and Seng 2016).
PP-PTSD symptoms
We assessed PP-PTSD symptoms using the PTSD Checklist for DSM-5 (PCL-5; Weathers et al. 2013b). The PCL-5 is a 20-item self-report measure assessing PTSD symptom frequency in accordance with DSM-5 criteria. Participants rated the frequency of PP-PTSD symptoms (e.g., “Repeated, disturbing, and unwanted memories of your childbirth experience?”) over the past month on a 5-point Likert scale, ranging from 0 (not at all) to 4 (extremely), with the index event anchored to “the most recent childbirth”. Total scores range from 0 to 80, with scores of 33 or above indicating clinically relevant symptom levels (Bovin et al. 2016). The PCL-5 has good psychometric properties (Blevins et al. 2015) and has previously been used to evaluate childbirth-related PTSD (e.g., Stramrood and Slade 2017).
Other psychiatric symptoms
We assessed frequency of psychiatric symptoms using the Brief Symptom Inventory (BSI; Derogatis 1993). The BSI is a 53-item self-report measure targeting various psychiatric symptoms. Participants rated symptom frequency (e.g., “Feeling hopeless about the future”) over the past week on a 5-point Likert scale, ranging from 0 (not at all) to 4 (extremely), resulting in a Global (symptom) Severity Index (GSI) and nine subscales (Somatization, Obsession-Compulsion, Interpersonal Sensitivity, Depression, Anxiety, Hostility, Phobic Anxiety, Paranoid Ideation, Psychoticism). The GSI represents the mean score of all 53 items and thus ranges from 0 to 4. The subscales are based on sum scores of specific items—Somatization consists of 7 items (subscale ranges from 0 to 28), Obsession-Compulsion, Depression, and Anxiety consist of 6 items (subscales range from 0 to 24), Hostility, Phobic Anxiety, Paranoid Ideation, and Psychoticism consist of 5 items (subscales range from 0 to 20), and Interpersonal Sensitivity consists of 4 items (subscale ranges from 0 to 16). Higher GSI and subscale scores represent higher symptom frequency. The BSI has good psychometric properties (Derogatis 1993) and has previously been used in postpartum samples (e.g., Ross et al. 2003).
Trauma history
We assessed trauma history using the Life Events Checklist for DSM-5 (LEC-5; Weathers et al. 2013a), a 17-item self-report measure of level of exposure to potentially traumatic events. It includes 16 pre-defined events and one “other event” of various levels of exposure on a 6-point nominal scale. The LEC-5 offers good psychometric properties (Gray et al. 2004).
Sociodemographics and childbirth-related information
We collected sociodemographic (i.e., age, education, mental health history, primiparity) and childbirth-related information (i.e., sleep deprivation, levels of pain, mode of delivery, labor and delivery complications, infant complications) via single items.
Statistical analysis
We examined potential impacts of missing data using Little’s Missing Completely At Random (MCAR) test. To test hypothesis (1), namely that levels of peritraumatic dissociation differ across modes of delivery, we used one-way analysis of variance (ANOVA). We tested hypothesis (2) pertaining to the association between peritraumatic dissociation during childbirth and psychiatric symptoms employing Pearson (partial) correlations. To test hypothesis (3) pertaining to the unique contribution of peritraumatic dissociation to PP-PTSD symptom levels above and beyond premorbid and other childbirth-related factors, we utilized multiple hierarchical regression. In the first step, we entered pre-childbirth variables including sociodemographics and mental health and trauma history. In the second step, we entered immediate childbirth variables pertaining to childbirth stressors and infant complications. In the third step, we entered peritraumatic dissociation. Finally, we conducted a multivariate analysis of covariance (MANCOVA) to test hypothesis (4), examining the difference between levels of peritraumatic dissociation on those psychiatric symptoms with significant Pearson partial correlations, controlling for PP-PTSD. To this end, we established three peritraumatic dissociation groups based on the 33.3rd and 66.6th percentiles of PDEQ scores. Data analysis was performed in IBM SPSS version 24.
Results
Missing data and instrument reliability
Out of 846 women who completed the survey, 94% met inclusion criteria (n = 795). We excluded 110 participants (14%) from the data set due to non-response on most measures, leaving a final sample of 685 women. Overall, 8.6% of data was missing. Little’s Missing Completely At Random (MCAR) test indicated missing completely at random, χ2(2654) = 1642.80, p = 1.00. We therefore used multiple imputation (Rubin 2009) to handle missing data.
PDEQ Reliability in the current study was high for the PDEQ (α = 0.91), PCL-5 (α = 0.95), and total BSI (α = 0.98) and acceptable for the BSI subscales (α between 0.77 for Psychoticism and 0.92 for Depression) and the LEC-5 (α = 0.86).
Demographics and descriptives
While slightly more than half of our sample (57%) indicated American or Puerto Rican nationality, 11% was European, 9% Canadian, 8% Australian/New Zealander, 7% Asian/Middle Eastern, 5% African, 2% held dual citizenships, and 1% was Latin American. While most women resided in North America (78% USA, 10% Canada), the remaining proportion of the sample indicated living in the UK (4%), Australia or New Zealand (3%), Europe (2%), Asia (1%), the Middle East (1%), and Africa (1%). Participants were between 18 and 47 years old (M = 31.37, SD = 4.80) and on average 3 months postpartum. The majority of women was married (93%), middle class (median household income = $50,000–$99,000), and held a higher education degree (71%). Slightly more than half (56%) was primiparous, and most delivered vaginally (64%) and at-term (90%, i.e., > 37 weeks of pregnancy). Around half of the sample indicated a trauma history (51%) and mental health issues prior to giving birth (43%). The majority of women reported sleep deprivation at the time of giving birth (67%), at least moderate degrees of pain during labor (76%) and delivery (51%), and slightly less than half reported obstetrical complications (47%).
PCL-5 scores ranged from 0 to 80 (M = 22.91, SD = 19.36) and close to a third (29%) of women endorsed clinically relevant levels of PP-PTSD symptoms (PCL-5 total score ≥ 33). PDEQ scores ranged from 10 to 50 (M = 20.45, SD = 9.89) and slightly more than half of women (57%) endorsed significant levels of peritraumatic dissociation (PDEQ total score ≥ 16). The relevant cut-off scores for the three PDEQ groups corresponded to PDEQ ≤ 14 (i.e., low PDEQ group with scores up to 33.3rd percentile), PDEQ > 14 and ≤ 23 (i.e., moderate PDEQ group with scores between 33.3rd and 66.6th percentiles), and PDEQ > 23 (i.e., high PDEQ group with scores higher than 66.6th percentile).
Women in the low PDEQ group were significantly older (M = 31.92, SD = 4.10) than those in the high (M = 30.69, SD = 4.65) PDEQ group, F(2,510) = 3.81, p = 0.02. The moderate PDEQ group did not differ from the other two groups regarding age (M = 31.09, SD = 5.07). Women in the low PDEQ group were more likely to have had at least some degree of higher education (98%) than women in the moderate (92%) and high (91%) PDEQ groups, X2(2, N = 653) = 9.58, p < 0.01. The groups also differed in regards to proportion of prior mental health issues (low PDEQ: 40%; moderate PDEQ: 39%; high PDEQ: 50%, X2 (2, N = 653) = 6.23, p = 0.04), primiparous mothers (low PDEQ: 44%; moderate PDEQ: 60%; high PDEQ: 67%, X2(2, N = 653) = 26.56, p < 0.001), sleep deprivation at time of birth (low PDEQ: 52%; moderate PDEQ: 72%; high PDEQ: 81%, X2(2, N = 653) = 45.26, p < 0.001), as well as obstetrical complications (low PDEQ: 30%; moderate PDEQ: 45%; high PDEQ: 72%, X2(2, N = 653) = 80.87, p < 0.001). There were no significant differences between the PDEQ groups regarding marital status and frequency of premature births.
Peritraumatic dissociation and mode of delivery
A one-way ANOVA with PDEQ scores as the dependent variable and mode of delivery as grouping factor revealed significant results, F(3,649) = 18.12, p < 0.001, ɳ2 = 0.08. Levels of peritraumatic dissociation were significantly higher among women who had undergone assisted vaginal deliveries and unscheduled Cesareans than among those with regular vaginal deliveries and scheduled Cesareans (see Table 1 for group means, standard deviations, and post hoc results).
Peritraumatic dissociation as a predictor of PP-PTSD
PDEQ scores were positively correlated with PCL-5 scores (Pearson r = 0.67, p < 0.001). We utilized hierarchical multiple regression to investigate the unique contribution of peritraumatic dissociation to PP-PTSD above and beyond premorbid and other childbirth-related factors. In the first step, we entered pre-childbirth variables including sociodemographics and mental health and trauma history. In the second step, we entered immediate childbirth variables pertaining to childbirth stressors and infant complications. In the third step, we entered peritraumatic dissociation. The variables accounted for 53% of the variance in PP-PTSD symptoms, F(12,567) = 53.43, p < 0.001. Education, mental health history, and primiparity explained 13% of the variance. The lower the level of education, having a mental health condition prior to childbirth, and being a first-time mother, the higher PP-PTSD symptoms reported. Regarding immediate childbirth factors, sleep deprivation, having an unscheduled Cesarean, childbirth complications, and pain during labor and delivery each had a significant contribution, explaining 16% of the variance. Finally, peritraumatic dissociation explained 24% of the variance in PP-PTSD symptoms, adding a significant contribution above and beyond premorbid and other childbirth-related factors (see Table 2).
Peritraumatic dissociation and psychiatric symptoms
PCL-5 scores were positively correlated with the GSI (Pearson r = 0.82, p < 0.001) and all BSI subscales (Pearson r between 0.52 for Hostility and 0.75 for Depression and Psychoticism, all p < 0.001). Higher levels of PP-PTSD symptoms were thus associated with higher psychiatric symptoms. Similarly, PDEQ scores were positively correlated with the GSI (Pearson r = 0.52, p < 0.001) and all BSI subscales (Pearson r between 0.27 for Hostility and 0.51 for Somatization and Obsession-Compulsion, all p < 0.001). Higher levels of peritraumatic dissociation were thus also associated with higher psychiatric symptoms.
When controlling for PCL-5 scores, however, PDEQ scores were negatively correlated with the GSI (Pearson r = − 0.10, p < 0.05), Depression (Pearson r = − 0.19, p < 0.001), Interpersonal Sensitivity (Pearson r = − 0.10, p < 0.05), Hostility (Pearson r = − 0.14, p < 0.01), and Psychoticism (Pearson r = − 0.13, p < 0.01). A MANCOVA including the aforementioned subscales as dependent variables, peritraumatic dissociation level groups as grouping factor, and PCL-5 scores as a covariate indicated a significant effect of peritraumatic dissociation group, F(12,790) = 2.62, p < 0.01, ɳ2p = 0.04. Partial eta-squared (ɳ2p) values of 0.01, 0.09, and 0.25 are interpreted to denote small, medium, and large effects, respectively. The high (n = 134) peritraumatic dissociation group showed significantly lower GSI, Depression, and Psychoticism than the low (n = 148) and moderate (n = 121) peritraumatic dissociation groups, lower Interpersonal Sensitivity than the moderate peritraumatic dissociation group, and lower Hostility than the low peritraumatic dissociation group, with small to medium effect sizes (see Table 3 and Fig. 1). Higher levels of peritraumatic dissociation were thus associated with lower levels of psychiatric symptoms when controlling for PP-PTSD symptoms.
Estimated marginal means of depression, interpersonal sensitivity, hostility, and psychoticism in levels of peritraumatic dissociation (PD). This figure illustrates significantly lower depression and psychoticism in the high PD group compared to the low and moderate PD groups (p < 0.01), lower interpersonal sensitivity in the high PD group compared to the moderate PD group (p < 0.01), and lower hostility in the high PD group compared to the low PD group (p < 0.01) when controlling for PP-PTSD. Low = PDEQ ≤ 14, n = 148; moderate = PDEQ > 14 and ≤ 23, n = 121; high = PDEQ > 23, n = 134
Discussion
We focused our investigation on the role of peritraumatic dissociation during childbirth in postpartum psychological adaptation. To this end, we examined peritraumatic dissociation across different modes of delivery and its contribution to the development of postpartum psychopathology. The main findings can be cataloged as follows: first, peritraumatic dissociation differed across modes of delivery, with higher levels linked to assisted vaginal deliveries and unscheduled Cesareans. Second, peritraumatic dissociation predicted childbirth-related posttraumatic stress symptoms above and beyond premorbid and other childbirth-related factors. Third, peritraumatic dissociation was associated with higher levels of psychiatric symptoms. However, when controlling for childbirth-related posttraumatic stress, higher levels of peritraumatic dissociation were associated with slightly lower levels of depression, interpersonal sensitivity, hostility, and psychoticism.
The finding of higher levels of peritraumatic dissociation reported after assisted vaginal deliveries and unscheduled Cesareans highlights the role of delivery environment (i.e., low stress versus high stress) rather than solely mode of delivery (i.e., vaginal versus Cesarean). Increased levels of peritraumatic dissociation in objectively amplified stressogenic childbirth environments support the notion of dissociation as a coping strategy to temporarily disconnect oneself from emotional and physical pain and distress in light of exposure to traumatic stressors (e.g., Spiegel 1991). Besides heightened stress levels, unscheduled C-sections and assisted vaginal deliveries may further share the features of unexpectedness and uncontrollability. Contemporary models of stress and coping highlight facing the “unknown” as an important situational feature. Future research should therefore set forth to identify the most stressful components of delivery environments by examining associated levels of expectedness and controllability.
Nonetheless, chronic use of dissociative mechanisms in coping with the traumatic event may lead to interference in processing and encoding of the traumatic memory, increasing the risk for subsequent postpartum posttraumatic stress (Briere et al. 2005; Koopman et al. 1994). Peritraumatic dissociation has previously been reported as one of the strongest predictors of PP-PTSD (Ayers et al. 2016) and PTSD related to other traumatic events (Ozer et al. 2003). Our finding of peritraumatic dissociation predicting childbirth-evoked PTSD symptoms above and beyond premorbid and other childbirth-related factors is in line with previous findings (Haagen et al. 2015; Lev-Wiesel and Daphna-Tekoah 2010; Olde et al. 2005) and highlights the notion that childbirth can be stressful enough to trigger dissociative and traumatic responses. Future studies utilizing prospective, longitudinal designs are warranted to explore the effects of chronic use of dissociative mechanisms in coping with highly stressogenic childbirth experiences.
Our findings pertaining to the relationship between peritraumatic dissociation and other postpartum psychiatric symptoms suggest that peritraumatic dissociation may be a protective mechanism, lending support to the conceptualization of peritraumatic dissociation as a “partially adaptive response to trauma” (Ladwig et al. 2002 p 41). Further, the findings are in line with the most common explanation for the unique link between peritraumatic dissociation and PTSD, namely that peritraumatic dissociation may interfere with the processing and encoding of the traumatic memory, increasing the risk for PTSD (Koopman et al. 1994; van der Kolk and van der Hart 1989), but not for depression and other psychiatric symptoms. Dissociation in light of exposure to a traumatic stressor may be an adaptive response, but may also present a risk factor for posttraumatic stress for some. While it should, however, be noted that the effect sizes for the negative associations between peritraumatic dissociation and psychiatric symptoms were small, the complex role of peritraumatic dissociation in psychological adaptation as potentially adaptive on the one hand, and maladaptive on the other, warrants future scientific attention.
Several limitations of the present study should be noted. While on average women’s PP-PTSD symptoms were assessed around 3 months postpartum, a time period in which PTSD symptoms become stable PP-PTSD, we only included a single time point. Retrospective self-report of peritraumatic dissociation may have been influenced by PP-PTSD symptom status. Further, the relationship between peritraumatic dissociation and PTSD symptoms may be stronger when using self-report measures as compared to interview methods (Ozer et al. 2003). Although we assessed PP-PTSD with a well-validated measure, we did not utilize a clinical assessment. Similarly, the different self-report measures utilized in the current study assess reported symptoms over differing time periods (i.e., PCL-5 “over the last month”, BSI “in the past week”). Although large in size, our sample was derived from a web survey raising the possibility of sample selection and severity-related reporting biases. Further, while the majority of our sample resided in North America, it comprised women with various nationalities. It should therefore be noted that there may be undetected cultural differences regarding the influence of expectations and demographic characteristics in coping with trauma and postpartum adaptation. Further, as the survey was in English and announcements were posted on English-language postpartum websites, women with English as a first language or the educational background to be fluent in English may be overrepresented in the current sample, limiting generalizability to non-English speaking women. Lastly, we did not collect information regarding receipt and quality of prenatal care, as well as mental and physical maternal health during pregnancy, or delivery place. Including these factors in future (longitudinal) studies will offer the opportunity to assess important aspects of pre- and perinatal stress and mental health, and to distinguish between the impacts of objectively and subjectively stressogenic birth experiences. Future research utilizing clinical assessments and prospective longitudinal designs to examine the nature of peritraumatic dissociation during birth and in postpartum mental health trajectories is warranted.
In summary, we document that childbirth can be associated with a dissociative response. We further highlight the role of delivery environments characterized by heightened levels of stress and unexpectedness in developing a stress response to childbirth. Screening women for dissociative responses to childbirth in routine care may offer a useful tool for identifying women at risk for childbirth-evoked PP-PTSD. On a broader level, investigation of PP-PTSD offers a prospective model to study PTSD immediately following exposure.
References
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, 5th edn. American Psychiatric Publishing, Arlington
Andersen LB, Melvaer LB, Videbech P, Lamont RF, Joergensen JS (2012) Risk factors for developing post-traumatic stress disorder following childbirth: a systematic review. Acta Obstet Gynecol Scand 91(11):1261–1272. https://doi.org/10.1111/j.1600-0412.2012.01476.x
Ayers S (2004) Delivery as a traumatic event: prevalence, risk factors, and treatment for postnatal posttraumatic stress disorder. Clin Obstet Gynecol 47(3):552–567
Ayers S, Bond R, Bertullies S, Wijma K (2016) The aetiology of post-traumatic stress following childbirth: a meta-analysis and theoretical framework. Psychol Med 46(6):1121–1134. https://doi.org/10.1017/S0033291715002706
Birmes P, Brunet A, Benoit M, Defer S, Hatton L, Sztulman H, Schmitt L (2005) Validation of the Peritraumatic dissociative experiences questionnaire self-report version in two samples of French-speaking individuals exposed to trauma. Eur Psychiatry 20(2):145–151. https://doi.org/10.1016/j.eurpsy.2004.06.033
Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL (2015) The posttraumatic stress disorder checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J Trauma Stress 28(6):489–498. https://doi.org/10.1002/jts.22059
Boudou M, Sejourne N, Chabrol H (2007) Childbirth pain, perinatal dissociation and perinatal distress as predictors of posttraumatic stress symptoms. Gynecol Obstet Fertil 35(11):1136–1142. https://doi.org/10.1016/j.gyobfe.2007.09.014
Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, Keane TM (2016) Psychometric properties of the PTSD checklist for diagnostic and statistical manual of mental disorders–fifth edition (PCL-5) in veterans. Psychol Assess 28(11):1379–1391. https://doi.org/10.1037/pas0000254
Briere J, Scott C, Weathers F (2005) Peritraumatic and persistent dissociation in the resumed etiology of PTSD. Am J Psychiatry 162(12):2295–2301. https://doi.org/10.1176/appi.ajp.162.12.2295
Bui E, Brunet A, Olliac B, Very E, Allenou C, Raynaud JP, Claudet I, Bourdet-Loubère S, Grandjean H, Schmitt L, Birmes P (2011) Validation of the Peritraumatic dissociative experiences questionnaire and Peritraumatic distress inventory in school-aged victims of road traffic accidents. Eur Psychiatry 26(2):108–111. https://doi.org/10.1016/j.eurpsy.2010.09.007
Choi KR, Seng JS (2016) Predisposing and precipitating factors for dissociation during labor in a cohort study of posttraumatic stress disorder and childbearing outcomes. J Midwifery Women's Health 61(1):68–76. https://doi.org/10.1111/jmwh.12364
Cook N, Ayers S, Horsch A (2018) Maternal posttraumatic stress disorder during the perinatal period and child outcomes: a systematic review. J Affect Disord 225:18–31. https://doi.org/10.1016/j.jad.2017.07.045
Dekel S, Stuebe C, Dishy G (2017) Childbirth induced posttraumatic stress syndrome: a systematic review of prevalence and risk factors. Front Psychol 8
Derogatis LR (1993) BSI brief symptom inventory: administration, scoring, and procedure manual, 4th edn. National Computer Systems, Minneapolis
Gray MJ, Litz BT, Hsu JL, Lombardo TW (2004) Psychometric properties of the life events checklist. Assess 11(4):330–341. https://doi.org/10.1177/1073191104269954
Haagen JG, Moerbeek M, Olde E, van der Hart O, Kleber RJ (2015) PTSD after childbirth: a predictive ethological model for symptom development. J Affect Disord 185:135–143. https://doi.org/10.1016/j.jad.2015.06.049
Koopman C, Classen C, Spiegel DA (1994) Predictors of posttraumatic stress symptoms among survivors of the Oakland/Berkeley, Calif., firestorm. Am J Psychiatry 151(6):888–894. https://doi.org/10.1176/ajp.151.6.888
Ladwig K, Marten-Mittag B, Deisenhofer I et al (2002) Psychophysiological correlates of peritraumatic dissociative responses in survivors of life-threatening cardiac events. Psychopathology 35(4):241–248. https://doi.org/10.1159/000063825
Lev-Wiesel R, Daphna-Tekoah S (2010) The role of peripartum dissociation as a predictor of posttraumatic stress symptoms following childbirth in Israeli Jewish women. J Trauma Dissociation 11(3):266–283. https://doi.org/10.1080/15299731003780887
Marcè LV (1858) Traité de la folie des femmes enceintes, des nouvelles accouchés et des nourrices, et des considerations medico-légales qui se rattachent à ce sujet [treatise on madness of pregnant women, with childbirth and nursing, and medicolegal considerations related to this subject]. Baillière et Fils, Paris
Marmar CR, Weiss DS, Metzler TJ (1997) The Peritraumatic dissociative experiences questionnaire. In: Wilson JP, Keane TM (eds) Assessing psychological trauma and PTSD. Guilford Press, New York, pp 412–428
McKenzie-McHarg K, Ayers S, Ford E, Horsch A, Jomeen J, Sawyer A, Stramrood C, Thomson G, Slade P (2015) Post-traumatic stress disorder following childbirth: an update of current issues and recommendations for future research. J Reprod Infant Psychol 33(3):219–237. https://doi.org/10.1080/02646838.2015.1031646
O'Hara MW, McCabe JE (2013) Postpartum depression: Current status and future directions. Annu Rev Clin Psychol 9:379–407. https://doi.org/10.1146/annurev-clinpsy-050212-185612
Olde E, van der Hart O, Kleber RJ, van Son MM, Wijnen HA, Pop VM (2005) Peritraumatic dissociation and emotions as predictors of PTSD symptoms following childbirth. J Trauma Dissociation 6(3):125–142. https://doi.org/10.1300/J229v06n03_06
Ozer EJ, Best SR, Lipsey TL, Weiss DS (2003) Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychol Bull 129(1):52–73. https://doi.org/10.1037/0033-2909.129.1.52
Punamäki R, Komproe IH, Qouta S, Elmasri M, de Jong JM (2005) The role of peritraumatic dissociation and gender in the association between trauma and mental health in a palestinian community sample. Am J Psychiatry 162(3):545–551. https://doi.org/10.1176/appi.ajp.162.3.545
Ross LE, Evans SG, Sellers EM, Romach MK (2003) Measurement issues in postpartum depression part 1: anxiety as a feature of postpartum depression. Arch Women's Ment Health 6(1):51–57. https://doi.org/10.1007/s00737-002-0155-1
Rubin DB (2009) Multiple imputation for nonresponse in surveys, vol 307. Wiley, Hoboken
Segre LS, O'Hara MW, Arndt S, Stuart S (2007) The prevalence of postpartum depression: the relative significance of three social status indices. Soc Psychiatry Psychiatr Epidemiol 42(4):316–321. https://doi.org/10.1007/s00127-007-0168-1
Spiegel D (1991) Dissociation and trauma. In: Tasman A, Goldfinger SM (eds) American psychiatric press review of psychiatry, vol 10. American Psychiatric Association, Arlington, pp 261–275
Stramrood C, Slade P (2017) A woman afraid of becoming pregnant again: posttraumatic stress disorder following childbirth. In: Paarlberg K, van de Wiel H (eds) Bio-psycho-social obstetrics and gynecology: a competency-oriented approach. Springer, Cham, pp 33–49. https://doi.org/10.1007/978-3-319-40404-2_2
Thiel F, Ein-Dor T, Dishy G, King A, Dekel S (2018) Examining symptom clusters of childbirth-related posttraumatic stress disorder. Prim Care Companion CNS Disord 20(5). https://doi.org/10.4088/PCC.18m02322
Van der Kolk BA, Van der Hart O (1989) Pierre Janet and the breakdown of adaptation in psychological trauma. Am J Psychiatry 146(12):1530–1540. https://doi.org/10.1176/ajp.146.12.1530
Vossbeck-Elsebusch AN, Freisfeld C, Ehring T (2014) Predictors of posttraumatic stress symptoms following childbirth. BMC Psychiatry 14
Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, Keane TM (2013a) The life events checklist for DSM-5 (lec-5). Scale available from the National Center for PTSD at www.ptsd.va.gov.
Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP (2013b) The ptsd checklist for DSM-5 (pcl-5). Scale available from the National Center for PTSD at www.ptsd.va.gov.
World Health Organization (2015) World health statistics 2015. Available at http://www.who.int/gho/publications/world_health_statistics/2015/en/
Yildiz PD, Ayers S, Phillips L (2017) The prevalence of posttraumatic stress disorder in pregnancy and after birth: a systematic review and meta-analysis. J Affect Disord 208:634–645. https://doi.org/10.1016/j.jad.2016.10.009
Acknowledgments
The authors would like to thank Ms. Shannon Henning for her generous support in initiating this research project. We also would like to thank Gabriella Dishy for developing the online survey.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Partners (Massachusetts General Hospital) Human Research Committee granted this study exemption.
Informed consent
This study entailed an anonymous online survey, no personal identifiable information was collected. Participants were informed that by agreeing to complete the study survey, they are implying their consent to participate in the study.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Thiel, F., Dekel, S. Peritraumatic dissociation in childbirth-evoked posttraumatic stress and postpartum mental health. Arch Womens Ment Health 23, 189–197 (2020). https://doi.org/10.1007/s00737-019-00978-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00737-019-00978-0