Abstract
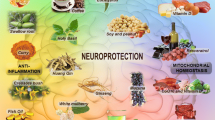
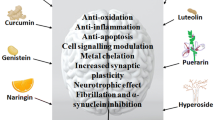
Parkinson’s disease is characterized by typical motor symptoms, loss of dopamine neurons in the substantia nigra, and accumulation of Lewy body composed of mutated α-synuclein. However, now it is considered as a generalized disease with multiple pathological features. Present available treatments can ameliorate symptoms at least for a while, but only a few therapies could delay progressive neurodegeneration of dopamine neurons. Lewy body accumulates in peripheral tissues many years before motor dysfunction becomes manifest, suggesting that disease-modifying therapy should start earlier during the premotor stage. Long-termed regulation of lifestyle, diet and supplement of nutraceuticals may be possible ways for the disease-modification. Diet can reduce the incidence of Parkinson’s disease and phytochemicals, major bioactive ingredients of herbs and plant food, modulate multiple pathogenic factors and exert neuroprotective effects in preclinical studies. This review presents mechanisms underlying neuroprotection of phytochemicals against neuronal cell death and α-synuclein toxicity in Parkinson’s disease. Phytochemicals are antioxidants, maintain mitochondrial function and homeostasis, prevent intrinsic apoptosis and neuroinflammation, activate cellular signal pathways to induce anti-apoptotic and pro-survival genes, such as Bcl-2 protein family and neurotrophic factors, and promote cleavage of damaged mitochondria and α-synuclein aggregates. Phytochemicals prevent α-synuclein oligomerization and aggregation, and dissolve preformed α-synuclein aggregates. Novel neuroprotective agents are expected to develop based on the scaffold of phytochemicals permeable across the blood–brain–barrier, to increase the bioavailability, ameliorate brain dysfunction and prevent neurodegeneration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In our aging society, the increase of patients with age-associated neurodegenerative diseases, such as Alzheimer’s (AD) and Parkinson’s disease (PD), is the most oppressive issue for medical care, society and economy. PD is characterized by typical motor symptoms and cognition decline. The etiology of PD remains to be clarified, and aging, genetic susceptibility and environmental factors have been proposed as the risk factors. There are typical pathological features; progressive and irreversible loss of dopamine (DA) neurons in the substantia nigra (SN) pars compacta and accumulation of Lewy bodies and neurites composed of α-synuclein (αSyn). The pathogenic factors include oxidative stress, mitochondrial dysfunction, deficits of neurotrophic factors (NTFs), inflammation, dysfunction of the ubiquitin–proteasome system (UPS) and autophagy-lysosome pathway (ALP) and activation of apoptosis. PD was once considered as a disease manifesting the motor triad of bradykinesia, rigidity and tremor caused by DA deficiency, but is now considered as a generalized disease involved in central, peripheral and enteric nervous systems. At the advanced stage, neuronal death is detected also in noradrenergic, serotonergic, cholinergic and GABAergic neurons, and patients with PD present depression, dementia, insomnia and dysphagia, along with impaired bladder and gastrointestinal tract, algesia and visual hallucination. The therapy for PD has been mainly aimed to replace DA deficiency with L-DOPA, DA agonists and inhibitors of monoamine oxidase (MAO). However, the present available therapies neither prevent the disease progression, nor control non-dopaminergic features of PD, such as falling, freezing and cognition decline. Now, “disease-modifying therapy” is proposed to protect dopaminergic and other neurons to slow the disease progression (Olanow et al. 2017).
Braak et al. proposed advancing stages of PD based on progress of Lewy pathology (Braak et al. 2003). In the early stage, gastrointestinal problems, such as dysphagia, nausea, constipation and olfactory problems, and the presence of Lewy bodies in the neurons of olfactory tract and enteric nerve system are detected. Neurodegeneration of PD begins in the dorsal motor nucleus of the vagus nerve and advances upwards through the medulla oblongata, pontine tegmentum, midbrain, basal forebrain and the cerebral cortex. The lesions progress to the SN, and typical motor symptom becomes manifest at a later stage of the disease. Preclinical phase with subclinical motor and non-motor symptoms may span 20 or more years. These results indicate that disease-modifying therapy should start in the prodromal stage presenting non-motor syndromes, such as olfactory loss, constipation, anxiety disorders, rapid eye movement sleep behavior disorder (Fereshtehnejad et al. 2019).
Quite a wide range of compounds have been proposed as neuroprotective agents in PD: inhibitors of type B MAO (MAO-B) (selegiline, rasagiline), antioxidants (vitamin E, C, ω-3 fatty acids, melatonin, metal chelators), bioenergetic compounds (coenzyme Q10, creatine), NTFs and anti-inflammatory compounds (lipoic acid, minocycline) (Espay et al. 2017; Naoi et al. 2020). Delayed-start trial of rasagiline presented modulation of disease progression, but most clinical trials did not (Olanow et al. 2009). Epidemiological and clinical intervention studies present that PD incidence is reduced by dietary habit, such as Mediterranean diet and ketogenic diet composed of low carbohydrate and fat-rich diet (Barichella et al. 2017). Foods reported to suppress PD progression are fresh vegetables, fruit, herbs, nuts and seeds, no-fried fish, olive oil, wine and spices. Diet habits modify mitochondrial function, maintain nutritional state, optimize L-DOPA therapy and minimize the motor complication. In randomized, placebo-controlled trials (RPCTs), vitamin E, carotenoids, ω-3 fatty acids and vitamin E improved clinical status of PD patients (Yang et al. 2017a). To data, however, clinical studies could not fully prove the prevention of disease progression by nutraceuticals.
Phytochemicals, plant secondary metabolites, are major bioactive ingredients of neuroprotective foods and herbs proposed as “herbal medicine” (Zanforlin et al. 2017). Bioactive phytochemicals have pleiotropic functions, modulate multiple pathogenic pathways and exert the neuroprotective effects in animal and cellular models of PD. The main ingredients, flavonoids, stilbenes, phenylpropanoids and terpenes, are present in high quantities in vegetables, fruits, tea, red wine and chocolate, and have potent antioxidant function by direct scavenge of reactive oxygen and nitrogen species (ROS, RNS) and activation of antioxidant enzymes.
This review presents effects of phytochemicals on the pathogenic factors of PD and the targets include oxidative stress, mitochondrial dysfunction and apoptosis, and αSyn aggregation and toxicity for modulation of disease progression (Naoi et al. 2017, 2019). Preclinical studies of phytochemicals present beneficial neuroprotective effects, but clinical trials have only scarcely presented convincing results on disease modification. Improvement of the bioactivity, stability and effective permeability through the blood–brain-barrier (BBB) of phytochemicals is discussed to develop novel compounds for disease-modifying therapy of PD.
Phytochemicals: structure and neuroprotective functions
Phytochemicals have diverse bioactivities, such as antioxidant, anti-apoptotic, anti-aging, anti-carcinogenic, anti-microbial and anti-inflammatory functions. Polyphenols are the major bioactive species of phytochemicals and contain one or more aromatic rings with hydroxyl groups as substituents. They include flavonoids, alkaloids, terpenes, terpenoids, saponins, sapogenins, β-carboline and isoquinoline alkaloids. The chemical structures of major phytochemicals are shown in Figs. 1 and 2.
More than 9000 flavonoids are found in fruits, vegetables, cereals and tea, and several hundred in human diet. They are proposed as potential therapeutic agents against oxidative stress-associated diseases. Flavonoids are further divided into subgroups: flavonols [found in broccoli, onion, kale, fruits (citrus, apples, cherries, berries), ginkgo, hibiscus, St John’s wort], flavanols (green tea, red wine, chocolate, Uncaria rhychophylai), flavanones (citrus fruits, tomatoes), flavones (apple skin, parsley, celery, chamomile, passionflower, ginkgo), isoflavones (soybeans, legumes, pomegranate) and anthocyanidins (red wine, cherries, grapes, berry fruits). They share the common chemical structure: two benzene rings joined by three-carbon chain and a carbon skeleton of diphenyl propanes. The most common flavones and flavonols contain dihydroxyl residues in the 3′ and 4′ positions of the B ring and mono-hydroxyl at 4′. The 3 position is most common glycosylation site. The B-ring of bioflavonoids is substituted at the 3 position, whereas, that of other flavonoids at the 2 position. Flavonoids have antioxidant, metal chelating, neuroprotective, anti-carcinogenic, anti-inflammatory, immune-stimulating and estrogenic effects.
Epigallocatechin-3-gallate (EGCG) is the major flavanol of green tea and the most biologically active compound in vitro and in vivo. EGCG can pass the BBB and exhibits multiple neuroprotective effects, such as anti-amyloidogenic potencies and activation of signally pathways to induce glial cell line-derived and brain-derived neurotrophic factor (GDNF, BDNF). In RPCTs, EGCG improved cognitive function in the aged, control and patients with mild cognitive impairment (MCI), and young adults with Down’s syndrome (Wightman et al. 2012). Isoflavones exert estrogenic or anti-estrogenic effects and are used as an alternative therapy for breast and prostate cancer, cardiovascular disease and menopausal symptoms. In a large prospective study, greater consumption of anthocyanidin-rich foods, such as berries, was associated with lower PD risk during 20–22 years of follow-up (Gao et al. 2012). Flavonoid intake prevented reduction of white matter hyperintensities volume, MRI marker of AD related dementia (Shishtar et al. 2020).
Non-flavonoid phytochemicals are neuroprotective and chemical structures of major polyphenols are shown in Fig. 2. Curcumin [1,7-bis(4-hydrox-3-methoxy-phenyl)-1,6-heptdiene-3,5-dione] is isolated from Curcuma longa (turmeric) as the yellow pigment. It is composed of an aliphatic unsaturated heptene linker with two benzene rings attached at both ends of two ferulic acids, each of which has a hydroxy and a methoxy group attached symmetrically. Curcumin crosses the BBB, activates the nuclear factor erythroid 2-related factor 2 (Nrf2) signaling to improve antioxidant status, suppresses glial reaction and increases anti-inflammatory activity. Curcumin has anti- and pro-oxidant properties and exerts anti-cancer, anti-diabetic, anti-microbial and anticoagulant activities. In clinical trials, curcumin showed beneficial effects in cognitive decline and depression (Lopresti et al. 2014; Rainey-Smith et al. 2016), but the positive results have not been presented in PD.
Phenolic acids are isolated from grain ban, whole grain, orange, tomato, carrot, borage and some medical herbs like Ligusticum chuangxion and the bioavailability depends on the hydrolysis by the degradation enzymes in intestinal tissues and gut microbiota. Phenolic acids are classified into benzoic acid derivatives with C6–C1 structure and cinnamic acid derivatives with C6–C3 structure. Cinnamic acids are intermediates in the biosynthesis of polyphenols from phenylalanine. Ferulic, p-coumaric, gallic, rosmarinic (caffeic-3,4-dihydroxphenyl lactic ester) and protocatechuic acid permeate the BBB, have antioxidant, anti-inflammatory, neuroprotective, antidepressant-like and anticancer activities, and protect DA neurons in cellular and animal models of PD. Gallic acid is found in blueberry, strawberry, mango, plums, walnut and hazelnuts. Gallic acid and the ester metabolites (n-propyl, n-methyl-, n-octyl gallate) have been shown as the most promising stable neuroprotective ingredients (Kurachi et al. 2012).
Resveratrol (trans-3,5,4′-trihydroxystilbene) is found in red grapes (Vitis vinifera L.), mulberries, red cherries, grape and peanuts and has been proposed as natural medicine and dietary supplement. The therapeutic potency is evident from “the French paradox”, low incidence of cardiovascular disease among red wine drinkers. Resveratrol is composed of two phenol rings connected through a styrene double bond. Resveratrol regulates protein kinase C (PKC) signal pathways, enhances antioxidant system and modulates inflammatory responses, decreases amyloid β (Aβ) level by enhancing the UPS activity, and mitigates aging-related neurodegeneration, carcinogenesis and atherosclerosis. Resveratrol crosses the BBB, exerts neuroprotection in similar way as “the caloric restriction” by activation of AMP-activated protein kinase (AMPK)/Sirt 1 (silent information regulator of transcription, a NAD-dependent deacetylase) pathway (Bastianetto et al. 2015; Sarubbo et al. 2018). In clinical studies, resveratrol improved cognitive function in the aged and post-menopausal women (Witte et al. 2014), but the trial for Parkinsonian patients has not been reported.
Astaxanthin (3,3′-dihydroxy-β,β′-carotene-4,4′-dione), a lipophilic xanthophyll carotenoid, occurs in microalgae Haematococcus pluvialis, krill, trout, crayfish and salmon, and has potent antioxidant, anti-inflammatory and anti-apoptotic actions. Its linear, polar-nonpolar-polar structure allows to be inserted into membrane, cross the BBB, and scavenge ROS within the hydrophobic interior and hydrophilic boundaries. Astaxanthin suppressed oxidative stress and protected MPP+-treated PC12 cells. It is associated with prevention of cardiovascular disease and cataract. Astaxanthin alone or with tocotrienol or sesamin intake improved cognitive function in the healthy aged and patients with mild cognition insufficient (MCI) in a RPCT (Sekikawa et al. 2020).
Extract of Ginkgo biloba contains terpene trilactones (ginkgolides A, B, C and bilobalide) and flavonoid (quercetin, kaempferol, isoharmnetin) glycosides, which can permeate the BBB and function as neuroprotective compounds in the brain. Ginkgo biloba extract, EGb 761, is the most commonly used herb preparation with cognition-enhancing properties, stabilizes mitochondrial membrane and prevents apoptosis in ischemia and aging (Maclennan et al. 2002). Ginkgolides A and B are antioxidants, enhance Bcl-2 expression, activate pro-survival PKC, extracellular signal-regulated kinase 1/2 (ERK1/2), and phosphoinositide 3-kinase (PI3K)/Akt pathways, and inhibit microglia activation and c-Jun-N-terminal kinase (JNK) signaling pathway in animal and cellular models of PD. In RPCTs, EGb 761 improved cognitive impairment and neuropsychiatric symptoms in subjects with MCI (Gavrilova et al. 2014).
Ginsenosides are the main bioactive ingredients of ginseng (Panax ginseng Meyer), a popular traditional Chinese medicine used for thousands of years in China, Japan, and Korea. Ginsenosides have commonly four-ring hydrophobic structure and are classified into two groups, protopanaxadiols and protopamaxatriols, according to binding sites of sugar moieties to tripeptide at 3- or 6-position. Ginsenosides have diverse pharmacological activities: antioxidant, anti-aging, anti-apoptosis, anti-inflammation, neurotransmitter balance, neuroprotection, and mitochondrial stabilization (Huang et al. 2019). Ginseng are used for treatment of age-related neurodegeneration, depression, diabetes, hypertension, inflammatory diseases and cancer. In animal models of PD prepared by carbon tetrachloride, MPTP, MPP+ and β-sitosterol β-D-glucoside, ginseng extract G115, ginsenoside Rb1, Rd, and Rg1, Re and a pseudoginsenoside F11 protected dopaminergic cells (Ahmed et al. 2016). Rb1 activated estrogen receptors, induced Bcl-2, BDNF and GDNF expression and exerted anti-apoptotic effects.
Pathogenic factors targeted by neuroprotective phytochemicals in Parkinson’s disease
Multiple pathogenic factors, such as oxidative stress, dysfunction of mitochondria and protein degradation system, downregulated expression of pro-survival genes and neuroinflammation, synergistically cause PD. Mitochondria play a central role in PD pathogenesis. Among 23 genes linked with monogenic PD forms, 14 genes are associated with functions and quality control of mitochondria, suggesting that mitochondria-targeted therapy may serve as potent disease-modification (Billingsley et al. 2019).
Oxidative stress and impaired mitochondrial function in Parkinson’s disease
Oxidative stress is a pivotal risk factor for neuronal loss in PD. ROS and RNS cause mitochondrial dysfunction, impair cellular energy metabolism and activate apoptosis machinery. In Parkinsonian brain, increased markers for oxidation of DNA [8-hydroxy-2-deoxyguanine (8-OHdG)], lipid [4-hydroxy-2-nonenal (4-HNE), lipid hydroperoxide] and protein [protein carbonyls, 3-nitro-tyrosine (3-NT)], and reduction of antioxidants, such as urate and glutathione (GSH), are commonly detected. DA itself contributes neurodegeneration of DA neurons in the SN. MAO localized at the outer mitochondrial membrane oxidizes DA into 3,4-dihydroxyphenylacetaldehyde (DOPAL) and produces hydrogen peroxide (H2O2), which is converted further into more toxic hydroxyl radical (–OH) in the presence of iron by the Fenton reaction. DOPAL is more reactive than DA, and DOPAL and its quinone promote oligomerization αSyn and the formed quinone-adduct impairs synaptic function (Jinsmaa et al. 2020). DA is also non-enzymatically oxidized into toxic DA-ortho-quinone producing superoxide radical (O2−−). Accumulation of DA-quinone reduces enzymatic activity of glucocerebrosidase (GCase), impairs lysosomal function and enhances αSyn accumulation (Burbulla et al. 2017). In the cytoplasm, DA-quinone produces aminochrome and finally neuromelanin, which is associated with loss of DA neurons.
In PD, mitochondrial dysfunction is another pathogenic factor (Trinh et al. 2021). Even under physiological condition, electron is leaked from complexes I and III of the electron transport chain (ETC), and generated O2− dismutates into H2O2, and diffuses into the cytosol. Postmortem studies of Parkinsonian brains presented a systematic deficiency of complex I, complex III and mitochondrial glycerol-3-phosphate dehydrogenase in the SN, platelets and skeletal muscle. The point mutations or depletion of mitochondrial DNA (mtDNA) increases in mitochondria of Parkinsonian DA neurons. Environmental factors [pesticides (rotenone), industrial solvent (trichloroethane)], endogenous isoquinoline toxins and mutations of mtDNA and nuclear DNA downregulate complex I and IV activities (Henchcliffe and Beal 2008). However, complex I reduction is modest (~ 20–30%) in most cases with sporadic PD and only about 30% of PD patients have a clear complex I defect. To modulate mitochondrial dysfunction and oxidative stress, creatine, vitamin E, coenzyme Q10, melatonin and deferoxamine have been tried in clinical studies. In a RPCT, coenzyme Q10 improved the Unified Parkinson’s Disease Rating Scale (UPDRS) score in PD (Yoritake et al. 2015), but another study of high-dosage coenzyme Q10 could not confirm the beneficial effects in early PD (Parkinson Study Group Qe3 investigators 2014).
Antioxidant function of phytochemicals
Polyphenols, especially flavonoids (apigenin, quercetin) directly scavenge free radicals, chelating metals and induce reduction–oxidation (redox)-related proteins. Flavonoids (isoquercetin, quercetin glycosides, rutin), resveratrol, astaxanthin and protocatechuic acid activate Nrf2/Keap1 (Kelch-like ECH-associated protein1) pathway to increase antioxidant enzymes, superoxide dismutase (SOD), catalase, heme-oxygenase-1 (HO-1), glutathione peroxidase (GPx).
Flavonoids donate a hydrogen molecule, form a phenoxyl radical, release another hydrogen and turn single oxygen, O2−, –OH, alkoxyl and peroxyl radicals to a stable quinone structure. The diol group forms a complex with ferric iron, copper and other transition metal ions and prevents ROS production. Antioxidant function depends on the number of hydroxyl groups in the aromatic A and B rings and the presence of 2,3-unsaturation and a 4-carbonyl in the C ring. The hydroxyl substitutions in the 3-position of C-ring and 4 and 7 of the A-ring are important for the antioxidant potency. EGCG has strong antioxidant properties via the radical scavenging by an ortho-hydroxyl group in the B ring and a gallery group at position 3.
The hydroxyl and methoxy groups of curcumin can scavenge ROS/RNS, and prevent lipid peroxidation in vivo and in vitro. Hydrogen-abstraction from phenolic groups in hydrogen-atom-transfer and single-electron-transfer mechanisms are associated with scavenging peroxy radicals. Curcumin activates Nrf2 and increases GSH, glutamate cysteine ligase (a rate-limiting enzyme of GSH synthesis) and Cu–Zn SOD.
trans-Resveratrol is more bioactive than the cis-form, and it can directly scavenge –OH radical with its hydroxyl groups, and 4′-hydroxyl group is the most reactive. The presence of conjugated double bonds in two phenolic groups makes the electrons more delocalized and resveratrol donates a hydrogen to hydroperoxyl (.OOH) radicals in its phenol group and prevents peroxidation. Resveratrol can scavenge free radicals and quench singlet oxygen in vitro, but the potency in vivo is quite low, and the in vivo biological function mainly depends on activation of Sirt1, PI3K/Nrf2/Keap/NF-κB pathway and peroxisome proliferator-activated receptor-γ (PPAR-γ), PPAR) γ cofactor-1 (PGC-1α) and enhancement of expression of antioxidant enzymes, GPx, HO-1, inducible nitric oxide synthase (iNOS), and cyclooxygenase (COX)-2. Phenolic acid has electron-donating 3-methoxy and 4-hydroxy groups on the benzene ring, and the carboxylic acid has an adjacent unsaturated carbon–carbon double bond, binds to lipid bilayer and prevents lipid peroxidation.
Astaxanthin scavenges ROS and prevents lipid peroxidation in membrane. The hydrophobic region of astaxanthin is a series of carbon–carbon double bonds alternating with carbon–carbon single bonds. The conjugated double bonds can remove an unpaired electron from radical, or donate electrons to radical. Its linear structure provides astaxanthin to scavenge radicals in the interior and at the surface of membrane (Goto et al. 2001). Astaxanthin can scavenge ROS tenfold potentially than carotinoids and 100-fold than α-tocopherol.
Regulation of mitochondrial apoptosis pathway by phytochemicals
In neurodegenerative disorders, apoptosis is often detected by the morphological and biochemical changes. Apoptosis cascade in mitochondria is a promising target for neuroprotection by bioactive phytochemicals (Fig. 3). Apoptosis is initiated by increased mitochondrial membrane permeability and formation of transitional and reversible pore at the inner mitochondrial membrane, by the binding of cyclophilin-D (Cyp-D) localized at the matrix to adenine nucleotide translocator (ANT) at the inner membrane. Prolonged insults fully open a non-selective mitochondrial permeability transition pore (mPTP) at the contact site between the inner and outer membrane, which increase the permeability to solutes and causes expansion of the matrix and rupture of the outer membrane. Irreversible opening of the mPTP is the “point of no return” of cell death, and releases caspase-activating proteins [cytochrome c (Cytc), SMAC/DIABLO] from the matrix into the cytoplasm and causes fragmentation and condensation of nuclear DNA. The major components of the mPTP are voltage-dependent anion channel (VDAC) at the outer membrane, and ANT and CypD at the inner membrane. In addition, anti- and pro-apoptotic Bcl-2 protein family, the outer membrane translocator protein 18 kDa (TSPO), hexokinase (HK)-I and II are associated with VDAC on the cytoplasmic face of the outer membrane, and creatine kinases (CK) at the intermembrane space. Glycogen synthase kinase-3β (GSK-3β) phosphorylates VDAC and inhibits its interaction with HK and ANT. The TSPO induces mitochondrial membrane permeabilization (MMP). Bcl-2 protein family regulates either in a preventive (Bcl-2, Bcl-xL, Bcl-w), or promoting way (Bax, Bak, Bid, Bad, Puma, Noxa). Recently the F1–F0-ATP synthase (F-ATPase) was reported to form the mPTP. Ca2+ binds to the F-ATPase at the catalytic site by replacing Mg2+, changes the conformation and F-ATPase is translocated from the matrix to the inner membrane, binds to CypD and forms the mPTP.
Effects of phytochemicals on mitochondrial apoptosis system and homeostasis. Phytochemicals inhibit stepwise opening of pore at the inner and outer membrane induced by PK11195, or other insults. They directly regulate expression of VDAC or anti-apoptotic Bcl-2 or inhibit the activation of caspase 3. Phytochemicals activate signal transduction, increase mitogenesis, and promote fission/fusion and mitophagy to stabilize mitochondrial function. White arrows represent protective effects, whereas, black arrows cytotoxic effects. Upward or downward arrow means promoting or inhibiting effects
Resveratrol, quercetin, rosmarinic acid, astaxanthin and black tea extract prevent the MMP and protect cells from apoptosis induced by MPTP, wild-type and mutated (A30P, A53T) αSyn and ischemia. Phytochemicals directly prevented or promoted the pore formation at mitochondrial membrane in a cellular model of apoptosis induced by a ligand of the TSPO, PK11195, 1-(2-chlorophenyl)-N-methyl-N-(1-methylpropyl)-3-isoquinoline carbamate (Wu et al. 2017). PK11195 induced the pore formation at the inner membrane with the burst of superoxide production called “superoxide flash”, and then the mPTP opened with calcium efflux from mitochondria. Astaxanthin and lipophilic methoxy derivative of ferulic acid inhibited formation of pore composed of ANT and Cyp-D at the inner membrane, and the following mPTP opening and apoptosis. Ferulic acid aldehyde and alcohol (coniferyl aldehyde, alcohol) prevented the pore formation at the outer membrane and the mPTP. Hydrophilic ethyl ester of ferulic acid promoted the mPTP opening, calcium efflux and apoptosis. These results suggest that microenvironment in the mPTP might be modulated by the amphipathic properties of phytochemicals, and the vital SH residue(s) in ANT might be reduced or oxidized by the redox potency of phytochemicals.
Resveratrol prevents oxidative modification of the critical thiol residues in ANT and membrane protein, phosphorylates Akt/GSK-3β pathway, dephosphorylates VDAC, promotes VDAC dissociation from Bax, activates poly(ADP-ribose)polymerase (PARP), and prevents the mPTP opening induced by oxidative stress and MPP+ (Tian et al. 2019). Curcumin binds to the amino acids in the N-terminal α-helix of VDAC, changes the conformation and prevents the pore formation (Tewari et al. 2015). EGCG is accumulated in mitochondria and locally scavenge free radicals. Among five ingredients of green tea catechins, the anti-apoptotic potency was in order, epicatechin gallate (ECG), EGCG >> epicatechin (EC), catechin >> epigallocatechin (EGC), indicating the essential role of 3-gallate group in neuroprotection (Jin et al. 2001). Black tea extract, theaflavins, rosmarinic acid and flavonoids directly interacts with membrane phospholipids, prevents the MMP. 5,7-Dihydroxy4-oxo-moiety of baicalein and morin enhances anti-apoptosis potency. Curcumin, protocatechuic acid, ginsenoside Rg1 and puerarin interact with caspase proteins and prevent apoptosis. Flavonoids (baicalein, EGCG, kaempferol, naringenin, quercetin), curcumin and berberine activate signal pathways to induce the expression of anti-apoptotic Bcl-2 and Bcl-xL and suppress that of apoptogenic Bax and Bak and modulate apoptosis pathway in mitochondria.
Impaired mitochondrial biosynthesis, dynamics and autophagy in Parkinson’s disease
Mitochondria are dynamic organelle. The biogenesis (mitogenesis), quality control by fission (division) and fusion, and cleavage of damaged mitochondria by autophagy regulate mitochondrial homeostasis. Deregulated mitochondrial dynamics has been proposed to attribute PD pathogenesis (Zilocchi et al. 2018). Mitochondrial biogenesis is a complex process with high ATP requirement, involving mtDNA replication, coordinated gene expression, protein synthesis, membrane formation and mitochondrial division. PGC-1α is a major transcriptional regulator of mitogenesis and regulate the dynamics with nuclear respiratory factor (NRF)-1, -2. Mitochondrial transcription factor (TFAM) regulates mtDNA replication and transcription. PGC-1α activates NRF-1 and NRF-2 transcription factors and estrogen-related receptor α (ERRα) and induces expression of nuclear DNA-encoded mitochondrial protein. PGC-1α activity is post-transcriptionally regulated by phosphorylation and acetylation, and Sirt-1deacetylates PGC-1α and regulates the activity. In the Parkinsonian SN, TFAM and mtDNA were downregulated, suggesting that impaired nuclear–mitochondrial regulation is associated with neuronal loss (Chen et al. 2020).
Mitochondrial fission and fusion determine the size, number and shape, and critically regulate neuronal death (Santos et al. 2015). Dynamin-related GTPase 1 (DRP1) mediates mitochondrial fission specifically on mitochondrial membranes. Mitochondrial fusion is mediated by DRP1-mimics, mitofusin (Mfn) and optic dominant atrophy 1 (Opa1). Mfns are localized at the outer membrane, and fuse mitochondrial membranes of adjacent tubules, and Opa1 is located in the inner membrane and interacts with Mfns to form inter-membrane protein complexes. PGC-1α and -1β, ERRα, the transcription factor MEF2 (myocyte enhancer factor-2) induce Mfn expression. Loss of Opa1 induced disruption of mitochondrial cristae and spontaneous apoptosis.
A selective degradation of mitochondria by autophagy is known as “mitophagy”, and its downregulation results in accumulation of dysfunctional and fragmented mitochondria. Mitophagy plays an important role in preservation of intracellular energy, mitochondrial quality, appropriate mass and population, and promotes cell survival in aging and neurodegenerative diseases (Tatsuta and Langer 2008).
In familiar PD, mitochondrial dysfunction is caused by autosomal dominant SNCA and leucine rich repeat kinase 2 (LRRK2) mutations, and autosomal recessive Parkin, PTEN-induced putative kinase (PINK1) and P5-type ATPase 13a2 (ATP13a2) mutations. Mutated Parkin (an E3 ubiquitin ligase) and PINK1 (a seine/threonine kinase) in autosomal PD modify mitophagy and mitochondrial dynamics. Impaired mitochondria are also degraded by the UPS, after phosphorylated by PINK1 and ubiquitinated by Parkin. Parkin incorporated into mitochondria modulates mitochondrial morphology and fission/fusion, and promotes mitophagy (Poole et al. 2008). PINK1 or Parkin mutation causes the accumulation of damaged mitochondria in axons in Parkinsonian patients (Liu et al. 2012).
αSyn is associated with mitochondrial dysfunction. Human αSyn has a mitochondria-targeting 32 amino acid sequence at the N-terminal region (NTR) and is transported into mitochondria by translocases of outer membrane (TOMs) and inner membrane (TIMs) and is localized predominantly at the inner membrane. αSyn is significantly accumulated in mitochondria of the DA neurons in the striatum, SN and cortex of Parkinsonian brains (Devi et al. 2008). Monomeric αSyn has high affinity to VDAC and induces mitochondrial dysfunction and cell death (Rostovtseva et al. 2015). Under physiological conditions, αSyn monomers improve ATP synthase efficiency and mitochondrial function, whereas, αSyn oligomers interact with ATP synthase, oxidize the β subunit and induce the mPTP opening (Ludtmann et al. 2018). αSyn oligomers interact with membrane lipids and about 15% of αSyn molecules present as membrane-bound aggregates in vivo. αSyn changes the conformation from α-helix to a coiled structure, and forms pore-like structure in vitro study. αSyn aggregates in the cytoplasm interact directly with membrane cardiolipin, an anionic phospholipid specific to mitochondria, and destabilize the membranes. Cardiolipin increases αSyn accumulation at the inner membrane and promotes the aggregation and pore formation at mitochondrial membrane. αSyn inhibits the nuclear translocation of high mobility group box 1 (HMGM1) and impairs autophagy. In addition, PD-related mutations, post-translational modifications and oxidative stress increase nuclear translocation of αSyn and downregulate PGC-1α, and induce mitochondrial dysfunction.
Phytochemicals promote mitogenesis and preserve mitochondrial quality
Phytochemicals enhance mitochondrial synthesis, maintain dynamics and quality control, and prevent mitochondrial dysfunction. Resveratrol and curcumin inhibit cAMP phosphodiesterases and increase cAMP, or activate PKCε and increase NAD, activate AMPK/Sirt1/PGC-1α pathway and stimulate mitochondrial function, biogenesis and dynamics (Higashida et al. 2013). Resveratrol activates Sirt1, mitochondrial Sirt3, and Foxo3/PINK1/Parkin signaling pathway, maintains the balance between fusion and fission, prevents mitophagy and protects cells (Das et al. 2014). In primary fibroblast culture from patients with Park2 mutations, resveratrol activated AMPK/Sirt1/PGC-1α l pathway, enhanced mitochondrial functions and autophagic efflux, and maintained energy homeostasis (Ferretta et al. 2014). Flavones (baicalein, quercetin, wogonin), isoflavones (daidzen, genistein), curcumin and hydroxytyrosol (3,4-dihydroxyphenyl-ethanol, present in olives) increase expression of Sirt1/AMPA/PGC-1α, enhance mitochondrial biogenesis, the ETC components and TFAM in vivo and in vitro (Dos Santos et al. 2018). Anthocyanins stabilized the fusion/fission processes and protected neuronal cells against cytotoxicity of rotenone and amyloid precursor protein (APP)swe mutation. Oleuropein (the main polyphenol isolated from extra virgin olive oil) increased expression of mtDNA, PGC-1α, complex II and IV, regulated mitochondrial function, mitogenesis and dynamics through Mfn1 and DRP1 in vivo (Sun et al. 2017). EGCG activated Sirt1/PGC-1α pathway and upregulated Nrf1 and TFAM, increased mtDNA content, and promoted mitochondrial biogenesis in cells from subjects with Down’s syndrome (Valenti et al. 2013). Allicin (diallyl thiosulfinate, the main biological compounds derived from gallic) inhibited DRP-1 increase and Opa1 decrease, regulated mitochondrial dynamics, and prevented mitochondrial fragmentation in 6-OHDA-treated PC12 cells.
In contrast to the results in preclinical studies, the effects of polyphenols on mitogenesis in humans have been shown only by a few trials. Quercetin and EGCG supplement increased the mRNA levels of Sirt1, PGC-1α, cytochrome c oxidase and creatine synthase in skeletal muscle after 2-week administration in young adult males (Nieman et al. 2010). EC-rich cocoa increased Sirt1, PGC-1α, TFAM, complex I and V, and enhanced mitogenesis in biopsied skeletal muscle from patients with type 2 diabetes and heart failure, and EC-rich dark chocolate significantly increased AMPA and PGC-1α and enhanced mitogenesis in normal sedentary subjects (Taub et al. 2016).
Anti-inflammatory functions of phytochemicals
Neuroinflammation is associated with PD pathology and is caused by age-dependent decline of immune response, infection, neurotoxins and accumulation of insoluble protein fibrils, such as αSyn. In the Parkinsonian SN and striatum, inflammatory processes are indicated by microglia activation, production of cytokines (IL-1α, Il-2, IL-6, IL9, TNF-α, TGF-β), inflammatory mediators [nitrite, nitric oxide, prostaglandin E2 (PGE2)] and the presence of autoantibodies. In the serum of PD patients, levels of HMGB1 and toll-like receptor 4 (TLR4), and their downstream signaling factors, NF-κB, TNF-α and myeloid differentiation factor 88, increased in accord to the progression (Yang et al. 2018). Mutations of SNCA, LRRK2, PINK1, Parkin and DJ-1 activated microglia and neuroinflammation (Lee et al. 2017). Toxic oligomeric or fibrillar αSyn activates TLR2 and stimulates the innate/cell-mediated immune system and microglia.
Phytochemicals inhibit activities of pro-inflammatory enzymes, COX-2 and lipoxygenases and cellular processes involved in inflammatory responses. Phytochemicals prevent the activation of transcription factors [NF-κB, activator protein (AP)-1], signal transducer and activator of transcription (STAT) and PPAR family or activate the anti-inflammatory and antioxidant activities (Kaur et al. 2020). Flavonoids (apigenin, EGCG, luteoloside, quercetin) inhibit expression of inflammasome components, NOD-like receptor (NRL) family and pyrin domain-containing 3 and 1 (NLRP3, NLRP1), and oligomerization of NLRP3 inflammasome. Flavonoids (3′,4′-dihyroxyflavone, 3′,4′-dichloroflavone, apigenin, kaempferol, quercetin) inhibit activation of TLR4 and NF-κB, and production of TNF-α, nitric oxide, IL-1β and PGR2 by NLRP3 inflammasome (Lim et al. 2018). 5,7-Dihydroxyl groups in the A ring and one to two hydroxyl or dichloro groups at C-3′,4′ in the B ring of flavones and flavonols are required for inhibition of IL-6β production. Curcumin and resveratrol reduce TLR4 expression in neurons, microglia and macrophages, and prevent activation of TLR4 signaling and NF-κB, and production of inflammatory cytokines and monocyte chemoattractant protein-1 (MCP-1). Resveratrol activates Sirt1 and reduces matrix metallopeptidase 9 expression and neuroinflammation. Rosmarinic acid inhibits HMGB1/TLR4/NF-κB signaling pathway and attenuates inflammatory responses (Lv et al. 2019).
Phytochemicals modulate α-synuclein oligomerization, aggregation and toxicity
αSyn is present as natively unfolded soluble form in high concentration at the presynaptic terminals. Changes in the protein environments increase the hydrophobicity of αSyn, decrease the net charge and induce folding. Monomeric αSyn is unfolded protein and by self-assembly transforms to partially folded intermediates, then higher order soluble oligomers in a size range from dimers to protofibrils. αSyn has three sequence regions: NTR (residues 1–60), a central hydrophobic region, called non-amyloid β-component with a conserved motif (KTKEGV) (NAC, residue 61–65) and a C-terminal region (CTR, residues 66–95). After binding to membrane, NTR forms two α-helices, changes the conformation from a random coil to β-sheet structure and amyloid β-like fibrils, whereas, CTR is highly acidic, anti-amyloidogenic and involved in Ca2+ binding. The central hydrophobic NAC region is the nucleation core and associated with αSyn fibrillization. Many factors, such as αSyn mutations, pH of the environment and presence of chaperones, accelerate misfolding process of amyloidogenic protein. The aggregation progresses in the presence of fibrillar seed, cupper and iron and by posttranslational modification, binding of DA, DOPAL and noradrenaline, proteolysis and modification (Singh and Bhat 2019).
Phytochemicals prevent α-synuclein oligomerization and neurotoxicity
Phytochemicals inhibit αSyn synthesis, oligomerization and aggregation, and disassemble preformed αSyn aggregates by remodeling the fibrils and immobilizing C-terminal tail in vitro and in vivo (Henriquez et al. 2020), as summarized in Fig. 4. 7,8-Dihydroxyflavone (7,8-DHF) and astibin (taxifolin3-O-rhamnoside, a bioactive ingredient in St John’s wort, Hypericum perforatum) downregulated αSyn expression in MPTP-induced mouse model of PD (Li et al. 2016). Ellagic acid inhibits primary nucleation, seeded aggregation, and membrane-induced aggregation (Kumar et al. 2021).
Interaction of phytochemicals on αSyn misfolding and aggregation. Phytochemicals suppress the αSyn synthesis and inhibit multiple stages of toxic oligomerization and aggregation. Curcumin and resveratrol potentiate autophagy and cleave aggregated αSyn. White arrows represent protective effects, whereas, black arrows cytotoxic effects. Black and white figures mean toxic and non-toxic derivatives of αSyn derivatives
Flavonoids (baicalein, kaempferol, catechin, EGCG, myricetin), resveratrol, theaflavins, oleocanthal (deacetoxy ligstroside aglycon, a phenolic compound of extra-virgin olive oil), rosmarinic acid, tannic acid and salvianolic acid B (a bioactive polyphenol extracted root of Salvia miltiorrhiza) bind to the native, unfolded αSyn monomers, engage αSyn in compact conformations and unfold polypeptide chains. Oleuropein aglycone stabilizes αSyn monomers, promotes the growth of stable non-toxic aggregates and protects the membrane (Mohammad-Beigi et al. 2019).
Polyphenols bind to β-sheet-rich oligomeric intermediates with much higher affinity than to the monomers, and redirect the assembly process into off-pathway, to form non-toxic, SDS-resistant spherical and non-structural oligomers of ~ 20 nm diameter (Ehrnhoefer et al. 2008). Aromatic rings of polyphenols interact with αSyn and inhibit its self-assembly by π–π and hydrophobic interaction. αSyn disaggregation by natural polyphenols is correlated with the number of hydroxyl groups on a single phenyl group; trihydroxy- (baicalein, scutellarein, EGCG, myricetin, tannic acid) > dihydroxy- (quercetin, morin, apigen, resveratrol, rosmarinic acid) > monohydroxy-phenyl ring [pupurogallin (2,3,4,6-tetrahydroxy-5-oxo-5H-benzo [7]annulene), ginkgolide B] (Caruana et al. 2011). The presence of 2,3-double bond in the C ring further enhanced the disaggregation. 3′,4′-Dihydroxy substitution on ring B of flavonoids and 2′,3′-dihydrol promotes inhibition of fibril formation, whereas, methoxylation of hydroxyl groups abolishes the inhibition. Flavonoids non-covalently bind to αSyn and sequentially produce flavonoid quinones, which covalently bind to free amines or thiols, and stabilize the soluble form of αSyn, monomers and oligomers and EGCG-derived quinones modify the amyloidogenic protein through Schiff base formation, crosslink the fibrils and prevents toxicity.
EGCG binds specifically to αSyn fibrils, alters the hydrophobic surface exposure, or disrupts the local b-sheet structure into benign, amorphous aggregates (Yao et al. 2020). Among EGCG-related polyphenols, ECG, gallocatechin gallate and EGCG containing a gallate group can modulate αSyn aggregation, but catechin and EC do not. A gallate group has surface active and amphipathic properties and might function as a surfactant (Lorenzen et al. 2014). EGCG blocks αSyn aggregation-prone sites, GKTKEGVLY, GVLYVGSKT, AAATGFVK, prevents conversion of active oligomers of αSyn into amyloid fibrils and prevents membrane disruption (Yang et al. 2017b). Polyphenol components of olive, such as verbascoside, elenolic acid, 3-hydroxytyrosol (3,4-dihydroxphenylethanol), inhibit αSyn fibril nucleation and elongation, and disaggregate preformed fibrils and prevent formation of the toxic oligomers (Mohammad-Beigi et al. 2019). Dihydromyricetin RB1 (a flavonoid ingredient isolated from seem and leaves of Ampelopsis grossedentaa) to the oligomers and disaggregate preformed αSyn fibrils. Ginsenoside Rb1 disaggregates performed αSyn fibrils, stabilizes soluble non-toxic oligomers containing no β-sheet, inhibits seeded polymerization and suppresses the neurotoxicity (Ardah et al. 2015). Curcumin and black tea extract promote autophagy and clearance of wild and mutant αSyn (A30P, A53T) and prevent MMP. Resveratrol activated Sirt1, deacetylated microtubule-associated protein 1 light chain 3 (LC3), promoted autophagic degradation of αSyn and exerted neuroprotection in MPTP-induced mouse model of PD (Guo et al. 2016).
Several polyphenol derivatives have been synthesized to intervene the αSyn aggregation at different stages. Carbamic ester derivatives of 7,8-DHF were more potent inhibitors than L-DOPA, and 4-oxo-2-phenyl-4H-chromene-7,8-diyl bis(1-amino-2-hydroxypropyl)carbamate had the highest binding to αSyn (Mohankumar et al. 2020). Curcumin derivatives were synthesized by replacement of the hydroxyl groups with methoxyl and –CH2-phenyl group, and the aromatic group with heteronuclear aromatic moieties, thiophene and pyridine to increase the inhibition (Jha et al. 2016). The benzene rings of curcumin play essential role, and the methoxyl replacement of curcumin masks the exposed hydrophobic surface of preformed αSyn fibrils and increases inhibition of αSyn fibrillation. Presence of –CH2-phenyl group promotes binding to preformed fibrils, suggesting the interaction of phenyl with the hydrophobic patches of αSyn. Curcumin pyrazole and N-(3-nitrophenyl-pyrazole) curcumin inhibit fibrillation of wild and mutant αSyn, disrupts preformed fibrils and prevents the toxicity (Ahsan et al. 2015). Incorporation of fluoro group in phenylzole curcumin at meta position significantly increases the potency to inhibit aggregation and disrupt fibrils.
Phytochemicals modulate deregulation of the UPS and ALP in PD
Dysfunction of the UPS and ALP causes accumulation of Lewy body and Lewy neurites in PD (Pan et al. 2008). The UPS selectively targets the unfolded ubiquitinated proteins, degrades short-lived proteins controlling signal transduction, cell cycle progression, apoptosis and cellular differentiation. Chymotrypsin-, trypsin- and caspase-like activity of the UPS decreased significantly in the SN of Parkinsonian patients (Furukawa et al. 2002). Mutations of αSyn, parkin, UCH-L1 and ATP13a2, A53T, A30P, E46K and increase in non-mutant αSyn by triplicated SNCA inhibit αSyn ubiquitination and the UPS activity, leading to αSyn accumulation in the SN.
Autophagy is induced by deficit of nutrients and energy supply and is the main system for degradation and recycling of long live, stable proteins, mitochondria, membrane proteins and protein oligomers and aggregates. The ALP is classified into macroautophagy (generally referred as autophagy), microautophagy and chaperone-mediated autophagy (CMA). Deregulated autophagy is associated with the pathogenesis of PD, especially autosomal dominant and recessive PD with mutations of SNCA, LRRK2, GBA encoding glucocerebrosidase (GCase), UCHL1 and DJ-1 (Manzoni and Lewis 2013). αSyn oligomers inhibit the UPS and ALP (Scrivo et al. 2018). Mutated and DA-modified αSyn have high affinity for the lysosomal membrane receptors and inhibit the lysosomal uptake and degradation by the CMA (Cuervo et al. 2004), whereas, wild type αSyn is translocated into lysosomes and degraded by the CMA pathway (Vogiatzi et al. 2008).
Phytochemicals modulate the ALP (Wang et al. 2017). Kaempferol and its glycoside (icariin) increase LC3-II, enhance mitochondria turnover by autophagy and exert neuroprotection in cell and animal models of PD (Filomeni et al. 2012). Loganin [7-hydroxy-6-desoxyvenalin, an iridoid monoterpenoid derived from fruits of cornus (Cornus officinalis)] downregulated LC3-II and Drp1 expression and autophagy and exerted neuroprotective effects in a MPTP-treated mouse model of PD. Carnosic acid from rosemary promoted parkin translocation into mitochondria, induced the interaction of parkin and Beclin-1, activated PINK1/parkin-mediated mitophagy and protected SH-SY5Y cells against 6-OHDA toxicity (Lin and Tsai 2019). EGCG promoted AMPK/mTOR (mammalian target of rapamycin)/autophagy pathway and protected HEK293T cells against endoplasmic reticulum stress (Holczer et al. 2018). Resveratrol, genistein and quercetin activate Sirts and modulate autophagy either directly by promoting deacetylation of Atg5, Atg7 and Atg8, or indirectly by regulating FOXO3a (the Forkhead box) transcription factor.
Phytochemicals bind to NTF receptors, activate signaling pathways and enhance NTF expression
NTFs play a major role in the development, function and survival of neurons. GDNF is a potent NTF specific for dopaminergic neurons and decreased in the Parkinsonian SN and hippocampus. GDNF binds to GDNF family receptor α (GFRα), phosphorylates the receptor tyrosine kinase RET (rearranged during transfection), activates PI3K and ERK/ mitogen-activated protein kinase (MAPK) pathways and maintains DA neurons in the adult brain. GDNF was administered in the nigra-striatal system of PD patients, using infusion or gene therapy of GDNF and neurturin (Barker et al. 2020), but effects of the intracerebral application have not fully been established (Whone et al. 2019). BDNF is required for development of nervous system and the deficit is involved in neurodegeneration and depression. BDNF decreases in Parkinsonian SN (Parain et al. 1999), Val66Met polymorphism of BDNF increases susceptibility to PD in Caucasians and is associated with cognitive decline in PD (Bieschke et al. 2010).
As presented in Fig. 5, phytochemicals show NTF-mimic activity by binding to NTF receptors, activation of downstream signal pathways and induction of NTF expression. 7,8-DHF, 7,8,3′-trihydroxyflavone, fisetin, deoxygedunin (a derivative of gedunin isolated from Azadirachta indica), diosmetin and curcumin bind to tropomycin-related kinase B (TrkB), the BDNF receptor, and activate PI3K/Akt, Ras/mitogen-activated protein (MAP)/ERK pathways, phospholipase C-γ (PLC-γ) and finally cAMP-response element-binding protein (CREB) in nuclei (Liu et al. 2014). 7,8-DHF showed the BDNF-mimic effects and prevented progressive degeneration of midbrain dopaminergic neurons in MPP+-treated monkey (He et al 2016). Hesperetin, huperzine (a sesquiterpene derived from Huperzia serrata), 4,6-dimethoxyphenyanthrene, spicoside A [6-hydroxyluteolin-7-(6″-(E)-caffeoxylglucoside) and quinic (= chinic) acid derivatives bind to TrkA receptor, the nerve growth factor (NGF) receptor, increased neurite outgrowth and showed neuroprotective potency (Hwang and Yen 2011). Phytochemicals directly intervene cellular signal molecules. Flavonoids (genistein, EGCG), curcumin and resveratrol activate PI3K/Akt, PKC, MAPK and Ras/MEK1/2/ERK1/2 pathways, increase Nrf2/HO-1 and finally phosphorylate CREB, which binds to CREB-binding protein (CBP) and increases transcription of target genes coding antioxidant enzymes, anti-apoptotic Bcl-2 and pro-survival NTFs (Vauzour et al. 2007). Flavonoids (quercetin, EC, hesperetin, icariin) inhibited cytotoxic JNK activity and prevented apoptosis.
Phytochemicals induce neuroprotective signaling pathways and protect neuronal cells. They bind to TrkB and other receptors at the plasma membrane, activate signal pathways, or directly activate PI3K, PKC and Ras/ERK1/2 pathway and promote transcription to express antioxidants, NTFs and anti-apoptotic Bcl-2 family. White arrows represent protective effects
Phytochemicals induce NTF expression in vivo and in vitro. NTFs cannot cross the BBB and the delivery system is required for transport into the brain. As an alternative practical method, the activation of de novo biosynthesis of BDNF and GDNF has been proposed by phytochemicals permeable of the BBB, including EC, EGCG, naringenin, curcumin, resveratrol and astaxanthin. Flavonoids, astaxanthin, curcumin, ginsenosides Rb1 and Rg1, phenolic acids, resveratrol, smilagenin (5β,20α,22α,25R-spirostan-3β-ol, a sapogenein from Rhizoma anemarrhenae, Radix asparagi) enhance expression of GDNF, BDNF, NGF, transforming growth factor-β1 (TGFβ1) and vascular endothelial growth factor (VEGF) in animal and cell models. Smilagenin [(25R)-5β-spirostan-3β-ol], catalpol and harpagoside (bioactive ingredients from Rehmannia glutinosa, Scrophularia ningoensis), naringen and curcumin stimulate intrinsic GDNF expression and protect dopaminergic neurons in vivo and in vitro (Sun et al. 2012). Apigenin, luteolin, puerarin, and caffeic acid phenethyl ester (a honeybee propolis ingredient) enhanced BDNF expression in the SN of neurotoxin-treated rodent models and protected nigral dopaminergic neurons (Kurauchi et al. 2012). Resveratrol and 6,7,4′-trihydroxyiso-flavone activate Sirt1/miR-134 signal pathway and induce CREB/BDNF expression in the hippocampus and improve cognitive function. BDNF is induced by flavonoids in vivo and in vitro, whereas, GDNF is mostly by non-flavonoid phytochemicals, curcumin, resveratrol and catalpol. It may be relevant with the results that flavonoids improve memory, cognition and depression, whereas, resveratrol and curcumin ameliorate neuronal dysfunction and prevent cell death in animal models of PD and AD.
Only few clinical trials could prove NTF induction by phytochemicals. In a RPCT, high-flavonoid intake, fruit and vegetables for 6 weeks in control subjects (26–70 years of age), or high-flavonoid cocoa drink for 12 weeks in older males and females (62–75 years of age) increased serum BDNF levels and improved cognitive function (Neshatdoust et al. 2016). In healthy subjects, coffee fruit extract increased plasma BDNF level (Reyes-Izquierdo et al. 2013). Ginkgo biloba supplement and green tea extract increased serum BDNF in physically active men (Sadowska-Krepa et al. 2017). In women with premenstrual syndrome, curcumin upregulated serum BDNF levels and ameliorates the syndrome (Fanaei et al. 2016). In Parkinsonian patients, no clinical trial of phytochemical has been reported to upregulate BDNF and GDNF levels.
A specific binding site for catechin gallates (EGCG, ECG) and resveratrol was isolated from plasma membrane in the rat brain, which might be associated with neuroprotection by polyphenols in hippocampal cells against Aβ25–35 toxicity (Han et al. 2006). EGCG binds to 67-kDa laminin receptors localized at cell surface, activates signal pathways to enhance BDNF and potentiate neurite synthesis (Gundimeda et al. 2014). Neuronal α7-nicotoninic acetylcholine receptor (nACHR) mediates neuroprotection by curcumin in dopaminergic neurons against 6-OHDA (Nebrisi et al. 2020) and by EGCG in cultured cortical neurons against Aβ1–42-induced cytotoxicity (Zhang et al. 2014). Flavonoids (calycosin, isohamnetin, luteolin, genistein, hesperetin) and resveratrol bind to estrogen receptor β (ERβ) and enhance BDNF, GDNF and NGF expression and promote cell survival in astrocytes (Xu et al. 2013). Curcumin and the derivative J147 activate serotonin-1A (5-HT1A) receptor and cAMP/BDNF signaling, induce hippocampal neurogenesis and exerted neuroprotective and antidepressant properties (Li et al. 2020).
Discussion
Epidemiological studies present that the greater intake of diet, vegetables, legumes and fruits containing anthocyanidins, quercetin, and EC reduced incidence of PD (Gao et al. 2012). An inverse association was reported between coffee and tea consumption with PD in males, but not in females, by Health Professionals Follow-up Study (HPFS) (Ascherio et al. 2001). RPCTs of flavonoids (green tea catechins, EGCG, anthocyanins), resveratrol and curcumin improved cognitive activity and increased serum BDNF in AD, MCI and control subjects (Huhn et al. 2018). However, to date clinical intervention trials of phytochemicals have not presented clear evidence of disease modulation in PD. Discrepancy between encouraging preclinical results and the failure of clinical trials may be due to inadequate designs of clinical intervention trials, improper evaluation of therapeutic effects, selection of end points and subjects from heterogeneous patient groups, trial duration and dose of phytochemicals.
Poor bioavailability of phytochemicals also inhibits the in vivo therapeutic efficiency. Polyphenols containing catechol and pyogallol moieties have poor pharmacokinetic properties and bioavailability, rapid metabolism, the inefficient permeability across the BBB and instability in the brain. To enhance the bioavailability, several methods have been proposed: modification of phytochemicals, liposomes, nanoparticles and inclusion complexes with cyclodextrin (Lewandowska et al. 2013). Structural modification of resveratrol by hydroxylation, amination, methoxylation, prenylation and glycosylation increased stability and bioavailability (Arbo et al. 2020). Oxyresveratrol (tetrahydroxystilbene), pinostilbene (3-methoxy-4′,5-dihydroxy-trans-stilbene) and a fully acetylated resveratrol showed increased bioavailability and neuroprotection in cellular models of PD. Lipophilic metabolites (O-methylated derivatives) are permeable more markedly than polar ones (glucuronidated, sulfated one). Conjugation of pharmacologically active moiety to the scaffold of BBB-permeable phytochemicals, such as lipophilic flavonoids, coumarins, gingolide B and terpene, has been proposed to increase bioactivity (Youdim et al. 2004). Nanoplatforms of phytochemicals, such as micro-, nano-emulsion, liposomes and nanoparticles, may be one of future promising delivery systems to maintain adequate concentrations in the brain, but more preclinical studies will be required.
Recently, bidirectional communication between the gut and the brain has been suggested in PD, AD, anxiety, depression, attention-deficit hypersensitivity disorder (ADHD) and autisms spectrum disorders (ASDs) (Cryan et al 2019). Inside the gastrointestinal tract, a complex ecological community called gut microbiota exists, which forms a permanent symbiotic relationship and have a wide range of physiological functions, including digestion, growth and self-defense. Microbiota interacts with the central nervous system and immune system, including the endocrine [the hypothalamic–pituitary–adrenal (HPA)] axis, immune (chemokines, cytokines), autonomic nervous system and enteric nervous system, forming microbiota-gut-brain (MGB) axis. In PD, microbiota-based therapeutic strategies have been proposed for treatment of gastrointestinal alterations, neuroinflammation and also motor symptoms (Sampson et al. 2016).
Gut microbiotas are associated with the biochemical processes of phytochemicals, especially flavonoids (quercetin, isoflavone) to become bioactive in human body. Dietary flavonoids are present in the glycoside form, and intestinal enzymes, such as β-glucosidases and lactase-phlorizin hydrolase, cleave the sugar moieties. Microbiotas cleave sugars into aglycones, such as rhamnose by α-rhannosidases secreted by Bifidobacterium dentium, and diverse hydroxyl moieties are modified, such as acetylation of flavanones by gallic acid. The backbone structures of flavonoids are remodeled by microbiota. Daidzein is metabolized to equol or a ring-fission product, O-desmethlangolensin, both of which act as nonsteroidal estrogens (Murota et al. 2018). The metabolites are absorbed into the blood circulation and distributed. The bioavailability of most polyphenols is quite low, but colonic microflora can breakdown them into hydrocinnamic, phenylacetic and benzoic acid derivatives, which are directly absorbed via the colon. Many metabolites are detected in the human bloodstream, but in the brain only a few metabolites, such as gallic acid and its dimerized ellagic acid and their metabolites, are detected (Figueira et al. 2017). These metabolites modulate NF-κB pathway, attenuate neuroinflammation, and protect endothelial and neuronal cells in vitro in BBB model. Microbiota-generated 3-hydroxtbenzoic acid (3-HBA), 3,4-dihydroxy-benzoic acid (3,4-DHBA) and related phenolic acids from dietary polyphenols modulated motor dysfunction in a Drosophila model of α-synucleopathy (Ho et al. 2019), and attenuated αSyn aggregation in HEK203 cells overexpressing αSyn-A53T-CEP/YFP (Yamasaki et al. 2020). These results suggest the association of gut microbiota with the bioavailability and bioactivity of polyphenols in the brain.
Most phytochemicals have biphasic either protective or promoting functions in neurodegeneration. Bioactive polyphenols inhibit Bcl-2 and Bcl-xL, induce Bax oligomerization, downregulate NF-κB signal pathway, induce the mPTP opening and apoptosis in cancer cells (Gogada et al. 2011). Dual functions of phytochemicals in mitochondrial death signal pathways depend on their structure, concentrations, redox activities and amphipathic properties of polyphenols and mitochondrial redox state (De Marchi et al. 2009). The narrow therapeutic window of polyphenols caused by their ambivalent functions make the beneficial effects less reproducible in clinical trials. The pharmacokinetical properties of phytochemicals should be studied in more details.
Abbreviations
- ARE:
-
Antioxidant responsive element
- ALP:
-
Autophagy-lysosome pathway
- αSyn:
-
α-Synuclein
- GCase:
-
Glucocerebrosidase
- HMGB1:
-
High-mobility group box 1
- MMP:
-
Mitochondrial membrane permeabilization
- mPTP:
-
Mitochondrial permeability transition pore
- RPCT:
-
Randomized, placebo-controlled trial
- TSPO:
-
The outer membrane translocator protein 18 kDa
- UPDRS:
-
Unified Parkinson’s Disease Rating Scale
- UPS:
-
Ubiquitin–proteasome system
References
Ahmed T, Raza SH, Maryam A et al (2016) Ginsenoside Rb1 as neuroprotective agents: a review. Brain Res Bull 125:30–43
Ahsan N, Mishra S, Jain MK, Surolia A, Gupta S (2015) Curcumin pyrazole and its derivative (N-(3-nitrophenylpyrazole) curcumin inhibit aggregation, disrupt fibrils and modulate toxicity of wild type and mutant α-synuclein. Sci Rep 5:9862
Arbo BD, Andre-Miral C, Nasre-Nasser RG et al (2020) Resveratrol derivatives as potential treatments for Alzheimer’s and Parkinson’s disease. Front Aging Neurosci 12:103
Ardah MT, Paleologou KE, Lv G et al (2015) Ginsenoside Rb1 inhibits fibrillation and toxicity of alpha-synuclein and disaggregates preformed fibrils. Neurobiol Dis 74:89–101
Ascherio A, Zhang SM, Hernan MA et al (2001) Prospective study of caffeine consumption and risk of Parkinson’s disease in men and women. Ann Neurol 50(1):56–63
Barichella M, Cereda E, Cassani E et al (2017) Dietary habits and neurological features of Parkinson’s disease patients: implications for practice. Clin Nutr 36(4):1054–1061
Barker RA, Björklund A, Gash DM et al (2020) GDNF and Parkinson’s disease: where next? A summary from a recent workshop. J Parkinsons Dis 10(3):875–891
Bastianetto S, Menard C, Qurion R (2015) Neuroprotective action of resveratrol. Biochim Biophys Acta 1852(6):1195–1201
Bieschke J, Russ J, Friedrich RP, Ehrnhoefer DE, Wobst H, Neugebauer K, Wanker EE (2010) EGCG remodels mature α-synuclein and amyloid-β fibrils and reduces cellular toxicity. Proc Natl Acad Sci U S A 107(17):7710–7715
Billingsley K, Barbosa IA, Bandres-Ciga S et al (2019) Mitochondria function associated genes contribute to Parkinson’s disease risk and later age at onset. NPJ Parkinson Dis 5:8
Braak H, Tredici KD, Rüb U, de Vos RAI, Jansen Steur ENH, Braak E (2003) Staging of brain pathology related sporadic Parkinson’s disease. Neurobiol Aging 24(2):197–211
Burbulla LT, Song P, Mazzulli JR et al (2017) Dopamine oxidation mediates mitochondrial and lysosomal dysfunction in Parkinson’s disease. Science 357(6357):1255–1261
Caruana M, Högen T, Levin J, Hillmer A, Giese A, Vassallo N (2011) Inhibition and disaggregation of α-synuclein oligomers by natural polyphenol compounds. FEBS Lett 585(8):1113–1120
Chen C, Vincent AE, Blain AP, Smith AL, Turnbull DM, Reeve AK (2020) Investigation of mitochondrial biogenesis defects in single substantia nigra neurons using post-mortem human tissues. Neurobiol Dis 134:104631
Cryan JF, O’Riordan KJ, Cowan CSM et al (2019) The microbiota-gut-brain axis. Physiol Rev 99(4):1877–2013
Cuervo AM, Stefanis L, Fredenburg R, Lansbury PT, Sulzer D (2004) Impaired degradation of mutant α-synuclein by chaperone-mediated autophagy. Science 305(5688):1292–1295
Das S, Mitrovsky G, Vasanthi H, Das DK (2014) Antiaging properties of a grape-derived antioxidant are regulated by mitochondrial balance of fission and fission leading to mitophagy triggered by a signaling network of Sirt1-Sirt3-Foxo3-Pink1-Parkin. Oxid Med Cell Longev 2014:345105
De Marchi U, Biasutto L, Garbisa S, Toninello A, Zorratti M (2009) Quercetin can act either as an inhibitor or an inducer of the mitochondrial permeability transition pore: a demonstration of the ambivalent redox character of polyphenols. Biochim Biophys Acta 1787(12):1425–1432
Devi L, Raghavendran V, Prabhu BM, Avadhani NG, Anandatheerthavarada HK (2008) Mitochondrial import and accumulation of α-synuclein impair complex I in human dopaminergic neuronal cultures and Parkinson disease brain. J Biol Chem 283(14):9089–9100
Dos Santos TW, Pereira QC, Teixeira L, Gambero A, Villena JA, Ribeiro ML (2018) Effects of polyphenols on thermogenesis and mitochondrial biogenesis. Int J Mol Sci 19(9):2757
Ehrnhoefer DE, Bieschke J, Boeddrich A et al (2008) EGCG redirects amyloidogenic polypeptides into unstructured, off-pathway oligomers. Nat Struct Mol Biol 15(6):558–566
Espay AJ, Brundin P, Lang AE (2017) Precision medicine for disease modifying in Parkinson disease. Nat Rev Neurol 13(2):119–126
Fanaei H, Khayat S, Kasaeian A, Javadimehr M (2016) Effect of curcumin on serum brain-derived neurotrophic factor levels in women with premenstrual syndrome: a randomized, double-blind, placebo-controlled trial. Neuropeptides 56:25–31
Fereshtehnejad SM, Yao C, Pelletier A, Montplaisir JY, Gagnon JF, Postuma RB (2019) Evolution of prodromal Parkinson’s disease and dementia with Lewy bodies: a prospective study. Brain 142(7):2051–2067
Ferretta A, Gaballo A, Tanzarella P et al (2014) Effect of resveratrol on mitochondrial function: implications in parkin-associated familiar Parkinson’s disease. Biochim Biophys Acta 1842(7):902–915
Figueira I, Garcia G, Pimao RC et al (2017) Polyphenols journey through blood-brain barrier towards neuronal protection. Sci Rep 7(1):11456
Filomeni G, Graziani I, De Zio D, Dini L, Centonze D, Rotilio G, Ciriolo MR (2012) Neuroprotection of kaempferol by autophagy in models of rotenone-mediated acute toxicity: possible implications for Parkinson’s disease. Neurobiol Aging 33(4):767–785
Furukawa Y, Vigouroux S, Wong H et al (2002) Brain proteasomal function in sporadic Parkinson’s disease and related disorders. Ann Neurol 51(6):779–782
Gao X, Cassidy A, Schwarzschild MA, Rimm EB, Ascherio A (2012) Habitual intake of dietary flavonoids and risk of Parkinson disease. Neurology 78(15):1138–1145
Gavrilova SI, Preuss UW, Wong JW, Hoerr R, Kaschel R, Bachinskaya N, GIMCIPlus Study Group (2014) Efficacy and safety of Ginkgo biloba extract EGb 761 in mild cognitive impairment with neuropsychiatric symptoms: a randomized, placebo-controlled, double-blind, multi-center trial. Int J Geriatr Psychiatry 29(10):1087–1095
Gogada R, Prabhu V, Amadori M, Scott R, Hashmi S, Chandra D (2011) Resveratrol induced p53-independent, X-linked inhibitor of apoptosis protein (XIAP)-mediated Bax protein oligomerization on mitochondria to initiate cytochrome c release and caspase activation. J Biol Chem 286(33):28749–28760
Goto S, Kogure K, Abe K, Kimura Y, Kitahama K, Yamashita E, Terada H (2001) Efficient radical trapping at the surface and inside the phospholipid membrane is response for highly potent antiperoxidative activity of the carotenoid astaxanthin. Biochim Biophys Acta 1512(2):251–258
Gundimeda U, McNeill TH, Fan TK, Deng R, Rayudu D, Chen Z, Cadenas E, Gopalakrishna R (2014) Green tea catechins potentiate the neurogenic action of brain-derived neurotrophic factor: role of 67-kDa laminin receptor and hydrogen peroxide. Biochem Biophys Res Commun 445(1):218–224
Guo YJ, Dong SY, Cui XX et al (2016) Resveratrol alleviates MPTP-induced motor impairments and pathological changes by autophagic degradation of α-synuclein via SIRT1-deacetylated LC3. Mol Nutr Food Res 60(10):2161–2175
Han YS, Bastianetto S, Dumont Y, Quirion R (2006) Specific plasma membrane binding sites for polyphenols, including resveratrol, in the rat brain. J Pharmacol Exp Ther 318(1):228–245
He J, Xiang Z, Zhu X et al (2016) Neuroprotective effects of 7,8-dihydroxyflavone on midbrain dopaminergic neurons in MPP+-treated monkey. Sci Rep 6:34339
Henchcliffe C, Beal MF (2008) Mitochondrial biology and oxidative stress in Parkinson disease pathogenesis. Nat Clin Pract Neurol 4(11):600–609
Henriquez G, Comez A, Guerrero E, Narayan M (2020) Potent role of natural polyphenols against protein aggregation toxicity: in vitro, in vivo, and clinical studies. ACS Chem Neurosci 11(19):2915–2934
Higashida K, Kim SH, Jung SR, Asaka M, Holloszy JO, Han DH (2013) Effects of resveratrol and Sirt1 on PGC-1α activity and mitochondrial biogenesis: a reevaluation. PLoS Biol 11(7):e1001603
Ho L, Zhao D, Ono K et al (2019) Heterogeneity in gut microbiota drive polyphenol metabolism that influences α-synuclein misfolding and toxicity. J Nutr Biochem 64:170–181
Holczer M, Besze B, Zambo V, Csala M, Banhegyi G, Kapuy O (2018) Epigallocatechin-3-gallate (EGCG) promotes autophagy-dependent survival via influencing the balance of mTOR-AMPA pathways upon endoplasmic reticulum stress. Oxid Med Cell Longev 2018:6721530
Huang X, Li N, Pu Y, Zhang T, Wang B (2019) Neuroprotective effects of ginseng phytochemicals: recent perspectives. Molecules 24(16):2939
Huhn S, Beyer F, Zhang R et al (2018) Effects of resveratrol on memory performance, hippocampus connectivity and microstructure in older adults—a randomized controlled trial. Neuroimage 174:177–190
Hwang SL, Yen GC (2011) Effects of hesperetin against oxidative stress via ER- and TrkA-mediated actions in PC12 cells. J Agric Food Chem 59(10):5779–5785
Jha NN, Ghosh D, Das S et al (2016) Effect of curcumin analogs on α-synuclein aggregation and cytotoxicity. Sci Rep 6:28511
Jin CF, Shen SR, Zhao BL (2001) Different effects of five catechins on 6-hydroxydopamine-induced apoptosis in PC12 cells. J Agric Food Chem 49(12):6033–6038
Jinsmaa J, Isonaka R, Sharabi Y, Goldstein DS (2020) 3,4-Dihydroxyphenyl-acetaldehyde is more efficient than dopamine in oligomerizing and quinonizing α-synuclein. J Pharmacol Exp Ther 372(2):157–165
Kaur N, Chugh H, Sakharkar MK, Dhawan U, Chidambaram SB, Chandra R (2020) Neuroinflammation mechanisms and phytotherapeutic intervention: a systemic review. ACS Chem Neurosci 11(22):3707–3731
Kumar S, Kumar R, Kumari M, Kumari R, Saha S, Bhavesh NS, Maiti TK (2021) Ellagic acid inhibits α-synuclein aggregation at multiple stages and reduces its cytotoxicity. ACS Chem Neurosci 12(11):1919–1930
Kurauchi Y, Hisatsune A, Isohama Y, Mishima S, Katsuki H (2012) Caffeic acid phenethyl ester protects nigral dopaminergic neurons via dual mechanisms involving haem oxygenase-1 and brain-derived neurotrophic factor. Br J Pharmacol 166(3):1151–1169
Lee H, James WS, Cowley SA (2017) LRRK2 in peripheral and central nervous system innate immunity: its link to Parkinson’s disease. Biochem Soc Trans 45(1):131–139
Lewadowska U, Szewczyk K, Hrabec E, Janecka A, Gorlach S (2013) Overview of metabolism and bioavailability enhancement of polyphenols. J Agric Food Chem 61(50):12183–12199
Li XH, Dai CF, Chen L, Zhou WT, Han HL, Domg ZF (2016) 7,8-Dihydroxyflavone ameliorates motor deficits via suppressing α-synuclein expression and oxidative stress in the MPTP-induced mouse model of Parkinson’s disease. CNS Neurosci Ther 22(7):617–624
Li J, Chen L, Li G et al (2020) Sub-acute treatment of curcumin derivative J147 ameliorates depression-like behavior through 5-HT1A-mediated cAMP signaling. Front Neurosci 14:701
Lim H, Min DS, Park H, Kim HP (2018) Flavonoids interfere with NLRP3 inflammasome activation. Toxicol Appl Pharmacol 355:93–102
Lin CY, Tsai CW (2019) PINK1/parkin-mediated mitophagy is related to neuroprotection by carnosic acid in SH-SH5Y cells. Food Chem Toxicol 125:430–437
Liu S, Sawada T, Lee S et al (2012) Parkinson’s disease-associated kinase PINK1 regulates Miro protein level and axonal transport of mitochondria. PLoS Genet 8(3):e1002537
Liu X, Obianyo O, Chan CB et al (2014) Biochemical and biophysical investing of the brain-derived neurotrophic factor mimetic 7,8-dihydroxyflavone in the binding and activation of the TrkB receptor. J Biol Chem 289(40):27571–27584
Lopresti A, Maes M, Maker G, Hood SD, Drummond PD (2014) Curcumin for the treatment of major depression: a randomized, double-blind, placebo controlled study. J Affect Disord 167:368–375
Lorenzen N, Nielsen SB, Yoshimura Y et al (2014) How epigallocatechin gallate can inhibit α-synuclein oligomer toxicity in vitro. J Bol Chem 289(31):21299–21310
Ludtmann MHR, Angelova PR, Horrocks MH et al (2018) α-Synuclein oligomers interact with ATP synthase and open the permeability transition pore in Parkinson’s disease. Nat Commun 9(1):2294
Lv R, Du L, Liu X, Zhou F, Zhang Z, Zhang L (2019) Rosmarinic acid attenuates inflammatory responses through inhibiting HMGB1/TLR4/NF-κB signal pathway in a mouse model of Parkinson’s disease. Life Sci 223:158–165
Maclennan KM, Darlington CL, Smith PF (2002) The CNS effects of Ginkgo biloba extracts and gingolide B. Prog Neurobiol 67(3):235–257
Manzoni C, Lewis PA (2013) Dysfunction of the autophagy/lysosomal degradation pathway is a shared feature of the genetic synucleinopathies. FASEB J 27(9):3424–3429
Mohammad-Beigi H, Aliakbari F, Sahin C et al (2019) Oleuropein derivatives from olive fruit extracts reduce α-synuclein fibrillation and oligomer toxicity. J Biol Chem 294(11):4215–4232
Mohankumar T, Chandramohan V, Lalithamba HS et al (2020) Design and molecular dynamic investigations of 7,8-dihydroxyflavone derivatives as potential neuroprotective agents against alpha-synuclein. Sci Rep 10(1):599
Murota K, Nakamura Y, Uehara M (2018) Flavonoid metabolism: the interaction of metabolites and gut microbiota. Biosci Biotechnol Biochem 82(4):600–610
Naoi M, Inaba-Hasegawa K, Shamoto-Nagai M, Maruyama W (2017) Neurotrophic function of phytochemicals for neuroprotection in aging and neurodegenerative disorders: modulation of intracellular signaling and gene expression. J Neural Transm 24(12):1515–1527
Naoi M, Wu Y, Shamoto-Nagai M, Maruyama W (2019) Mitochondria in neuroprotection by phytochemicals: bioactive polyphenols modulate mitochondrial apoptosis system, function and structure. Int J Mol Sci 20(10):2451
Naoi M, Maruyama W, Shamoto-Nagai M (2020) Rasagiline and selegiline modulate mitochondrial homeostasis, intervene apoptosis system and mitigate α-synuclein cytotoxicity in disease-modifying therapy for Parkinson’s disease. J Neural Transm 127(2):131–147
Nebrisi EE, Javed H, Ojha SK, Oz M, Shehab S (2020) Neuroprotective effects of curcumin on the nigrostriatal pathway in a 6-hydroxydopamine-induced rat model of Parkinson’s disease by α-7-nicotinic receptors. Int J Mol Sci 21(19):7329
Neshatdoust S, Saunders C, Castle SM et al (2016) High-flavonoid intake induces cognitive improvements linked to changes in serum brain-derived neurotrophic factor: two randomized controlled trials. Nutr Healthy Aging 4(1):81–93
Nieman DC, Williams AS, Shanely RA, Jin F, McAnulty SR, Triplett NT, Austin MD, Henson DA (2010) Quercetin’s influence on exercise performance and muscle mitochondrial biogenesis. Med Sci Sports Exerc 42(2):338–345
Olanow CW, Rascol O, Hauser R et al (2009) A double-blind, delayed-start trial of rasagiline in Parkinson’s disease. N Engl J Med 361(13):1268–1278
Olanow CW, Kieburtz K, Katz R (2017) Clinical approaches to the development of a neuroprotective therapy for PD. Exp Neurol 298(Pt B):246–251
Pan T, Kondo S, Le W, Jankovic J (2008) The role of autophagy-lysosome pathway in neurodegeneration associated with Parkinson’s disease. Brain 131(Pt 8):1969–1978
Parain K, Murer MG, Yan Q, Faucheux B, Agid Y, Hirsch E, Raisman-Vozari R (1999) Reduced expression of brain-derived neurotrophic factor protein in Parkinson’s disease substantia nigra. NeuroReport 10(3):557–561
Parkinson Study Group QE3 investigators (2014) A randomized clinical trial of high-dose coenzyme Q10 in early Parkinson disease: no evidence of benefit. JAMA Neurol 71(5):543–552
Poole AC, Thomas RE, Andrews LA, McBride HM, Whitworth AJ, Pallanck LJ (2008) The PINK1/Parkin pathway regulates mitochondrial morphology. Proc Natl Acad Sci U S A 105(5):1638–1643
Rainey-Smith SR, Brown B, Sohrabi HR, Shah T, Goozee KG, Cupta VB, Martins RN (2016) Curcumin and cognition: a randomized, placebo-controlled, double-blind study of community-dwelling older adults. Br J Nutr 115(12):2106–2113
Reyes-Izquierdo T, Nemzer B, Shu C, Argumedo R, Keller R, Piertrzkowski Z (2013) Modulatory effect of coffee fruit extract on plasma levels of brain-derived neurotrophic factor in healthy subjects. Br J Nutr 110(3):420–425
Rostovtseva T, Gurnev PA, Protchenko O, Hoogerheide DP, Yap TL, Philpott CC, Lee JC, Bezrukov SM (2015) α-Synuclein shows high affinity interaction with voltage-dependent anion channel, suggesting mechanisms of mitochondrial regulation and toxicity in Parkinson disease. J Biol Chem 290(30):18467–18477
Sadowska-Krepa E, Klapcinska B, Pokora I, Domaszewski P, Kempa K, Podgorski T (2017) Effects of six-week Ginkgo biloba supplementation on aerobic performance, blood pro-antioxidant balance, and serum brain-derived neurotrophic factor in physically active men. Nutrients 9(8):803
Sampson TR, Debelius JW, Thron T et al (2016) Gut microbiota regulate motor deficits and neuroinflammation in a model of Parkinson’s disease. Cell 167(6):1469–1480
Santos D, Esteves AR, Silva D, Januario C, Cardoso SM (2015) The impact of mitochondrial fusion and fission modulation in sporadic Parkinson’s disease. Mol Neurobiol 52(1):573–586
Sarubbo F, Esteban S, Miralles A, Moranta D (2018) Effects of resveratrol and other polyphenols on Sirt1: relevance to brain function during aging. Curr Neuropharmacol 16(2):126–136
Scrivo A, Bourdenx M, Pampliega O, Cuervo AM (2018) Selective autophagy as a potential therapeutic target for neurodegenerative disorders. Lancet Neurol 17(9):802–825
Sekikawa T, Kizawa Y, Li Y, Takara T (2020) Cognitive function improvement with astaxanthin and tocotrienol intake: a randomized, double-blind, placebo-controlled study. J Clin Biochem Nutr 67(3):307–316
Shishtar E, Rogers GT, Blumberg JB, Au R, DeCarli C, Jacques P (2020) Flavonoid intake and MRI markers of brain health in the Framingham offspring cohort. J Nutr 150(6):1545–1553
Singh P, Bhat R (2019) Binding of noradrenaline to native and intermediate states during the fibrillation of α-synuclein leads to the formation of stable and structured cytotoxic species. ACS Chem Neurosci 10(6):2741–2755
Sun X, Xiong Z, Zhang Y et al (2012) Harpagoside attenuates MPTP/MPP+ induced dopaminergic neurodegeneration and movement disorder via elevating glial cell line-derived neurotrophic factor. J Neurochem 120(6):1072–1083
Sun W, Wang X, Hou C et al (2017) Oleuropein improves mitochondrial function to attenuate oxidative stress by activating the Nrf2 pathway in the hypothalamic paraventricular nucleus of spontaneously hypertensive rats. Neuropharmacology 113(Pt A):556–566
Tatsuta T, Langer T (2008) Quality control of mitochondria: protection against neurodegeneration and ageing. EMBO J 27(2):306–314
Taub PR, Ramairez-Sanchez I, Patel M et al (2016) Beneficial effects of dark chocolate on exercise capacity in sedentary subjects: underlying mechanisms. A double blind, randomized, placebo controlled trial. Food Funct 7(9):3686–3693
Tewari D, Ahmed T, Chirasani VR, Singh PK, Maji SK, Senapati S, Bera AK (2015) Modulation of the mitochondrial voltage dependent anion channel (VDAC) by curcumin. Biochim Biophys Acta 1848(Pt A):151–158
Tian M, Xie Y, Meng Y et al (2019) Resveratrol protects cardiomyocytes against anoxia/reoxygenation via dephosphorylation of VDAC1 by Akt-GSK3 β pathway. Eur J Pharmacol 843:80–87
Trinh D, Israwi AR, Arathoon LR, Gleave JA, Nash JE (2021) The multi-faceted role of mitochondria in the pathology of Parkinson’s disease. J Neurochem 156(6):715–752
Valenti D, De Rasmo D, Signorile A et al (2013) Epigalocatchin-3-gallate prevents oxidative phosphorylation deficit and promotes mitochondrial biogenesis in human cells from subjects with Down’s syndrome. Biochim Biophys Acta 1832(4):542–552
Vauzour D, Vafeiadou K, Rice-Evans C, Williams RJ, Spencer JPE (2007) Activation of pro-survival Akt and ERK1/2 signaling pathways underlie the anti-apoptotic effects of flavanones in cortical neurons. J Neurochem 103(4):1355–1367
Vogiatzi T, Xilouri M, Vekrellis K, Stefanis L (2008) Wild type α-synuclein is degraded by chaperone-mediated autophagy and macroautophagy in neuronal cells. J Biol Chem 284(35):23542–23556
Wang ZY, Liu JY, Yang CB, Malampati S, Huang YY, Li MX, Li M, Song JX (2017) Neuroprotective natural products for the treatment of Parkinson’s disease by targeting the autophagy-lysosome pathway: a systematic review. Phytother Res 31(8):1119–1127
Whone A, Luz M, Boca M et al (2019) Randomized trial of intermittent intraputamenal glial cell line-derived neurotrophic factor in Parkinson’s disease. Brain 142(3):512–525
Wightman E, Haskell CF, Forster JS, Veasey RC, Kennedy DO (2012) Epigallocatechin gallate, cerebral blood flow parameters, cognitive performance and mood in healthy humans: a double-blind, placebo-controlled, crossover investigation. Hum Psychopharmacol 27(2):177–186
Witte AV, Kerti L, Margulies DS, Flöel A (2014) Effects of resveratrol on memory performance, hippocampal functional connectivity, and glucose metabolism in healthy older adults. J Neurosci 34(23):7862–7870
Wu Y, Shamoto-Nagai M, Maruyama W, Osawa T, Naoi M (2017) Phytochemicals prevent mitochondrial membrane permeabilization and protect SH-SY5Y cells against apoptosis induced by PK11195, a ligand for outer membrane translocator protein. J Neural Transm 124(1):89–98
Xu SL, Bi CWC, Choi RCY, Zhu KY, Miernisha A, Dong TTX, Tsim KWK (2013) Flavonoids induce the synthesis and secretion of neurotrophic factors in cultured rat astrocytes: a signaling response mediated by estrogen receptor. Evid Based Complement Alternat Med 2013:127075
Yamazaki TR, Ono K, Ho L, Pasinetti GM (2020) Gut microbiome-modified polyphenolic compounds inhibit α-synuclein seeding and spreading in α-synucleinopathy. Front Neurosci 14:398
Yang F, Wolk A, Hakansson N, Pedersen NL, Wirdefeld K (2017a) Dietary antioxidants and risk of Parkinson’s disease in two population-based cohorts. Mov Disord 32(11):1631–1636
Yang JE, Rhoo KY, Lee S, Lee JT, Park JH, Bhak G, Paik SR (2017b) EGCG-mediated protection of the membrane disruption and cytotoxicity caused by the ‘active oligomer’ of α-synuclein. Sci Rep 7(1):17945
Yang Y, Han C, Guo L, Guan Q (2018) High expression of the HMGB1-TLR4 axis and its downstream signaling factors in patients with Parkinson’s disease and the relationship of pathological staging. Brain Behav 8(4):e00948
Yao Y, Tang Y, Wei G (2020) Epigallocatechin gallate destabilizes α-synuclein fibril by disrupting the E46–E80 salt-bridge and inter-protofibril interface. ACS Chem Neurosci 11(24):4351–4361
Yoritake A, Kawajiri S, Yamamoto Y et al (2015) Randomized, double-blind, placebo-controlled pilot trial of reduced coenzyme Q10 for Parkinson’s disease. Parkinsonism Relat Disord 21(8):911–916
Youdim KA, Shukitt-Hale B, Joseph JA (2004) Flavonoids and the brain: Interactions at the blood–brain-barrier and their physiological effects on the central nervous system. Free Radic Biol Med 37(11):1683–1693
Zanforlin E, Zagotto G, Ribaudo G (2017) The medical chemistry of natural and semisythetic compounds against Parkinson’ and Huntington’s diseases. ACS Chem Neurosci 8(11):2356–2368
Zhang X, Wu M, Lu F, Luo N, He ZP, Yang H (2014) Involvement of α7nAcR signaling cascade in epigallocatechin gallate suppression of β-amyloid-induced apoptotic cortical neuronal insults. Mol Neurobiol 49(1):66–77
Zilocchi M, Finzi G, Lualdi M, Sessa F, Fasano M, Alberio T (2018) Mitochondrial alterations in Parkinson’s disease human samples and cellular models. Neurochem Int 118:61–72
Funding
The authors’ research of food-derived bioactive compounds is supported by the Grants-in-Aids for Scientific Research, No. 18Kk07430 (WM).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from that disclosed.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Naoi, M., Maruyama, W. & Shamoto-Nagai, M. Disease-modifying treatment of Parkinson’s disease by phytochemicals: targeting multiple pathogenic factors. J Neural Transm 129, 737–753 (2022). https://doi.org/10.1007/s00702-021-02427-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-021-02427-8