Abstract
The objective of the study was to evaluate the psychometric properties of the Edinburg Postnatal Depression Scale (EPDS) to detect depression during pregnancy in Chile. The EPDS was applied to a sample of 111 pregnant women, who were attending an antenatal appointment in primary care centers. The Beck Depression Inventory (BDI-I) was used to assess the convergent validity, and the Depressive Episode module of the MINI was used to identify cases. The factor analysis showed that there was a good fit, with a factor model that explains 57.6 % of the total variance. There was a high degree of internal consistency (Cronbach’s α = 0.914) and good convergent validity with the BDI-I (rho = 0.850, p < 0.001). The EPDS was capable of differentiating cases of depression from non-cases. The best cutoff point was between 12 and 13, corresponding to an overall accuracy of 87.4 %. The questionnaire has good psychometric properties and can be useful for detecting cases of depression during pregnancy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Depression is one of the most common and disabling psychiatric disorders (Murray and López 1996). Studies have consistently shown that, beginning in early adolescence, women have higher prevalence than men (Kessler et al. 1993), and that pregnancy does not protect against the emergence or persistence of the illness (Evans et al. 2001).
Available studies indicate that antepartum depression (AD) affects between 10 and 15 % of women (Josefsson et al. 2001; Stocky and Lynch 2000; Gavin et al. 2005) and represents a major predictor for postpartum depression across different ethnic groups (Liu and Tronick 2012).
Moreover, recent literature shows that AD is often underdiagnosed and undertreated (Vesga-López et al. 2008; Wisner et al. 2013). Thus, its detection and adequate treatment appear as a critical health issue deserving the attention of researchers, clinicians, and policymakers.
Untreated AD increases the risk for multiple adverse outcomes among women and their offspring. Suicide is responsible for about 20 % of postpartum deaths (Lindahl et al. 2005) and is the second most common cause of mortality in postpartum women (Lindahl et al. 2005). In turn, AD can have negative effects on pregnancy outcomes (Chung et al. 2001) and early child development and attachment (Murray 1992; Hayes et al. 2013), with consequences noted even in adolescence (Pawlby et al. 2009; O’Donnell et al. 2013).
Three Chilean studies have found that, if assessed at the symptoms’ level, about one third of Chilean women suffer from unspecific depressive and/or anxiety symptoms during midpregnancy (Millán et al. 1990; Jadresic et al. 1992; Alvarado et al. 1993). When standardized interviews and strict diagnostic and operational criteria for depression are employed, prevalence figures for AD range from 7.4 % (Jadresic et al. 1992) to 29 % (Alvarado et al. 1993), in middle- and lowerclass women, respectively.
In addition, Chilean research has shown that states of emotional distress (anxiety/depression) in pregnancy are associated with both low birth weight and preterm labor (Jadresic et al. 1993; Alvarado et al. 2002), and that they potentiate (through synergic interactions) the effects of other biomedical risk factors (Alvarado et al. 2000). As is the case in other countries, local investigators have determined that AD is a risk factor for postpartum depression (Jadresic et al. 1993; Alvarado et al. 2000).
The Edinburgh Postnatal Depression Scale (EPDS) is the most widely used screening tool for detection of depression during the postpartum period (Cox et al. 1987). However, it is increasingly being validated in pregnant women, and versions for prenatal use are currently available in at least ten different languages (Murray and Cox 1990; Areias et al. 1996; Adouard et al. 2005; Adewuya et al. 2006; Felice et al. 2006; Su et al. 2007; Wang et al. 2009; Tran et al. 2011; Rubertsson et al. 2011; Töreki et al. 2013). No validation studies have been conducted in Spanish-speaking populations during pregnancy.
Murray and Cox (1990) validated the EPDS, with a cutoff point of 14/15 for “probable depression.” This validation was carried out in women who were 28 to 34 weeks pregnant, using the Research Diagnostic Criteria for depressive illness obtained from Goldberg’s Standardized Psychiatric Interview.
Gibson et al. (2009) conducted a systematic review of studies validating the EPDS in antepartum and postpartum women, reporting heterogeneity among study findings, which may be due to differences in study methodology, language, and the diagnostic interview/criteria used.
The first two postnatal validation studies of Spanish-translated versions of the EPDS were carried out in Chile. Both studies, conducted by two independent groups, showed that the EPDS is a valid and useful screening instrument for the detection of postpartum depression in Chilean women (Alvarado et al. 1992; Jadresic et al. 1995). For the last two decades, the EPDS has been widely used for this purpose by Chilean health professionals and researchers (Rojas et al. 2006; Jadresic et al. 2007).
Hence, as the evidence suggests that the EPDS could prove a useful screening tool for AD, the need for validation studies of Spanish-translated version of the EPDS clearly emerges. Our aim was to carry out the first of such validations by studying the psychometric properties of one of the Chilean translations of the EPDS into Spanish (Jadresic et al. 1995).
Method
A research design combining techniques intended to establish both construct validity and criteria validity was employed (Cronbach 1998; Martínez Árias 1995).
A transversal type of study was carried out during November and December 2012. The sample consisted of pregnant women at least 18 years of age, with up to 28 weeks of gestation, attending their second antenatal consultation. The women were recruited from three primary care clinics, belonging to the public health sector, in Santiago, Chile.
A sample size of 100 women—ten cases per each item of the instrument being validated (Martínez Árias 1995)—was calculated. An additional 10 % (ten cases) were added to account for possible losses, resulting in a final estimated sample size of 110 women.
Cases of depressive illness were defined according to the DSM-IV (American Psychiatric Association 1994). The Major Depressive Episode Module of the Mini International Neuropsychiatric Interview (MINI), a short structured clinical interview which enables researchers to diagnose psychiatric disorders according to the DSM-IV or ICD-10, was used to derive the diagnostic criteria (Sheegan et al. 1998).
The Beck Depression Inventory, version I (BDI-I) (Beck et al. 1961, 1988; Beck and Steer 2000), was also applied to study convergent validity, by verifying whether the scores of both instruments move in a concurrent fashion.
Assessment of patients was undertaken by two psychologists, who were especially trained for the purpose of the study. This training included carrying out ten preliminary joint interviews aimed at achieving a good inter-rater reliability. Subsequently, the testing procedure was as follows: sociodemographic data were collected, self-report measures (EPDS, BDI-I) were applied, and a diagnosis was made. All interviews lasted 15 to 20 min. Data were analyzed using the Statistical Package for the Social Sciences (SPSS.15).
The study protocol and the informed consent form were approved by the Research Ethics Committee of the Faculty of Medicine of the University of Chile, in conformity with the principles embodied in the Declaration of Helsinki.
Results
Sample characteristics
The sample consisted of 111 pregnant women, attending their second antenatal consultation in three primary care clinics in Santiago, Chile (Table 1). There were no refusals to participate in the study. The age of the women ranged from 18 to 43 years. An asymmetric distribution was found, with participants tending to be younger women, with a median age of 25 years and an interquartile range from RI25 = 22 to RI75 = 30.
Of the interviewed group, 48 women (43.2 %) were bearing their first child, 37 (33.3 %) already had one child, 15 (13.5 %) had two children, and 11 (9.9 %) had 3 or 4 children.
Additionally, 89.2 % reported having a steady partner at the time of the assessment. Regarding marital status, 39.6 % were single, 21.6 % were married, and 38.7 % cohabited.
The median time of schooling was 12 years, with RI25 = 12 years and RI75 = 13 years, which means that most women had completed their secondary education (76.6 % of the sample had least finished secondary school). Thirty-seven women (33.3 %) had a stable job, 9 (8.1 %) had an unstable job, and more than half (52.3 %) had an unpaid jobs and/or were housewives. Seven women (6.3 %) reported having some other types of job.
Gestational age at the time of interview ranged from 8 to 28 weeks of pregnancy, with a median of 21 weeks and an interquartile range from RI25 = 15 weeks to RI75 = 25 weeks.
Item analysis, study of validity, and internal consistency
Analysis of the heterogeneity of the items
Responses for almost all items showed good variability: in nine out of the ten items, the alternative with the highest percentage fluctuated between 33.3 and 67.6 %. The only exemption was item 10—“The thought of harming myself has occurred to me”—for which 84.7 % of the women answered “never.”
Factor analysis
All indicators for verifying the model fit were strong: (1) the KMO test result was 0.917 (a KMO test result of 0.90 is excellent); (2) the p value for Bartlett’s test was <0.001; and (3) the values in the anti-image matrix for each of the items ranged from 0.873 to 0.946.
In the factor extraction, only one factor was obtained, explaining 57.6 % of the variance, which confirms the unifactorial structure of the EPDS. Subsequently, an equamax orthogonal rotation was carried out, whose results concerning factorial loads are shown in Table 2. All factorial loads were greater than 0.300, indicating a satisfactory correlation between the item and factor (in this case, the overall EPDS).
Internal consistency
Cronbach’s alpha (α) was used to determine the internal consistency. The α for the EPDS was 0.914, and the results for each item are shown in Table 3. As can be seen, all items exhibited a high correlation with the overall EPDS, and exclusion of any item did not improve the value of α. Therefore, the instrument can be concluded to have a good internal consistency.
Convergent validity
The objective of this analysis was to establish whether the EPDS scores moved in a similar direction to that observed in other questionnaire that measures the same construct. In this study, the BDI-I, widely used for measuring the severity of depressive symptoms was utilized.
Since the distribution of the scores was neither normal nor symmetrical, Spearman’s rank correlation test was employed. A rho value of 0.850 was found, with a p value for a one-tail test <0.001. This result indicates that there is a strong convergence between the scores of both questionnaires.
Description of the EPDS scores
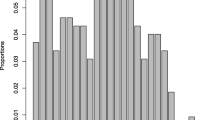
The EPDS scores varied from 0 to 27, with a mean of 9.7 and a standard deviation of 6.8. The median score was 8, with RI25 = 4 and RI75 = 15.
The EPDS scores followed a right-skewed distribution (Fig. 1), as was expected; it was predicted that only a minor percentage of the sample would present a depressive disorder (represented by a score high on the EPDS)
Predictive capacity of the test
To analyze the predictive capacity of the EPDS, the DSM-IV criteria for Major Depressive Episode, obtained through the MINI, was used as the “gold standard.” The utilization of the module showed that 38 mothers-to-be (34.2 %) had a major depressive disorder at the time of interview.
Pregnant women classified by the MINI as suffering from a depressive disorder exhibited significantly higher EPDS scores (16.3 ± 6.0) than non-depressed pregnant women (6.3 ± 4.3) (Mann-Whitney test, with p < 0.001). A similar situation was observed with the BDI-I scores, 22.6 ± 8.8 vs. 8.2 ± 5.3, for depressed and non-depressed women, respectively (Mann-Whitney test, p < 0.001). These findings confirm that the depression cases were appropriately classified and that they differ significantly from non-cases.
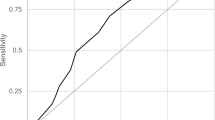
Table 4 shows the performance of the EPDS during pregnancy, from cutoff scores of 6/7 to 15/16, in terms of sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and overall accuracy.
The maximum overall accuracy was achieved with a cutoff point of 12/13, with 87.4 % of cases and non-cases being adequately classified. With this optimum case/non-case threshold score, a good combination of PPV and NPV was attained (85.3 and 88.3 %, respectively). A good overall accuracy is also reached with a cutoff point of 10/11 (86.5 %), but in this case, the PPV diminishes to less than 80 %.
Discussion
The value of the EPDS as a screening tool for depression in the postpartum period has been widely documented, for various decades (Cox et al. 1987; Gibson et al. 2009), even in Latin American countries such as Chile (Alvarado et al. 1992; Jadresic et al. 1995). Its use to identify depressive episodes in pregnancy is newer, but it has been well-documented in English-speaking countries (Murray and Cox 1990; Areias et al. 1996; Adouard et al. 2005; Adewuya et al. 2006; Felice et al. 2006; Su et al. 2007; Wang et al. 2009; Tran et al. 2011; Rubertsson et al. 2011; Töreki et al. 2013). To date, however, there are no publications about the use of the EPDS during pregnancy in Spanish-speaking countries; this is the first known study.
Studies have demonstrated the importance of treating depressive episodes during pregnancy, given their association with increased perinatal risk for both the child and mother (Murray 1992; Chung et al. 2001; Lindahl et al. 2005; Hayes et al. 2013) as well as a greater risk for presenting postpartum depression (Jadresic et al. 1993; Alvarado et al. 2000). The lack of specialized mental health resources in low- and middle-income countries (WHO 2005) puts more emphasis on increasing the diagnostic and treatment capacity of primary care teams. To this end, brief and easy to apply screening instruments, such as the EPDS, can be very useful.
The importance of studying the psychometric properties of instruments in different cultural contexts has been well recognized. In some cases, it is necessary to adjust some items or their structure, to optimize the assessment of latent values (Martínez Árias 1995). We followed a strategy much like the one used years before in Chile to validate the EPDS to detect postpartum depressive episodes, with a similar sample and procedures (Jadresic et al. 1995). Our results confirm that the instrument has good psychometric properties: good item variability; a unifactorial structure, which adequately explains the variability (57.6 %); a high degree of internal consistency (Cronbach’s α = 0,914); and a good convergent validity with the BDI-I (rho = 0.850). These results are in agreement with the findings of other studies (Gibson et al. 2009).
It is also relevant to highlight that the best cutoff point obtained (between 12 and 13) is similar to what was found in other studies, conducted outside of Chile (Murray and Cox 1990; Cox and Holden 1994; Su et al. 2007), and that it is higher than the recommended cutoff point for detecting postpartum depression in Chile (Alvarado et al. 1992; Jadresic et al. 1995). This was expected, due to the characteristics of pregnancy, in which some of the aspects evaluated by the screening test tend to be more frequently present than in the postpartum, especially toward the end of pregnancy (e.g., feeling scared more often, being more easily startled, feeling that normal chores are overwhelming, or having difficulty sleeping).
Although the study was carried out with a small sample of 111 pregnancy women, this sample size is sufficient to capture the variability of the items in a ten-question instrument (Martínez Árias 1995). One of the limitations of this study is that the sample consisted of women of medium and low socioeconomic status, so the results cannot be directly extrapolated to women of higher income. Another possible limitation is that the EPDS was applied by psychologists who were specially trained; when it is used in normal service conditions, the external validity could be reduced. However, given that the screening instrument was applied during routine prenatal appointments, in clinical settings typically used for these purposes, coupled with the fact that the EPDS is very short (about 5 min), we believe that this potential limitation is very minor and insignificant.
In conclusion, the EPDS is a useful, valid, and reliable instrument for the detection of depressive symptoms in pregnancy. It is easy to apply by health services staff, who carry out prenatal appointments, and it is a practical tool to reduce the risks associated with depression. We have shown the EPDS’ good performance in Chile, and we think that it might be equally useful in other low- and middle-income countries, by enhancing the response capacity of primary care teams.
References
Adewuya AO, Ola BA, Dada AO, Fasoto OO (2006) Validation of the Edinburgh postnatal depression scale as a screening tool for depression in late pregnancy among Nigerian women. J Psychosom Obstet Gynaecol 27(4):267–272
Adouard F, Glangeaud-Freudenthal NM, Golse B (2005) Validation of the Edinburgh postnatal depression scale (EPDS) in a sample of women with high-risk pregnancies in France. Arch Womens Ment Health 8(2):89–95
Alvarado R, Vera A, Rojas M, Olea E, Monardes E, Neves E (1992) La Escala de Edinburgo para la detección de cuadros depresivos en el postparto. Rev Psiquiatr 9(3–4):1177–1181
Alvarado R, Perucca E, Neves E, Rojas M, Monardes J, Olea E, Vera A (1993) Cuadros depresivos durante el embarazo y factores asociados. Rev Chil Obstet Ginecol 58(2):135–141
Alvarado R, Rojas M, Monardes J, Perucca E, Neves E, Olea E, Vera A (2000) Cuadros depresivos en el postparto en una cohorte de embarazadas: construcción de un modelo causal. Rev. Chil Neuropsiquiatr 38(2):84–93
Alvarado R, Medina E, Aranda W (2002) El efecto de variables psicosociales durante el embarazo en el peso y la edad gestacional del recién nacido. Rev Med Chil 130(5):561–568
American Psychiatric Association (1994) Diagnostic and statistical manual of mental disorders, 4th edn. American Psychiatric Press, Washington
Areias ME, Kumar R, Barros H, Figueiredo E (1996) Comparative incidence of depression in women and men, during pregnancy and after childbirth. Validation of the Edinburgh postnatal depression scale in Portuguese mothers. Br J Psychiatry 169(1):30–35
Beck AT, Steer RA (2000) Beck Depression Inventory (BDI). In: American Psychiatric Association (ed). Handbook of Psychiatric Measures. Washington DC, USA. Pp. 519–523
Beck AT, Ward CH, Mendelson M, Mock JE, Erbaugh J (1961) An inventory of measuring depression. Arch Gen Psychiatry 4:561–585
Beck AT, Steer RA, Gabin MG (1988) Psychometric properties of the Beck Depression Inventory: twenty-five years of evaluation. Clin Psychol Rev 8:78–100
Chung TK, Lau TK, Yip AS, Chiu HF, Lee DT (2001) Antepartum depressive symptomatology is associated with adverse obstretic and neonatal outcomes. Psychosom Med 63:830–4
Cox JL, Holden JM (1994) Perinatal psychiatry: use and misuse of the Edinburgh postnatal depression scale EPDS. Gaskell, London
Cox JL, Holden JM, Sagovsky R (1987) Detection of postnatal depression: development of a 10-item Edinburgh postnatal depression scale. Br J Psychiatry 150:782–786
Cronbach LJ (1998) Fundamentos de los test psicológicos. Ed. Biblioteca Nueva. España: Madrid
Evans J, Heron J, Francomb H, Oke S, Golding J (2001) Cohort study of depressed mood during pregnancy and after childbirth. BMJ 323(7307):257–260
Felice E, Saliba J, Grech V, Cox J (2006) Validation of the Maltese version of the Edinburgh postnatal depression scale. Arch Womens Mental Health 9(2):75–80
Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, Swinson T (2005) Perinatal depression: a systematic review of prevalence and incidence. Obstet Gynecol 106(5 Pt 1):1071–1083
Gibson J, McKenzie-McHarg K, Shakespeare J, Price J, Gray R (2009) A systematic review of studies validating the Edinburgh postnatal depression scale in antepartum and postpartum women. Acta Psychiatr Scand 119:350–356
Hayes LJ, Goodman SH, Carlson E (2013) Maternal antenatal depression and infant disorganized attachment at 12 months. Attach Hum Dev 15(2):133–153
Jadresic E, Jara C, Miranda M, Arrau B, Araya R (1992) Trastornos emocionales en el embarazo y el puerperio: estudio prospectivo de 108 mujeres. Rev Chil Neuropsiquiatr 30:99–106
Jadresic E, Jara C, Araya R (1993) Depresión en el embarazo y el puerperio: estudio de factores de riesgo. Acta Psiquiat Psicol. Am lat (1): 63–74
Jadresic E, Araya R, Jara C (1995) Validation of the Edinburgh postnatal depression scale (EPDS) in Chilean postpartum women. J Psychosom Obstet Gynecol 16:187–191
Jadresic E, Nguyen DN, Halbreich U (2007) Whay does Chilean research tell us about postpartum depression (PPD)? J Affect Disord 102:237–243
Josefsson A, Berg G, Nordon C, Sydsjo G (2001) Prevalence of depressive symptoms in late pregnancy and postpartum. Acta Obstet Gynecol Scand 80:251–255
Kessler RC, McGonagle KA, Swartz M, Blazer DG, Nelson CB (1993) Sex and depression in the national comorbidity survey. I: Lifetime prevalence, chronicity and recurrence. J Affect Disord 29(2–3):85–96
Lindahl V, Pearson JL, Colpe L (2005) Prevalence of suicidality during pregnancy and the postpartum. Arch Womens Ment Health 8(2):77–87
Liu CH, Tronick E (2012) Rates and predictors of postpartum depression by race and ethhnicity: results from the 2004 to 2007 New York City PRAMS Survey (Pregnancy Risk Assessment Monitoring System). Matern Child Health J; Oct 25
Martínez Árias R (1995) Psicometría: Teoría de los test psicológicos y educativos. Ed. Síntesis. España: Madrid
Millán T, Yévenez R, Gálvez M, Bahamonde MI (1990) Encuesta sobre síntomas de depresión en embarazadas de un consultorio urbano de atención primaria. Rev Méd Chil 118:1230–1234
Murray L (1992) The impact of postnatal depression on infant development. J Child Psychol Psychiatry 33(3):543–561
Murray D, Cox J (1990) Screening for depression during pregnancy with the Edinburgh depression scale (EPDS). J Reprod Infant Psychol 8:99–107
Murray CJ, López DA (1996) Evidence-based health policy—lessons from the global burden of disease study. Science 274(5228):740–743
O’Donnell KJ, Glover V, Jenkins J, Browne D, Ben-Shlomo Y, Golding J, O’Connor TG (2013) Prenatal maternal mood is associated with altered diurnal cortisol in adolescence. Psychoneuroendocrinology. doi:10.1016/j.psyneuen.2013.01.008
Pawlby S, Hay DF, Sharp D, Waters CS, O’Keane V (2009) Antenatal depression predicts depression in adolescent offspring: prospective longitudinal community-based study. J Affect Disord 113(3):236–243
Rojas G, Fritsch R, Solis J, Jadresic E, Castillo C, Gonzalez M, Guajardo V, Lewis G, Peters TJ, Araya R (2006) Treating postnatal depression among low-income mothers in primary care in Santiago, Chile: a randomised controlled trial. Lancet 370:1629–1637
Rubertsson C, Börjesson K, Berglund A, Josefsson A, Sydsjö (2011) The Swedish validation of the Edinburgh postnatal depression scale (EPDS) during pregnancy. Nord J Psychiatry 65(6):414–418
Sheegan DV et al (1998) The Mini-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnosis psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 59(suppl 20):22–33
Stocky A, Lynch J (2000) Acute psychiatric disturbance in pregnancy and the puerperium. Baillieres Best Pract Res Clin Obstet Gynaecol 14(1):73–87
Su KP, Chiu TH, Huang CL, Ho M, Lee CC, Wu PL, Lin CY, Liau CH, Liao CC, Chiu WC, Pariante CM (2007) Different cutoff points for different trimesters? The use of Edinburgh postnatal depression scale and beck depression inventory to screen for depression in pregnant Taiwanese women. Gen Hosp Psychiatry 29(5):436–441
Töreki A, Andó B, Keresztúri A, Sikovanyecz J, Dudas RB, Janka Z, Kozinszky Z, Pál A (2013) The Edinburgh postnatal depression scale: translation and antepartum validation for a Hungarian simple. Midwifery 29(4):308–315
Tran TD, Tran T, La B, Lee D, Rosenthal D, Fisher J (2011) Screening for perinatal common mental disorders in women in the north of Vietnam: a comparison of three psychometric instruments. J Affect Disord 133(1–2):281–293
Vesga-López O, Blanco C, Keyes K, Olfson M, Grant BF, Hasin DS (2008) Psychiatric disorders in pregnant and postpartum women in the United States. Arch Gen Psychiatry 65(7):805–815
Wang Y, Guo X, Lau Y, Chan KS, Yin L, Chen J (2009) Psychometric evaluation of the mainland Chinese version of the Edinburgh postnatal depression scale. Int J Nurs Stud 46(6):813–823
Wisner KL, Sit DK, McShea MC, Rizzo DM, Zoretich RA, Hughes CL, Eng HF, Luther JF, Wisniewski SR, Costantino ML, Confer AL, Moses-Kolko EL, Famy CS, Hanusa BH (2013) Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. JAMA Psychiatry 70(5):490–498
World Health Organization (2005) Mental health atlas. WHO, Geneva
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Alvarado, R., Jadresic, E., Guajardo, V. et al. First validation of a Spanish-translated version of the Edinburgh postnatal depression scale (EPDS) for use in pregnant women. A Chilean study. Arch Womens Ment Health 18, 607–612 (2015). https://doi.org/10.1007/s00737-014-0466-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00737-014-0466-z