Abstract
Microglia are the resident mononuclear immune cells of the central nervous system (CNS) and the activation of microglia contributes to the production of excessive neurotoxic factors. In particular, the overproduction of neurotoxic factors has critical effects on the development of brain injuries and neurodegenerative diseases. The human bone marrow-derived mesenchymal stem cells (hBM-MSCs) have blossomed into an effective approach with great potential for the treatment of neurodegenerative diseases and gliomas. The present study aimed to investigate the mechanism behind the therapeutic effect of hBM-MSCs on the activation of microglia in vitro. Specifically, the hBM-MSCs significantly inhibited the proliferation of lipopolysaccharide-activated microglial cells (LPS)-activated microglial cells. Additionally, we investigated whether the adenosine-monophosphate-activated protein kinase signaling (AMPK) pathway was involved in this process. Our data demonstrated that hBM-MSCs significantly increased the phosphorylated AMPK in LPS-activated microglial cells. In addition, our study indicated the inhibitory effect of hBM-MSCs on the pro-inflammatory mediators and oxidative stress by the AMPK pathway in LPS-activated microglial cells. These results could shed light on the understanding of the molecular basis for the inhibition of hBM-MSCs on LPS-activated microglial cells and provide a molecular mechanism for the hBM-MSCs implication in brain injuries and neurodegenerative diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Microglia, the resident immune cells in the CNS, play a role in the maintenance of homeostasis and responses to neuroinflammation (Dheen et al. 2007). In the normal brain, microglia are in a homeostatic state (Zhan et al. 2019), expressing low levels of most immune receptors, such as pattern recognition receptors, chemokine receptors, and major histocompatibility complex molecules, which are all essential to the initiation and propagation of immune responses (Kumar et al. 2018; Borst et al. 2018). When activated, microglia undergo morphological, phenotypic and functional changes. Activated microglia exhibit detrimental effects involving the overproduction of pro-inflammatory mediators and neuro-toxic cytokines (Lee et al. 2005; Graeber et al. 2011) including nitric oxide (NO), reactive oxygen species (ROS), interleukin (IL)-1β, IL-6 and tumor necrosis factor (TNF)-α. What is more, neuroinflammation is closely related with the pathogenesis and progress of brain injuries and neurodegenerative diseases including Alzheimer’s disease (Franco and Fernandez-Suarez 2015; Blaylock 2017). Several studies (Lim et al. 2017; Carniglia et al. 2017) indicated that inhibition of microglial activation was an effective strategy for many injuries and diseases including stroke, multiple sclerosis, neurodegenerative diseases, along with brain trauma. Thus, it is important to explore a novel therapeutic approach that would downregulate microglial activation and mitigate the progression of inflammation-related neuronal diseases.
The advances in mesenchymal stem cells (MSCs) (Trallori et al. 2019) based cell therapy are revolutionizing the paradigm of tissue repair and regenerative medicine and provide an ideal option in the preclinical and clinical studies. The hBM-MSCs possess an extended degree of plasticity, high proliferation, and differentiation capacity (Steens and Klein 2018). Encouragingly, multi-potent MSCs have the potential to differentiate into neurons and glial cells (Her et al. 2013). What is more, some clinical trials have proved that hBM-MSCs can effectively alleviate neurological diseases (Oh et al. 2015). Additionally, the hBM-MSCs have the advantages of autologous sources and abundance of cells (Yan et al. 2013), providing a promising tool for cell-based therapies of brain injuries and neurodegenerative diseases (Chakari-Khiavi et al. 2019; Drela et al. 2013). However, the underlying mechanisms are not yet fully understood. Considering the close relationship between glial activation and brain injuries and neurodegenerative diseases, further explorations are required to better understand how hBM-MSCs regulate microglial activation.
Lipopolysaccharide (LPS), a bacterial endotoxin a constituent of the outer membrane of Gram-negative bacteria, can trigger via microglia activation and stimulates the neuroinflammatory pathway (Subedi et al. 2017). In this study, the hBM-MSCs were evaluated for their effectiveness on LPS-activated microglial cells. We intended to investigate whether hBM-MSCs accommodate LPS-activated microglial cells and as well as possible repair mechanisms for neuroimmune responses, focusing on its role in the signaling pathway mediating the effect of hBM-MSCs on LPS-activated microglial cells.
Materials and methods
Reagents and antibodies
The Cell Counting Kit-8, Compound C (a specific AMPK inhibitor), AICAR (a specific AMPK activator) and Annexin V-FITC/PI Apoptosis Detection Kit were from Sigma (St. Louis, MO, USA). Enhanced BCA Protein Assay Kit and Annexin V-FITC/PI Apoptosis Detection Kit were from Beyo-time Biotechnology (Haimen, China). The primary antibodies including phospho-AMPKα (1:1000), AMPKα (1:2000), Bcl-2 (1:2000), Bax (1:2000), cleaved caspase-3 (1:1000), CD11b/c (1:2000), and p-p47phox (1:1000) were purchased from Abcam (Cambridge, MA, USA). The iTaqTM Universal SYBR Green was purchased from Bio-Rad Laboratories (Bio-Rad Laboratories, Inc., Hercules, CA, USA).
Cell culture
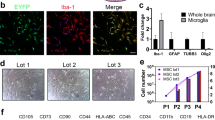
Microglial cells were isolated from 0- to 24-h-old SD rats by a modification of a previously described method (Togna et al. 2013). Briefly the cortices were harvested and digested for 20 min at 37 °C in 0.25% trypsin and for further 5 min in presence of with Dulbecco’s modified Eagle’s medium–F12 nutrient mixture (DMEM–F12) with 10% fetal bovine serum (10% FBS) and antibiotics (100 U/ml of penicillin and 100 g/ml of streptomycin). After 10 and 14 days from dissection, microglia was detached from the astrocyte monolayer by shaking, and the cells re-suspended in DMEM–F12 (10% FBS and antibiotics). Thereafter the cells were placed at a density of 5 × 105 cells/ml, incubated at 37 °C in a humidified atmosphere containing 5% CO2. Purity of microglial cell populations (> 98%) were verified by staining with Iba-1 antibody (Iba-1, 1:1000; Wako Chemicals Inc., Richmond, VA) (Bollinger et al. 2016).
Human bone marrow-derived mesenchymal stem cells were from healthy persons between 40 and 45 years of age who voluntarily donated bone marrow stem cells. Briefly, mesenchymal stem cells were collected into appropriately supplemented DMEM–F12 at 37 °C/5% CO2 fully humidified atmosphere. The expressions of hBM-MSC surface markers cluster of differentiation (CD14, CD34, CD45, CD90, CD73, and CD105) were detected by BD FACS Calibur™ (BD Biosciences, San Jose, CA, USA), cells were characterized as having high expression of these positive markers (CD90, CD73 and CD105) and low expression of the negative markers (CD14, CD34 and CD45) (Qiao et al. 2018). Cells that had grown to 80–90% confluence were used for all the experiments. After 24 h, the medium was collected and centrifuged at 300×g for 3 min to remove debris before use.
Co-culture system and treatment
The microglial cells were activated by the treatment with 1 ug/mL LPS. To evaluate the effects of the hBM-MSCs on LPS-activated microglial cells, indirect co-culture in Transwell chamber (24-mm diameter, 0.4-mm pore size; Corning) was used. Prior to the addition of LPS, AICAR, or Compound C to the medium, the microglial cells were inoculated in the lower part and the hBM-MSCs were inoculated in the upper part at a 1:1 ratio. The cell numbers were evaluated using microscopy and viability was determined by the trypan blue exclusion assay. Samples were collected after culturing for 24, 48, or 72 h.
Cell proliferation assay
Cell proliferation was determined using the sensitive colorimetric assay, the Cell Counting Kit-8 (CCK-8; Sigma-Aldrich, St. Louis, MO, USA). The coculture cells were collected after culturing for 24, 48, or 76 h. The CCK-8 reagent was added to the lower chamber containing activated microglial cells in the LPS-activated microglial cells group and the coculture group and incubated for 2 h according to the manufacturer’s protocol.
Western blot analysis
The LPS-activated microglial cells were harvested at the indicated time-points and lysed in RIPA buffer for 30 min. Cell lysates were centrifuged (10,000g) at 4 °C for 20 min and the supernatants were quantified for total protein concentration by using an Enhanced BCA Protein Assay Kit (Beyo-time Biotechnology, Haimen, China) according to the manufacturer’s protocol. Western blot analysis was performed as described previously (Zhai et al. 2015). Briefly, The LPS-activated microglial cells lysate (25 μg/lane) was separated by SDS-PAGE and the proteins were transferred onto a nitrocellulose membrane. Target proteins were detected by primary antibodies against phospho-AMPKα, AMPKα, Bcl-2, Bax, cleaved caspase-3, and CD11b/c. After incubating with horseradish peroxidase (HRP)-conjugated secondary antibodies, immunoreactive bands were visualized by chemiluminescence reagents (ECL, Amersham).
RNA isolation and real-time PCR
The expression levels of CD11b/c and p47phox genes were examined by RT-PCR. Total RNA was isolated from cells using TRIzol reagent (Invitrogen Life Technologies, Carlsbad, CA, USA) and quantified by ultraviolet absorption at 260 and 280 nm. Total RNA was reverse-transcribed into cDNA using a cDNA reverse transcription kit (Takara Biotechnology Co, Ltd.) at 37 °C for 15 min, 85 °C for 5 s, and stored at − 20 °C. The products were used for two-step qPCR. The primer sequences are listed in Table 1. PCR reactions were performed with iTaqTM Universal SYBR Green. The thermocycling program was set as follows: initial denaturation at 94 °C for 10 min; 35 cycles of denaturation at 94 °C for 1 min, annealing at 55 °C for 15 s and extension at 70 °C for 15 s; and a final extension at 70 °C for 5 min. The cycle threshold (Ct) values were normalized against the housekeeping gene GAPDH and analyzed by using the ΔΔCt method. The values were expressed as fold change in mRNA level of target gene relative to GAPDH.
ELISA assay
Levels of TNF-α, IL-1β, IL-6, and PEG2 were quantified using commercial enzyme-linked immunosorbent assay (ELISA) kits specific for rat according to the instructions (Enzo Life Sciences, Farmingdale, NY, USA). Intensity of color was measured at 450 nm using a microplate reader (TECAN, Mannedorf, Switzerland). The concentration of protein was determined by using standard curve.
Assay of NADPH oxidase activity
NADPH oxidase activity was measured using lucigenin as described previously [16]. Briefly, the coculture cells or the LPS-activated microglial cells were harvested and centrifuged at 400×g for 10 min at 4 °C, the cell pellet was kept on ice after re-suspended by 35 µl/per well of ice-cold RPMI-1640 medium. Then the NOX activity was measured in cell homogenates in a reaction mixture that contained NADPH (1 µM) or lucigenin (20 µM), 5 µl of cell suspension and a final 200 µl volume of pre-warmed (37 °C) RPMI-1640 medium. The chemiluminescence was continuously recorded for 12 min, and the specific enzyme activity was calculated as counts per million cells.
Measurement of oxidative stress
The amount of reactive oxygen species (ROS) and malondialdehyde (MDA), and the activities of superoxide dismutase (SOD) and glutathione peroxidase (GSH-Px) were performed according to manufacturer’s instructions. The fluorescent probe DCFH-DA was used to monitor the intracellular accumulation of ROS and the fluorescence of samples was measured using a microplate reader with 488 nm excitation. The level of MDA was expressed as (pmol/mg protein) (λ = 523 nm). The activity of SOD (U/mg protein) was expressed at 450 nm, and the activity of GSH-Px (U/mg protein) was read for the absorbance at 412 nm.
Statistical analysis
The results are obtained as the mean ± standard deviation of at least three assays and the differences between means were evaluated by using an unpaired two-sided Student’s t test. P < 0.05 was considered as significant difference.
Results
The hBM-MSCs inhibited proliferation in LPS-activated microglial cells
The Transwell coculture was used to determine the effects of hBM-MSCs on LPS-activated microglial cells. The CCK-8 assay was performed to measure the microglial cells proliferation at indicate time-points. The results in Fig. 1 showed that proliferation of microglial cells was significantly increased by the effect of LPS at 48 h and 72 h, while treatment with hBM-MSCs significantly inhibited the proliferation.
hBM-MSCs inhibited proliferation in LPS-activated microglial cells. The primary rat microglial cells with or without 1 μg/ml LPS and hBM-MSCs were seeded at a 1:1 ratio in Co-culture system for 24 h, 48 h, and 72 h, and cell viability of the primary rat microglial cells was measured using CCK-8 assay. Data (n = 3) are expressed as the mean ± standard deviation of three independent experiments. **P < 0.001 vs the control group; ##P < 0.001 vs the group treatment with LPS
The AMPK pathway was required for the inhibitory effect of hBM-MSCs in LPS-activated microglial cells
Increasing studies (Mukherjee et al. 2008) have shown that AMPK phosphorylation induces the apoptosis in astrocytes and protects normal brain cells. In our study, we hypothesized that the inhibitory effect of hBM-MSCs in LPS-activated microglial cells was through the AMPK signaling pathway. To verify this hypothesis, Western blot was performed to examine the effect of hBM-MSCs on AMPK activation in LPS-activated microglial cells. At 48 h, LPS-activated microglia displayed an approximate 35% increase in the proliferation (Fig. 1). Then the LPS-activated microglia was used to test the effect of hBM-MSCs on AMPK activation. As displayed in Fig. 2A, the hBM-MSCs increased the phosphorylated AMPK expression at 48 h.
The AMPK pathway was required for the inhibitory effect of hBM-MSCs in LPS-activated microglial cells. a Western blot analysis of phospho-AMPKα (Thr172) and AMPKα (n = 3). The cocultures and LPS-activated microglial cells were harvested after cultured for 24 h, Western blot analyses were performed. b Analyses of CD11b/c mRNA fold changes (n = 3). The cocultures and the microglial cells were pretreated with or without Compound C (10 μM) or AICAR (1 mM) for 1 h before incubation with LPS, and then cells were harvested after cultured for 48 h. The CD11b/c mRNA level was relative to GAPDH. C Western blot analysis of CD11b/c expression. **P < 0.001 vs the control group. ##P < 0.001 vs the group treatment with LPS. §P < 0.05 vs the cocultures treatment with LPS. §§P < 0.001 vs the cocultures treatment with LPS
To further confirm the role that the AMPK signaling pathway played the inhibitory effect of hBM-MSCs in LPS-activated microglial cells, we used Compound C (the specific AMPK inhibitor) and AICAR (the specific AMPK activator) to examine the expression levels of CD11b/c, the specific marker of activated microglial cells. The microglial cells were pretreated with Compound C or AICAR for 1 h before incubation with LPS and then treated with hBM-MSCs for 48 h. In Fig. 2b, as compared to the control, the result revealed that LPS increased the CD11b/c mRNA expression and hBM-MSCs reduced CD11b/c mRNA expression in the LPS-activated microglial cells, while AICAR plus hBM-MSCs showed a significant decrease the CD11b/c expression in LPS-activated microglial cells and the inhibition effect was partially counteracted by Compound C treatment. A similar trend was obtained when CD11b/c protein expression was examined (Fig. 2c). These results indicated that the inhibition effect of hBM-MSCs in LPS-activated microglial cells was partly through AMPK signaling pathway.
The AMPK pathway was involved in hBM-MSCs-induced reduction of pro-inflammatory mediators in LPS-activated microglial cells
Considering that microglia cells play an important role in the maintenance of homeostasis and responses to neuroinflammation, thus we evaluated the role of AMPK signaling pathway in hBM-MSCs-mediated immunomodulation effects of LPS-activated microglial cells. Figure 3 shows that the levels of TNF-α, IL-6, and PGE2 were markedly increased in the presence of LPS. However, hBM-MSCs significantly inhibited secretion of these factors, and the inhibitory effects were enhanced with the AMPK activator AICAR. In contrast, the hBM-MSCs-mediated inhibitory effects on the expression levels of TNF-α, IL-6, and PGE2 were partially counteracted by the AMPK inhibitor Compound C. In conclusion, these results clearly suggested that the anti-inflammatory effect of hBM-MSCs on LPS-activated microglial cells was partly mediated by the AMPK signaling pathway.
The AMPK pathway was involved in hBM-MSCs-induced reduction of pro-inflammatory mediators in LPS-activated microglial cells. The cocultures and the microglial cells were pretreated with or without Compound C (10 uM) or AICAR (1 mM) for 1 h before incubation with LPS, the supernatants were collected and measured after cultured for 48 h (n = 3). **P < 0.001 vs the control group. ##P < 0.001 vs the group treatment with LPS. §P < 0.05 vs the cocultures treatment with LPS. §§P < 0.001 vs the cocultures treatment with LPS
The hBM-MSCs inhibited the NADPH-oxidase activity and p47phox expression by inducing the activation of AMPK signaling pathway
Accumulating evidences indicate the NADPH oxidase family are critical intermediates in the physiology and pathology of nervous system (Crosas-Molist and Fabregat 2015; Haslund-Vinding et al. 2017). Since we have confirmed that the AMPK signaling pathway contributed to the inhibitory effect of hBM-MSCs on LPS-activated microglial cells, we intended to study whether the AMPK signaling pathway was involved in regulating NADPH-oxidase activity and p47phox expression by the hBM-MSCs in LPS-activated microglial cells.
As displayed in Fig. 4a, the stimulation of LPS accelerated the NADPH oxidase activity whereas the hBM-MSCs led to a significant decrease in the NADPH oxidase activity in LPS-activated microglial cells. Moreover, hBM-MSCs-mediated the inhibitory effect on NADPH oxidase activity was induced in the presence of AICAR and the inhibitory effect offered by hBM-MSCs was partially counteracted by hBM-MSCs.
hBM-MSCs inhibited NADPH-oxidase activity and p47phox expression by inducing the activation of AMPK signaling pathway. a NADPH oxidase activity was measured following treatment. b, c Analyses of p47phox expression (n = 3). The p47phox mRNA expression and protein expression were analyzed by real-time PCR and Western blot analysis, respectively. **P < 0.001 vs the control group. ##P < 0.001 vs the group treatment with LPS. §P < 0.05 vs the coculture treatment with LPS. §§P < 0.001 vs the coculture treatment with LPS
As the functional active component of the NADPH oxidase complex, p47phox, is considered to play a vital role in the activity of NADPH oxidase. Therefore, the p47phox expression was used to examine the respective signaling pathway. As shown in Fig. 4b, LPS markedly increased the mRNA level of p47phox and the effects of hBM-MSCs reduced p47phox mRNA. Notably, hBM-MSCs plus AICAR strengthened the inhibitory effect of p47phox expression and hBM-MSCs plus Compound C attenuated the effect. In addition, a similar trend was obtained when p47phox protein expression was examined by Western blot analysis (Fig. 4c). This finding encouraged us to speculate that AMPK signaling pathway was also required for the inhibition effect of hBM-MSCs on activation of NADPH oxidase.
The AMPK pathway mediated the effect of hBM-MSCs on oxidative stress in LPS-activated microglial cells
The NADPH oxidase contributed to oxidative stress during degenerative diseases. Hence, it is important to test the effect of hBM-MSCs on oxidative stress expression in LPS-activated microglial cells. Since we have revealed that the effect of hBM-MSCs on NADPH-oxidase activity and p47phox expression was partly through the AMPK signaling pathway, we intended to study whether the regulatory roles of hBM-MSCs on the activities of superoxide dismutase (SOD) and glutathione peroxidase (GSH-Px), the intracellular reactive oxygen species (ROS) production, and the level of malondialdehyde (MDA) in LPS-activated microglial cells were also mediated by this pathway.
This approach (Fig. 5) revealed that the LPS treatment resulted in a significant decrease in the activity of SOD and GSH-Px, whereas hBM-MSCs treatment could restored the SOD and GSH-Px expression level. Compared to the control, the level of MDA and intracellular ROS was remarkably increased after LPS treatment (Fig. 5). However, the LPS-induced increased MDA and intracellular ROS expression could be inhibited in hBM-MSCs-treated group. Compared to the hBM-MSCs-treated group, the AICAR enhanced the activity of SOD and GSH-Px in LPS-activated microglial cells and Compound C reversed SOD activity induced by hBM-MSCs in LPS-activated microglial cells. Additionally, AICAR attenuated the level of MDA and intracellular ROS in LPS-activated microglial, in contrast, the inhibition effects of hBM-MSCs were remarkably reverted by Compound. These results clearly suggested that the hBM-MSCs contributed to regulate oxidative stress through AMPK axis in LPS-activated microglial cells.
The AMPK pathway mediated the effect of hBM-MSCs on oxidative stress in LPS-activated microglial cells. a–d Measurement of oxidative stress (n = 3). The cocultures and the microglial cells were pretreated with or without Compound C (10 μM) or AICAR (1 mM) for 1 h before incubation with LPS, the supernatants were collected and measured after cultured for 48 h. The amount of ROS and MDA, and the activities of SOD and GSH-Px were determined. **P < 0.001 vs the control group. ##P < 0.001 vs the group treatment with LPS. §P < 0.05 vs the cocultures treatment with LPS
Discussion
Accumulating evidences reveal the microglial activation and subsequent neuroinflammatory response are implicated in brain injuries (Wilhelmsson et al. 2017) and neurodegenerative diseases (Song and Colonna 2018), such as Alzheimer’s disease, stroke and glioma. The inhibition of microglial activation and the neuroinflammatory response are considered to be an effective therapeutic approach to mitigate various brain diseases. In recent years, the BM-MSCs are regarded as an ideal candidate for application in the diseases related to human nervous system, since they offer the significant practical advantages including easy-handling in vitro, self-renewal, multipotent differentiation, and low immunogenicity (Karussis et al. 2008). Given that microglial activation has the critical role of alleviating the progression of brain diseases and BM-MSCs are the promising tool for cell-based therapies in tissue repair and regenerative medicine. This study has been concerned on establishing proofs for seeking the molecular mechanisms underlying hBM-MSCs inhibition of LPS-activated microglial cells in vitro. These data focused on talking over three aspects: (1) the hBM-MSCs inhibited LPS-activated microglial cells proliferation in vitro; (2) the hBM-MSCs had the positive effect on the phosphorylated AMPK expression in LPS-activated microglial cells; (3) hBM-MSCs contributed to suppress the produce of pro-inflammatory mediators, the NADPH-oxidase expression, and the oxidative stress through AMPK signaling pathway in LPS-activated microglial cells. Together, our study will shed light on the molecular mechanisms underlying hBM-MSCs inhibition of LPS-activated microglial cells, providing solid foundation for the hBM-MSCs application in the various brain diseases.
LPS has been often used as a proinflammogen to stimulate microglia and induce inflammatory response (Kettenmann et al. 2011). Our report indicated that hBM-MSCs inhibited the proliferation of LPS-activated microglial cells. Multiple signaling pathways have been confirmed to participate in the regulatory mechanism of on the microglial cells activation (Popiolek-Barczyk and Mika 2016; Xue et al. 2008), such as the mitogen-activated protein kinases (MAPKs) and the nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κb) signaling pathway. It is report that BMSCs can enhance the proliferation of LPS-activated microglial cells through cell cycle modulation (Jose et al. 2014). The activity of AMPK, an energy charge sensor with neuroprotective properties, negatively modulates pathological excitability in the peripheral or central nervous system (Baron et al. 2010). However, the potential effects of AMPK on microglial activation are not known. In fact, our study indicated that the AMPK pathway was required for the inhibitory effect of hBM-MSCs in LPS-activated microglial cells. In this regard, this result might provide a new clue and possibility for explaining the inhibition effect of hBM-MSCs on LPS-activated microglial cells.
Importantly, oxidative stress and neuroinflammation play critical roles in the pathological feature of the central nervous system (Cabezas et al. 2018; Lewerenz et al. 2018) and occur in response to the invasion of various pathogens. Inflammatory responses are accompanied by the induction of pro-inflammatory cytokines, such as TNF-α, interleukin (IL)-1, and IL-6. We noticed that, the generation of reactive oxygen species (ROS) are interrelated and interact on the development of the various brain diseases. What is more, NADPH oxidase signaling pathway plays a key role in the chronic neuroinflammation and neurodegenerative diseases (Hou et al. 2018). We used the specific AMPK inhibitor Compound C and the specific AMPK activator AICAR to test pro-inflammatory mediators, the NADPH-oxidase expression, and the oxidative stress in LPS-activated microglial cells. We date showed that the AMPK signaling pathway was involved in this process of the inhibitory effect of hBM-MSCs on pro-inflammatory mediators, the oxidative stress, and NADPH oxidase signaling pathway in LPS-activated microglial cells.
In summary, we have shown that hBM-MSCs markedly inhibited the proliferation of LPS-activated microglial cells. Our results demonstrated that the inhibiting effect of the hBM-MSCs on the production of pro-inflammatory mediators, the oxidative stress, and the NADPH-oxidase expression were mediated at least by the AMPK signaling pathway. Therefore, our study will provide a new molecular mechanism for the therapeutic effect of hBM-MSCs on neurological disease-related microglial activation.
References
Baron R, Binder A, Wasner G (2010) Neuropathic pain: diagnosis, pathophysiological mechanisms, and treatment. Lancet Neurol 9(8):807–819. https://doi.org/10.1016/S1474-4422(10)70143-5
Blaylock RL (2017) Parkinson’s disease: microglial/macrophage-induced immunoexcitotoxicity as a central mechanism of neurodegeneration. Surg Neurol Int 8:65. https://doi.org/10.4103/sni.sni_441_16
Bollinger JL, Bergeon Burns CM, Wellman CL (2016) Differential effects of stress on microglial cell activation in male and female medial prefrontal cortex. Brain Behav Immun 52:88–97. https://doi.org/10.1016/j.bbi.2015.10.003
Borst K, Schwabenland M, Prinz M (2018) Microglia metabolism in health and disease. Neurochem Int. https://doi.org/10.1016/j.neuint.2018.11.006
Cabezas R, Baez-Jurado E, Hidalgo-Lanussa O, Echeverria V, Ashraf GM, Sahebkar A, Barreto GE (2018) Correction to: growth factors and neuroglobin in astrocyte protection against neurodegeneration and oxidative stress. Mol Neurobiol. https://doi.org/10.1007/s12035-018-1257-8
Carniglia L, Ramirez D, Durand D, Saba J, Turati J, Caruso C, Scimonelli TN, Lasaga M (2017) Neuropeptides and microglial activation in inflammation, pain, and neurodegenerative diseases. Mediat Inflamm 2017:5048616. https://doi.org/10.1155/2017/5048616
Chakari-Khiavi F, Dolati S, Chakari-Khiavi A, Abbaszadeh H, Aghebati-Maleki L, Pourlak T, Mehdizadeh A, Yousefi M (2019) Prospects for the application of mesenchymal stem cells in Alzheimer’s disease treatment. Life Sci 231:116564. https://doi.org/10.1016/j.lfs.2019.116564
Crosas-Molist E, Fabregat I (2015) Role of NADPH oxidases in the redox biology of liver fibrosis. Redox Biol 6:106–111. https://doi.org/10.1016/j.redox.2015.07.005
Dheen ST, Kaur C, Ling EA (2007) Microglial activation and its implications in the brain diseases. Curr Med Chem 14(11):1189–1197
Drela K, Siedlecka P, Sarnowska A, Domanska-Janik K (2013) Human mesenchymal stem cells in the treatment of neurological diseases. Acta Neurobiol Exp 73(1):38–56
Franco R, Fernandez-Suarez D (2015) Alternatively activated microglia and macrophages in the central nervous system. Prog Neurobiol 131:65–86. https://doi.org/10.1016/j.pneurobio.2015.05.003
Graeber MB, Li W, Rodriguez ML (2011) Role of microglia in CNS inflammation. FEBS Lett 585(23):3798–3805. https://doi.org/10.1016/j.febslet.2011.08.033
Haslund-Vinding J, McBean G, Jaquet V, Vilhardt F (2017) NADPH oxidases in oxidant production by microglia: activating receptors, pharmacology and association with disease. Br J Pharmacol 174(12):1733–1749. https://doi.org/10.1111/bph.13425
Her GJ, Wu HC, Chen MH, Chen MY, Chang SC, Wang TW (2013) Control of three-dimensional substrate stiffness to manipulate mesenchymal stem cell fate toward neuronal or glial lineages. Acta Biomater 9(2):5170–5180. https://doi.org/10.1016/j.actbio.2012.10.012
Hou L, Wang K, Zhang C, Sun F, Che Y, Zhao X, Zhang D, Li H, Wang Q (2018) Complement receptor 3 mediates NADPH oxidase activation and dopaminergic neurodegeneration through a Src-Erk-dependent pathway. Redox Biol 14:250–260. https://doi.org/10.1016/j.redox.2017.09.017
Jose S, Tan SW, Ooi YY, Ramasamy R, Vidyadaran S (2014) Mesenchymal stem cells exert anti-proliferative effect on lipopolysaccharide-stimulated BV2 microglia by reducing tumour necrosis factor-alpha levels. J Neuroinflamm 11:149. https://doi.org/10.1186/s12974-014-0149-8
Karussis D, Kassis I, Kurkalli BG, Slavin S (2008) Immunomodulation and neuroprotection with mesenchymal bone marrow stem cells (MSCs): a proposed treatment for multiple sclerosis and other neuroimmunological/neurodegenerative diseases. J Neurol Sci 265(1–2):131–135. https://doi.org/10.1016/j.jns.2007.05.005
Kettenmann H, Hanisch UK, Noda M, Verkhratsky A (2011) Physiology of microglia. Physiol Rev 91(2):461–553. https://doi.org/10.1152/physrev.00011.2010
Kumar A, Henry R, Stoica B, Loane D, Abulwerdi G, Bhat S, Faden A (2018) Neutral sphingomyelinase inhibition alleviates LPS induced microglia activation and neuroinflammation after experimental traumatic brain injury. J Pharmacol Exp Ther. https://doi.org/10.1124/jpet.118.253955
Lee DY, Oh YJ, Jin BK (2005) Thrombin-activated microglia contribute to death of dopaminergic neurons in rat mesencephalic cultures: dual roles of mitogen-activated protein kinase signaling pathways. Glia 51(2):98–110. https://doi.org/10.1002/glia.20190
Lewerenz J, Ates G, Methner A, Conrad M, Maher P (2018) Oxytosis/ferroptosis-(Re-) emerging roles for oxidative stress-dependent non-apoptotic cell death in diseases of the central nervous system. Front Neurosci 12:214. https://doi.org/10.3389/fnins.2018.00214
Lim SY, Subedi L, Shin D, Kim CS, Lee KR, Kim SY (2017) A new neolignan derivative, balanophonin isolated from firmiana simplex delays the progress of neuronal cell death by inhibiting microglial activation. Biomol Ther 25(5):519–527. https://doi.org/10.4062/biomolther.2016.224
Mukherjee P, Mulrooney TJ, Marsh J, Blair D, Chiles TC, Seyfried TN (2008) Differential effects of energy stress on AMPK phosphorylation and apoptosis in experimental brain tumor and normal brain. Mol Cancer 7:37. https://doi.org/10.1186/1476-4598-7-37
Oh KW, Moon C, Kim HY, Oh SI, Park J, Lee JH, Chang IY, Kim KS, Kim SH (2015) Phase I trial of repeated intrathecal autologous bone marrow-derived mesenchymal stromal cells in amyotrophic lateral sclerosis. Stem Cells Transl Med 4(6):590–597. https://doi.org/10.5966/sctm.2014-0212
Popiolek-Barczyk K, Mika J (2016) Targeting the microglial signaling pathways: new insights in the modulation of neuropathic pain. Curr Med Chem 23(26):2908–2928
Qiao H, Zhou Y, Qin X, Cheng J, He Y, Jiang Y (2018) NADPH oxidase signaling pathway mediates mesenchymal stem cell-induced inhibition of hepatic stellate cell activation. Stem Cells Int 2018:1239143. https://doi.org/10.1155/2018/1239143
Song WM, Colonna M (2018) The microglial response to neurodegenerative disease. Adv Immunol 139:1–50. https://doi.org/10.1016/bs.ai.2018.04.002
Steens J, Klein D (2018) Current strategies to generate human mesenchymal stem cells in vitro. Stem Cells Int 2018:6726185. https://doi.org/10.1155/2018/6726185
Subedi L, Ji E, Shin D, Jin J, Yeo JH, Kim SY (2017) Equol, a dietary daidzein gut metabolite attenuates microglial activation and potentiates neuroprotection in vitro. Nutrients. https://doi.org/10.3390/nu9030207
Togna AR, Latina V, Trefiletti G, Guiso M, Moschini S, Togna GI (2013) 1-Phenil-6,7-dihydroxy-isochroman inhibits inflammatory activation of microglia. Brain Res Bull 95:33–39. https://doi.org/10.1016/j.brainresbull.2013.03.001
Trallori E, Ghelardini C, Di Cesare Mannelli L (2019) Mesenchymal stem cells, implications for pain therapy. Neural Regen Res 14(11):1915–1916. https://doi.org/10.4103/1673-5374.259615
Wilhelmsson U, Andersson D, de Pablo Y, Pekny R, Stahlberg A, Mulder J, Mitsios N, Hortobagyi T, Pekny M, Pekna M (2017) Injury leads to the appearance of cells with characteristics of both microglia and astrocytes in mouse and human brain. Cereb Cortex 27(6):3360–3377. https://doi.org/10.1093/cercor/bhx069
Xue Y, Wang Y, Feng DC, Xiao BG, Xu LY (2008) Tetrandrine suppresses lipopolysaccharide-induced microglial activation by inhibiting NF-kappaB pathway. Acta Pharmacol Sin 29(2):245–251. https://doi.org/10.1111/j.1745-7254.2008.00734.x
Yan ZJ, Hu YQ, Zhang HT, Zhang P, Xiao ZY, Sun XL, Cai YQ, Hu CC, Xu RX (2013) Comparison of the neural differentiation potential of human mesenchymal stem cells from amniotic fluid and adult bone marrow. Cell Mol Neurobiol 33(4):465–475. https://doi.org/10.1007/s10571-013-9922-y
Zhai X, Qiao H, Guan W, Li Z, Cheng Y, Jia X, Zhou Y (2015) Curcumin regulates peroxisome proliferator-activated receptor-gamma coactivator-1alpha expression by AMPK pathway in hepatic stellate cells in vitro. Eur J Pharmacol 746:56–62. https://doi.org/10.1016/j.ejphar.2014.10.055
Zhan L, Krabbe G, Du F, Jones I, Reichert MC, Telpoukhovskaia M, Kodama L, Wang C, Cho SH, Sayed F, Li Y, Le D, Zhou Y, Shen Y, West B, Gan L (2019) Proximal recolonization by self-renewing microglia re-establishes microglial homeostasis in the adult mouse brain. PLoS Biol 17(2):e3000134. https://doi.org/10.1371/journal.pbio.3000134
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cao, D., Qiao, H., He, D. et al. Mesenchymal stem cells inhibited the inflammation and oxidative stress in LPS-activated microglial cells through AMPK pathway. J Neural Transm 126, 1589–1597 (2019). https://doi.org/10.1007/s00702-019-02102-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-019-02102-z