Abstract
Objectives The Edinburgh Postnatal Depression Scale (EPDS) was originally created as a uni-dimensional scale to screen for postpartum depression (PPD); however, evidence from various studies suggests that it is a multi-dimensional scale measuring mainly anxiety in addition to depression. The factor structure of the EPDS seems to differ across various language translations, raising questions regarding its stability. This study examined the factor structure of the Hebrew version of the EPDS to assess whether it is uni- or multi-dimensional. Methods Seven hundred and fifteen (n = 715) women were screened at 6 weeks postpartum using the Hebrew version of the EPDS. Confirmatory factor analysis (CFA) was used to test four models derived from the literature. Results Of the four CFA models tested, a 9-item two factor model fit the data best, with one factor representing an underlying depression construct and the other representing an underlying anxiety construct. Conclusions for Practice The Hebrew version of the EPDS appears to consist of depression and anxiety sub-scales. Given the widespread PPD screening initiatives, anxiety symptoms should be addressed in addition to depressive symptoms, and a short scale, such as the EPDS, assessing both may be efficient.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Significance
What is already known on this subject? The EPDS is the most commonly used scale around the world to screen for PPD. Factor structure analyses of the EPDS-English version show that the EPDS includes an anxiety sub-scale as well as a depression subscale. The EPDS seems to screen for anxiety in addition to depression.
What this study adds? This is the first Confirmatory Factor Analysis of the EPDS-Hebrew version, and its main finding is that the EPDS-Hebrew version seems to consist of anxiety and depression sub-scales. This is also the first study to systematically compare and highlight the differences between the factor structures of the English and non-English versions of the EPDS.
Introduction
The postpartum period is associated with a range of emotional difficulties; however the focus of attention is commonly given to postpartum depression (PPD), whether as a specific depressive disorder or as an overarching phrase encompassing various emotional disorders [5, 32]. In the past few years growing attention has been given to distinguishing PPD from other postpartum emotional disorders, with special attention given to anxiety that appears in the postpartum period [31]. Postpartum anxiety (PPA) is often comorbid with depression but in many cases appears as an independent condition, at times more prevalent than depression and at least as disruptive for women and their infants [5, 29].
The Edinburgh Postnatal Depression Scale (EPDS: [11]) is the most widely used scale for assessing depression in the perinatal period in research as well as in clinical practice and public health programs [23, 25]; it has been translated and validated in many languages, including Hebrew [21]. Although the EPDS was developed as a uni-dimensional scale for assessing depression [11], a number of studies have examined its factor structure and suggested that it measures other factors as well, mainly anxiety [25]. As discussed below, the factor structure of the EPDS may vary across cultures and languages. Therefore, it is important to examine the factor structure of translated versions of the EPDS and the purpose of this study was to highlight the difference between the factor structures of the English and non-English versions of the EPDS and to examine the factor structure of the Hebrew version of the EPDS.
Studies Examining the Factor Structure of the EPDS
Several studies have explored the factor structure of the EPDS. Although conclusions vary, the majority suggest that the EPDS consists of two or three subscales [27]. The studies have been conducted in various settings around the world and the results appear to differ between studies examining the English version and studies examining other language versions of the EPDS. Studies that examined the factor structure of the original English language version of the EPDS (see Table 1) found that the EPDS consists of one sub-scale measuring depression and another sub-scale measuring anxiety [24, 27, 35], with a possible third sub-scale for anhedonia [23, 37] or suicide [19, 20, 31]. Interestingly, the studies that found that the EPDS consists of two factors were carried out in Australia, whereas studies carried out in the U.S., Canada, and the United Kingdom found that the EPDS consists of three factors.
It appears that the emerging leading approach regarding the EPDS English version is that items 3, 4, and 5 of the EPDS constitute an anxiety sub-scale (termed EPDS-3A), and a number of researchers recommend that scores for the depression and anxiety sub-scales of the EPDS be calculated separately [19, 24, 27, 35, 37]. In addition to examining the factor structure of the EPDS, further work has been done to validate the anxiety sub-scale against diagnostic criteria, with two studies concluding that the EPDS-3A can be used to screen for anxiety, providing optimal cut-off scores indicative of anxiety symptoms of 4 or above [27] or 6 or above [24]. Matthey et al. [25], in a review of studies that examined the performance of the EPDS at detecting women with anxiety disorder diagnoses, found that women with only an anxiety disorder scored significantly higher on the total EPDS than women with no diagnosis; and women with only depression scored significantly higher on the total EPDS than women with only anxiety. Reinforcement for the claim to use the anxiety sub-scale to screen for anxiety comes from the Matthey [24] study where the researcher found that women who scored high on the anxiety sub-scale (EPDS-3A) scored low on the depression sub-scale and relatively low on the total EPDS, indicating that if anxiety was not assessed using the EPDS-3A these women would not have been detected as needing further assessment or treatment.
Although there have been several studies examining the factor structure of the English language EPDS, most of these studies have methodological limitations. For example, four of the studies used principal components analysis (PCA; [24, 31, 35, 37]). Although PCA is often used as a form of exploratory factor analysis (EFA) it may produce different results than EFA using other extraction methods, such as principal factors (PF) or weighted least squares (WLS). However, “PCA is more appropriately used as a data reduction technique; … EFA is more appropriate (than PCA) if the stated objective is to reproduce the intercorrelations of a set of indicators with a small number of latent dimensions, recognizing the existence of measurement error in the observed measures” [7]. Among the studies that used EFA or confirmatory factor analysis (CFA), three had small sample sizes ([19], n = 101; [20], n = 117; and [23], n = 169). Although there are various recommendations about acceptable sample sizes for CFA, sample sizes of at least 200 are generally recommended for this analysis [22]. Only one of the English language EPDS studies, conducted by Phillips et al. [27], used EFA and CFA and had a sufficiently large sample size for these analyses (n = 309). However, Phillips et al. used the same sample for both their EFA and CFA, which limits the conclusions that can be drawn from their analysis.
Studies that explored the factor structure of other language versions of the EPDS (see Table 2) had inconsistent findings. Most found that the EPDS consists of two or three subscales; however the sub-scales were somewhat different than the subscales identified in the EPDS English version studies. All identified a “depression” sub-scale. However some also identified an anxiety sub-scale [6, 9, 26, 28, 30] whereas others identified the other sub-scales as “despair,” “loss of enjoyment” [34], or “depression and other disorders, including anxiety” [1]. In addition, although some found a three factor (depression, anxiety, and anhedonia) model similar to Tuohy and McVey’s [37] English language model, the items that loaded on the three factors were not consistent with those found by Touhy and Mcvey [9, 30]. Finally, there is no consistency across the studies regarding the items that loaded on the anxiety sub-scale. Some found that this sub-scale consists of items 3, 4, and 5, similar to the English version studies [6, 28, 30], items 3, 4, and 5 along with other items [9]; and one study found that the anxiety sub-scale consists of entirely other items [26].
Similar to the studies using the English language EPDS, many of the studies of translated versions of the EPDS also had methodological limitations. Four of the studies [4, 6, 17, 26] used PCA instead of EFA or CFA. Several of the studies had small sample sizes for the analyses conducted; Adouard et al. [1] did not specify the type of factor analysis conducted, but the sample size (n = 60) was small for any form of factor analysis. Small et al. [34] examined three translated versions of the EPDS, Vietnamese, Turkish, and Tagalog (Filipino) using EFA, but the sample sizes for each group were small (n = 103, 104, and 106, respectively). Similarly, Chabrol and Teissedre [9] had a relatively large sample of 299 women, however splitting the sample to conduct both EFA and CFA resulted in a small sample for each. Only two of the studies had sufficient sample sizes for CFA ([28], n = 293; [30], n = 811 for EFA and CFA).
Although there seems to be consistency in the studies of the English EPDS version factor structure concluding that the EPDS consists of an anxiety sub-scale comprised of items 3, 4, and 5, more work is warranted to validate this sub-scale and to understand the entire factor structure of the EPDS. In addition, there seems to be instability in the factor structure of the EPDS across various language versions and more work is warranted to understand its factor structure for translated versions of the measure. This is especially important considering the extensive use of the EPDS as a screening measure. For example, the EPDS is administered as standard care in Israel in all mother-and-child (“Drop of Milk”) centersFootnote 1 to women 4–8 weeks postpartum (Israel Ministry of Health, Circular Notice 20/12, 2012), and is administered widely in many other places and settings, whether clinical or research-oriented, around the world (Matthey, 2013). Factor stability of the EPDS across cultures is important in the context of potentially using the EPDS sub-scales to distinguish between depression and anxiety symptoms of perinatal women [18, 20]. Assessing the factor structure of the EPDS is therefore crucial for future research, assessment, and provision of tailored optimal treatment for women with postpartum mood disorders [23, 35]. The factor structure of the EPDS Hebrew version has not been examined previously; however, based on the Hebrew version validation study, which found that some women who scored high on the EPDS had a main diagnosis of anxiety and not depression [21], it seems likely that the Hebrew version may assess anxiety in addition to depression. The aim of this study was therefore to examine the factor structure of the EPDS Hebrew version using confirmatory factor analysis (CFA).
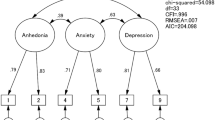
Because no prior factor structure studies of the Hebrew version of the EPDS were found, the extensive prior research using both the English language and translated versions of the EPDS was considered in developing the confirmatory factor analyses for this study. Based on the original purpose of the EPDS to be used as a uni-dimensional scale [11], a one factor EPDS model including all 10 items on a depression factor was tested. Considering the methodological limitations of prior research, studies using EFA and/or CFA with a sample size of at least 200 were used to develop the two factor models used in this study. Specifically, based on the work of Phillips et al. [27], a two factor EPDS model including factors for depression (items 1, 2, 6, 7, 8, 9, and 10) and anxiety (items 3, 4, and 5) was tested; an alternative two factor model without item 6 was also examined based on the work of Pop et al. [28], who found that item 6 (“Things have been getting on top of me”) crossloaded on both the anxiety and depression factors. Finally, based on the work of Reichenheim et al. [30], a three factor model was tested with factors for anhedonia (items 1, 2, and 6), anxiety (items 3, 4, and 5), and depression (items 7, 8, 9, and 10).
Methods
Participants
Participants included 969 women who were recruited from the maternity department at a large hospital in Jerusalem, Israel between June 2008 and February 2009. Women were eligible to participate if they were 18 years of age and above, Jewish, gave birth to a live baby without major medical illnesses, were one to 2 days postpartum, and completed questionnaires in Hebrew. Of the 969 women who were initially recruited, 715 (74 %) participated at a 6-week postpartum screening using the EPDS Hebrew version. This paper focuses on these 715 EPDS Hebrew version assessments at 6 weeks postpartum.
Procedures
The University Institutional Review Board and the Hospital’s Helsinki committee approvals were obtained prior to carrying out the study protocol. At one to 2 days postpartum women signed an informed consent form, filled out a demographic questionnaire, and were asked to leave their contact information for the purpose of screening for depressive symptoms at 6 weeks postpartum. Participation was confidential, but not anonymous in order for the researcher to track respondents for the PPD screening. This was all explained in the initial recruitment meeting during the informed consent process. At 6 weeks postpartum all women were contacted by telephone, were reminded that they agreed to participate in the study, and were asked if they agreed to be screened for PPD. Only those who agreed were screened using the Edinburgh Postnatal Depression Scale (EPDS) Hebrew version. Women who screened positive for PPD (EPDS total scores > = 9) were told that they had PPD symptoms and may have PPD. They also received an explanation of what PPD is and were referred for treatment.
Measures
The Edinburgh Postnatal Depression Scale
Presence and severity of PPD symptoms were measured by the Edinburgh Postnatal Depression Scale (EPDS; [11]) during the 6 week screening. The EPDS is a self-report scale consisting of 10 short statements, each followed by four possible responses in a Likert scale format ranging from low severity of the symptom (scored 0) to high severity of the symptom (scored 3). Women chose the responses that best described the way they had been feeling during the past 7 days. Scores on all 10 statements are summed after reverse coding items 1, 2 (which are positively stated) and 4 (which has an inversed answer format ranging from high severity to low severity of the symptom), resulting in a possible score of 0–30, with higher scores reflecting greater symptom severity. A cut-off score of 9 was used in this study, reflecting at least a mild case of depressive symptoms [10, 15]. Cronbach’s alpha for the EPDS in this study was .76.
The EPDS was translated into Hebrew by Glasser and Barell [16] using a translation-back translation method, which was repeated by two different people in order to ensure common language usage. The Hebrew version scores were then validated by Kandel-Katznelson et al. [21] by comparing EPDS scores to the Structured Clinical Interview for DSM disorders (SCID) scores at 1–3.5 months postpartum. With a cut-off score of 9, the EPDS sensitivity was 92.3 % and specificity was 72.5 %.
Demographic Background
Demographic data were collected during the initial phase of the study (1–2 days postpartum). These data included participant age, number of children, marital status (coded as ‘married’, ‘single’, ‘widowed’, and ‘divorced’), and level of income (coded as ‘below average income’ [equivalent to an annual income below $26,000 US], and ‘average income or above’ [equivalent to an annual income of $26,001 and above].
Data Analysis
Confirmatory factor analyses of the Hebrew version of the EPDS were conducted using Mplus 7.11. Because EPDS responses were on four-point Likert type scales, data were treated as ordered categorical and, as recommended by Byrne [8], the WLSMV estimator was used; the assumptions for the analysis were adequately met. As recommended by Brown [7] and Kline [22], multiple indices were examined to assess model fit. Brown [7] suggests reporting the root mean square error of approximation (RMSEA), the comparative fit index (CFI), and the Tucker-Lewis fit index (TLI), with RMSEA < .06, CFI > .95, and TLI > .95 indicating reasonably good fit. Significant factor loadings of .55 and greater are considered good [36] and were interpreted.
Results
The mean age of participants was 29.37 years (SD = 5.33, range 18–45 years); the vast majority of them were married (98.7 %), with 3.35 children on average (SD = 2.29, range 1–13 children). In addition, 41.5 % of participants had an average income or above and 58.5 % had a below average income. Eighty of the women who participated at the 6-week postpartum screening (11 %) screened positive for PPD symptoms. Analyses (t tests and χ 2) performed in order to detect significant differences on age, number of children, marital status and level of income between those who participated at the 6 week postpartum screening (Group I) and those who did not (drop-outs; Group II) indicated that women in Group I were significantly older (M = 29.37, SD = 5.34 for Group I; M = 28.09, SD = 5.36 for Group II; t = 3.25, p = .001), on average had more children (M = 3.35, SD = 2.29 for Group I; M = 3.01, SD = 2.26 for Group II; t = 2.00, p = .04) and a higher level of income (44.8 % of Group I participants had an average income or above while 32.4 % of Group II participants had an average income or above; χ 2 = 10.483, p = .001) than women in Group II.
Of the four CFA models tested, the 9-item two factor model, with items 1, 2, 7, 8, 9, and 10 loading on the depression factor and items 3, 4, and 5 loading on the anxiety factor, fit the data the best (see Table 3 for fit indices and Table 4 for standardized factor loadings for each model tested). Overall, fit indices for the 9-item two factor model suggest this model has adequate fit to the data (RMSEA = .068, CFI = .95, TLI = .931). Discriminant validity for the depression and anxiety factors was adequate with a moderate significant correlation between the anxiety and depression factors (r = .67, p < .001), providing further support for the 9-item two factor model. “A factor correlation that equals or exceeds .85 is often used as the cut-off criterion for problematic discriminant validity” [7]; in this case the correlation of .67 suggests reasonable discriminant validity for the depression and anxiety factors.
Several of the fit indices indicate adequate fit of the 9-item two factor model; however, the significant Chi square (χ2 = 112.912, df = 26, p < .001) suggests a possible problem in model fit. Although the Chi square test may be overly sensitive in large samples (such as that in the current study), as suggested by Kline [22] correlation residuals with absolute values >.10 were examined (p. 202). In the current study, six residual correlations exceed an absolute value of .10: items 1 and 2 (.178), items 1 and 10 (−.311), items 2 and 9 (−.128), items 3 and 4 (−.111), items 3 and 8 (.148), and items 3 and 10 (.290). Negative correlation residuals indicate the model over predicts the association between the variables and positive correlation residuals indicate the model under predicts the association between the variables. The three negative residual correlations occur between pairs of items on the same factors (pair 1 and 10 and pair 2 and 9 on the depression factor and pair 3 and 4 on the anxiety factor), suggesting the model over predicts the strength of association between some pairs of variables within each factor. One of the three positive residual correlations is for an item pair (1 and 2) where the two items are both on the depression factor and the other two positive residual correlations are for item pairs across the two factors; all three positive residual correlations suggest the model under predicts the association between these pairs of items. Consistent with this pattern, the modification indices for this model suggest adding several error covariances. However, because error covariances tend to be sample specific and the model fits adequately without further modification, error covariances were not added to the model. In summary, the 9-item two factor model fits well, but item 10 may be problematic as demonstrated by the two large residual correlations involving this item.
Discussion
The current study confirmed the multi-dimensional factor structure of the EPDS, similar to findings in most previous studies. Our finding that the EPDS measures anxiety as well as depression is consistent with several other studies (e.g., [6, 24, 27, 28]. The EPDS was developed based on clinicians’ experiences with postpartum women and the EPDS scores were validated against other depression scales [11], but not anxiety scales. Because depression is often comorbid with anxiety symptoms [14], it may be that women in the initial EPDS validation studies experienced undetected anxiety alongside depression.
Consistent with the study by Pop et al. [28], findings in the current study support a 9-item two factor—depression and anxiety—model for the Hebrew version of the EPDS. The 9-item two factor model fits better than the 10-item two factor model, suggesting that item 6 does not fit well with the depression factor in the current study. Further, in both the 9-item and 10-item two factor models, the depression and anxiety factors were significantly correlated, suggesting that dropping item 6 from the two factor model does not change the relationship between the depression and anxiety factors. Although conducted more than 20 years ago, the Pop et al. study is one of the few prior studies to conduct CFA with a sample size over 200, using a translated version of the EPDS. It is unclear why the Pop et al. factor structure was not reported in the later CFA work on the EPDS (see Tables 1, 2 for factor structures tested in each study). However, consistent with the Pop et al. model, several other studies did not include item 6 in their final factor structures [6, 20, 23, 31, 37], further suggesting that this item may not fit well with the other items on the EPDS.
The three factor model fit the data reasonably well in the current study (although not quite as well as the 9-item two factor model). However, the anhedonia factor correlates significantly with both the depression (r = .84, p < .005) and anxiety (r = .58, p < .005) factors. The high correlation between the depression and anhedonia factors suggests limited discriminant validity in the three factor model; therefore, separate factors for anhedonia and depression are not supported in this study. This finding is consistent with Jomeen and Martin’s [20] study in which the researchers examined Chabrol and Teissedre’s [9] 3 factor model (“depression”, “anxiety” and “anhedonia”) and found that it did not fit the data well.
Further work is needed for item 10 (“The thought of harming myself has occurred to me”) because the two largest residual correlations involve this item (with items 1 and 3) and several previous studies (i.e., [6, 19, 20, 31, 34—Vietnamese sample only]) suggest that this item may represent a separate construct of suicide. However, because these studies were based on principal components analysis and/or were conducted with small samples, and—most importantly—did not identify a consistent set of items for the depression and anxiety factors (see Tables 1, 2), a three factor model with item 10 on its own third factor was not tested in the current study.
The difference between the several proposed EPDS factor structures appears to stem from the various language versions of the EPDS under examination and not from differences in the perinatal period in which women were assessed, as suggested previously by Phillips et al. [27]. Our finding of an anxiety sub-scale consisting of items 3, 4, and 5 is consistent with all EPDS English version studies [19, 20, 23, 24, 27, 31, 35, 37] and several of the EPDS non-English version studies [6, 28, 30]. However, most of the non-English version studies did not find that items 3, 4, and 5 load on a separate anxiety factor [1, 4, 9, 17, 26, 34], and therefore more work is needed in examining the factor structure of the translated versions of the EDPS. One should bear in mind that women in different cultures may differ in their experience of postpartum mood disorders as well as in the meanings they give to their experience [2, 10] and this may be the reason for the variations in the factor structures that were found in the EPDS non-English factor structure studies. Further validation of the Hebrew anxiety sub-scale is needed to support the current study finding of an anxiety sub-scale.
Limitations
Although the current study has a number of strengths, mainly that it was carried out with a large sample and that this is the first study that examined the factor structure of the EPDS-Hebrew version, like any study, there are several limitations that should be considered. First, preliminary analysis revealed that women who participated at the 6-week postpartum screening were statistically significantly older, on average had more children and a higher level of income than those who did not participate at the 6-week postpartum screening (drop-outs), a finding that may pose a limitation to the representativeness of the findings. However, this difference of 1 year in age, .3 in number of children and the difference in level of income may not be meaningful in practice, taking into account that the age of participants ranged from 18 to 45, number of children ranged from 1 to 13 and over half of participants in both groups had a lower-then-average income, and the study had sufficient power to detect small differences. Second, data are not available to test the concurrent or predictive validity of the anxiety and depression subscale scores. Third, findings suggest that item 10 needs further examination.
Finally, Cronbach’s alpha was .71 for the six item depression subscale and .60 for the three item anxiety subscale. The alpha for the six item depression scale is smaller than that found for the full 10 item EPDS (α = .76), but both meet DeVaus’ [12] level of .7 to “indicate a reliable set of items” (p. 20). Although the alpha for the three item anxiety subscale does not meet the guideline for a reliable set of items, alpha is related to the number of items, with smaller numbers of items yielding smaller alphas [33]. Moreover, Chronbach’s alpha for the full 10 item EPDS found in the current study is quite similar to Chronbach’s alphas found in some other studies on translated versions of the EPDS (e.g., α = .76 in Adouard et al. [1] and in Guedeney and Fermanian [17]; .77 in Montazeri et al. [26]; and .80 in Pop et al. [28] and in Brouwers et al. [6]). Also, the alphas of the various subscales found in some of these studies ranged from .53 to .85, with most under .74 (Adouard et al. [1], Guedeney and Fermanian [17], and Pop et al. [28]), fairly close to those found in the current study.
Implications
Consistent with other studies, the current study suggests that the Hebrew version of the EPDS consists of two subscales, one measuring depression and the other anxiety. Considering the extensive use of the EPDS in clinical postnatal settings with a focus on screening for depression [23] and based on the known comorbidity of depression and anxiety, the high prevalence of PPA [2, 5], and the negative consequences of PPA [29], those who screen postpartum women should be aware of the multidimensionality of the EPDS and assess women for anxiety along with depression in order to provide treatment tailored to a woman’s specific assessment and diagnosis. Based on the preliminary validation of the anxiety and depression EPDS subscale cutoff scores identified by Matthey [24] and Phillips et al. [27], clinicians in postnatal settings can assess women for separate depressive and anxiety symptoms using this one short screening tool. In view of the similar findings of this study to the other English version studies regarding the anxiety subscale, we cautiously suggest that those who screen women using the EPDS Hebrew version can use the cutoff scores suggested by Matthey [24] and Phillips et al. [27]; however further work validating the Hebrew version subscales and cutoff scores should be done.
Taking into account that the EPDS total score may indicate presence of anxiety in addition to or in the absence of depression and that women with a total high score on the anxiety sub-scale (EPDS-3A) may score relatively low on the total EPDS, it may be that if anxiety is not assessed using the EPDS-3A these women may not be detected. Considering that the EPDS is a screening tool and that after initial screening women should be referred for clinical diagnosis and appropriate treatment [24] it is important that the screening process be done in a way that will detect women’s actual symptoms and encourage them to follow up with referrals, especially considering the fact that many women do not follow up with these referrals [3]. Some evidence shows that women who experience PPA are less likely to turn to professional help than those experiencing PPD, which may be attributed to increased attention given to PPD in national public campaigns leading women to feel more comfortable discussing PPD than PPA [38]; therefore if the screening process focuses only on depression and if a women is told that she has symptoms of depression but feels anxious and not depressed, she may very likely not follow up with a referral for further evaluation and treatment. It therefore seems likely that if both depression and anxiety are assessed and addressed together it may help increase women’s sense of comfort to discuss their feelings of anxiety and may eventually increase treatment rates.
In the context of the Israeli population, these results are of great importance due to the universal postpartum screening using the EPDS that began in 2013 in all Mother-and-Child centers in Israel. Public health nurses who screen women in these settings are required to carry out an initial supportive intervention before deciding on an appropriate referral, if needed. It is therefore important that these nurses be aware of the likelihood that the EPDS assesses anxiety in addition to depressive symptoms in order to be able to address the specific distress a woman is suffering from and to make an appropriate referral.
Conclusion
Being the first study to systematically compare and highlight the differences between the factor structures of the English and non-English versions of the EPDS, it is recommended that further work be done in order to examine the factor structure of the non-English versions of the EPDS in order to assess stability of the EPDS factor structure, taking into consideration the variations in cultural meanings of PPD and PPA. Screening women for postpartum emotional distress has been shown to be a first step in enhancing treatment rates [13] and is therefore of value; however if one does not want to burden screeners and women and wants to make sure women are adequately screened, a short assessment that addresses both depressive and anxiety symptoms may be of value. The current findings suggest that the EPDS may be an efficient tool for anxiety and depression screening.
Notes
These centers provide all vaccination and well child visits from birth to 6 years old.
References
Adouard, F., Glangeaud-Freudenthal, N. M. C., & Golse, B. (2005). Validation of the Edinburgh Postnatal Depression Scale (EPDS) in a sample of women with high-risk pregnancies in France. Archives of Womens Mental Health, 8, 89–95.
Andajani-Sutjahjo, S., Manderson, L., & Astbury, J. (2007). Complex emotions, complex problems: Understanding the experiences of perinatal depression among new mothers in urban Indonesia. Culture, Medicine and Psychiatry, 31, 101–122.
Andrews Horowitz, J., & Cousins, A. (2006). Postpartum depression treatment rates for at-risk women. Nursing Research, 55(2S), s23–s27.
Berle, J. O., Aarre, T. F., Mykletun, A., Dahl, A. A., & Holsten, F. (2003). Screening for postnatal depression: Validation of the Norwegian version of the Edinburgh Postnatal Depression Scale, and assessment of risk factors for postnatal depression. Journal of Affective Disorders, 76, 151–156.
Brockington, I. F., Macdonald, E., & Wainscott, G. (2006). Anxiety, obsessions and morbid preoccupations in pregnancy and the puerperium. Archives of Womens Mental Health, 9, 253–263.
Brouwers, E. P. M., Van Baar, A. L., & Pop, V. J. M. (2001). Does the Edinburgh Postnatal Depression Scale measure anxiety? Journal of Psychosomatic Research, 51, 659–663.
Brown, T. A. (2015). Confirmatory factor analysis for applied research (2nd ed.). New York: The Guilford Press.
Byrne, B. M. (2012). Structural equation modeling with Mplus. New York: Routledge.
Chabrol, H., & Teissedre, F. (2004). Relation between Edinburgh Postnatal Depression Scale scores at 2–3 days and 4–6 weeks postpartum. Journal of Reproductive and Infant Psychology, 22(1), 33–39.
Cox, J. L., & Holden, J. (2003). Perinatal mental health: A guide to the Edinburgh Postnatal Depression Scale. London: Gaskell.
Cox, J. L., Holden, J. M., & Sagovsky, R. (1987). Detection of postnatal depression: Development of the 10-item Edinburgh Postnatal Depression Scale. British Journal of Psychiatry, 150, 782–786.
DeVaus, D. (2002). Analyzing social science data: 50 key problems in data analysis. Thousand Oaks: Sage.
Earls, M. F. (2010). Incorporating recognition and management of perinatal and postpartum depression into pediatric practice. Pediatrics, 126, 1032.
Farr, S. L., Dietz, P. M., O’Hara, M. W., Burley, K., & Ko, J. Y. (2014). Postpartum anxiety and comorbid depression in a population-based sample of women. Journal of Women’s Health, 23(2), 120–128.
Gibson, J., McKenzie-McHarg, K., Shakespeare, J., Price, J., & Gray, R. (2009). A systematic review of studies validating the Edinburgh Postnatal Depression Scale in antepartum and postpartum women. Acta Psychiatrica Scandinavica, 119(5), 350–364.
Glasser, S., & Barell, V. (1999). Depression scale for research in and identification of postpartum depression. Harefuah, 136, 764–768. [Hebrew].
Guedeney, N., & Fermanian, J. (1998). Validation study of the French version of the Edinburgh Postnatal Depression Scale (EPDS): New results about use and psychometric properties. European Psychiatry, 13, 83–89.
Ip, W. Y., & Martin, C. R. (2007). The factor structure of the Chinese version of the Edinburgh Postnatal Depression Scale (EPDS). Journal of Reproductive and Infant Psychology, 25, 83–86.
Jomeen, J., & Martin, C. R. (2005). Confirmation of an occluded anxiety component within the Edinburgh Postnatal Depression Scale (EPDS) during early pregnancy. Journal of Reproductive and Infant Psychology, 23, 143–154.
Jomeen, J., & Martin, C. R. (2007). Replicability and stability of the multidimensional model of the Edinburgh Postnatal Depression Scale in late pregnancy. Journal of Psychiatric and Mental Health Nursing, 14, 319–324.
Kandel-Katznelson S, Maisel S, Zilber N, Lerner J. (2000) Validation of the Hebrew translation of the Edinburgh postnatal depression scale: Background, methods and findings. Tenth Annual Conference of the Israeli Psychiatric Association, Jerusalem, Israel [Hebrew].
Kline, R. B. (2011). Principles and practice of structural equation modeling (3rd ed.). New York: The Guilford Press.
Lee King, P. A. (2012). Replicability of structural models of the Edinburgh Postnatal Depression Scale (EPDS) in a community sample of postpartum African American women with low socioeconomic status. Archives of Womens Mental Health, 15, 77–86.
Matthey, S. (2008). Using the Edinburgh Postnatal Depression Scale to screen for anxiety disorders. Depression and Anxiety, 25, 926–931.
Matthey, S., Fisher, J., & Rowe, H. (2013). Using the Edinburgh Postnatal Depression Scale to screen for anxiety disorders: Conceptual and methodological considerations. Journal of Affective Disorders, 146, 224–230.
Montazeri, A., Torkan, B., & Omidvari, S. (2007). The Edinburgh Postnatal Depression Scale (EPDS): Translation and validation study of the Iranian version. BMC Psychiatry, 7, 11.
Phillips, J., Charles, M., Sharpe, L., & Matthey, S. (2009). Validation of the subscales of the Edinburgh Postnatal Depression Scale in a sample of women with unsettled infants. Journal of Affective Disorders, 118, 101–112.
Pop, V. J., Komproe, I. H., & Van Son, M. J. (1992). Characteristics of the Edinburgh Post Natal Depression Scale in the Netherlands. Journal of Affective Disorders, 26, 105–110.
Reck, C., Müller, M., Tietz, A., & Möhler, E. (2013). Infant distress to novelty is associated with maternal anxiety disorder and especially with maternal avoidance behavior. Journal of Anxiety Disorders, 27, 404–412.
Reichenheim, M. E., Moraes, C. L., Oliveira, A. S. D., & Lobato, G. (2011). Revisiting the dimensional structure of the Edinburgh Postnatal Depression Scale (EPDS): Empirical evidence for a general factor. BMC Medical Research Methodology, 11, 93.
Ross, L. E., Gilbert Evans, S. E., Sellers, E. M., & Romach, M. K. (2003). Measurement issues in postpartum depression part 1: Anxiety as a feature of postpartum depression. Archives of Womens Mental Health, 6, 51–57.
Rowe, H. J., Fisher, J. R. W., & Loh, W. M. (2008). The Edinburgh Postnatal Depression Scale detects but does not distinguish anxiety disorders from depression in mothers of infants. Archives of Womens Mental Health, 11, 103–108.
Sijtsma, K. (2009). On the use, the misuse, and the very limited usefulness of Cronbach’s alpha. Psychometrika, 74, 107–120.
Small, R., Lumley, J., Yelland, J., & Brown, S. (2007). The performance of the Edinburgh Postnatal Depression Scale in English speaking and non-English speaking populations in Australia. Social Psychiatry Psychiatric Epidemiology, 42, 70–78.
Swalm, D., Brooks, J., Doherty, D., Nathan, E., & Jacques, A. (2010). Using the Edinburgh Postnatal Depression Scale to screen for perinatal anxiety. Archives of Womens Mental Health, 13, 515–522.
Tabachnick, B. G., & Fidell, L. S. (2007). Using multivariate statistics (5th ed.). New York, NY: Pearson.
Tuohy, A., & McVey, C. (2008). Subscales measuring symptoms of non-specific depression, anhedonia, and anxiety in the Edinburgh Postnatal Depression Scale. British Journal of Clinical Psychology, 47, 153–169.
Woolhouse, H., Brown, S., Krastev, A., Perlen, S., & Gunn, J. (2009). Seeking help for anxiety and depression after childbirth: Results of the Maternal Health Study. Archives of Womens Mental Health, 12, 75–83.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Bina, R., Harrington, D. The Edinburgh Postnatal Depression Scale: Screening Tool for Postpartum Anxiety as Well? Findings from a Confirmatory Factor Analysis of the Hebrew Version. Matern Child Health J 20, 904–914 (2016). https://doi.org/10.1007/s10995-015-1879-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-015-1879-7