Abstract
Background
The management of craniopharyngiomas is challenging due to their high rate of recurrence following resection. Excision of recurrent tumors poses further surgical challenges due to loss of arachnoidal planes and adherence to anatomical structures. The endoscopic endonasal approach (EEA) offers a favorable alternative to transcranial approaches for primary craniopharyngiomas. However, the safety and efficacy of EEA for recurrent tumors, specifically after a prior transcranial approach, needs further investigation.
Methods
We performed a systematic review using PubMed to develop a database of cases of recurrent craniopharyngiomas previously treated with a transcranial approach.
Results
Fifteen articles were included in this review with a total of 75 cases. There were 50 males and 25 females with a mean age of 38 years (range 2–80). One prior transcranial surgery was done in 80.0% of cases, while 8.0% had two and 12.0% had more than two prior surgeries. Radiotherapy after transcranial resection was given in 18 cases (24.0%). Following EEA, vision improved in 60.0% of cases, and vision worsened in 8.6% of the cases. Of cases, 64.4% had pre-existing anterior hypopituitarism, and 43.8% had diabetes insipidus prior to EEA. New anterior hypopituitarism and diabetes insipidus developed in 24.6% and 21.9% of cases, respectively following EEA. Gross total resection (GTR) was achieved in 64.0%, subtotal resection in 32.0%, and partial resection in 4.0% revision EEA cases. GTR rate was higher in cases with no prior radiotherapy compared to cases with prior radiotherapy (72.0% vs 39.0%, p = 0.0372). The recurrence rate was 17.5% overall but was significantly lower at 10.0% following GTR (p = 0.0019). The average follow-up length was 41.2 months (range, 1–182 months).
Conclusion
The EEA can be utilized for resection of recurrent or residual craniopharyngiomas previously managed by a transcranial approach.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Craniopharyngiomas are rare, slow-growing, epithelial tumors derived from the remnants of Rathke’s pouch. They are located in the suprasellar or parasellar region and make up between 2 and 5% of all primary intracranial tumors with an incidence of 2 per 100,000 per year [34]. Patients with craniopharyngiomas often present with symptoms of increased intracranial pressure, endocrine dysfunction, and visual disturbances due to infiltration of, adherence to, or mass effect on surrounding critical structures of the sellar and parasellar regions, most notably the pituitary gland, hypothalamus, optic chiasm, blood vessels, and third ventricle [34]. Definitive treatment for craniopharyngiomas is resection of the tumor to achieve gross total resection (GTR); however, for tumors involving the optic chiasm, optic nerves, or the hypothalamus, acceptable treatment includes subtotal resection of the tumor followed by radiotherapy [27, 34, 41].
Recurrence of craniopharyngiomas remains an issue and complicates the management of these tumors. Craniopharyngiomas can recur from macroscopic remnants of the tumors left behind following resection, even after GTR. This can be explained by their proximity to adjacent neurovascular structures or from neuroradiologically undetectable tumors after GTR [6]. The recurrence rates after a transcranial approach are reported to be 9.0–51.0% with a median time to recurrence of 26–96 months as compared to an initial microscopic or endoscopic transsphenoidal approach, which has a recurrence rate of 0–13.0% with GTR and 24.0–60.0% with STR [31]. Treatment strategies to manage recurrent cases still remain controversial as surgical management of recurrent lesions is more technically challenging and is associated with greater morbidity and mortality [32, 36].
Salvage surgery with either a transcranial or an endoscopic endonasal approach (EEA) offers a cure for recurrent craniopharyngiomas, while radiotherapy, intracystic bleomycin, and cystic aspiration results in lower morbidity [1]. Successful excision of recurrent tumors depends on the primary surgical approach and the use of adjuvant radiotherapy because of the difficulty of tumor excision from scarring and adhesions. Multiple transcranial approaches have classically been utilized for resection of craniopharyngiomas depending on their location with respect to the optic chiasm, pituitary stalk, hypothalamus, and third ventricle. The size of the tumor as well as the type of approach that offers the best exposure of the tumor and vital structures is also taken into consideration [33]. The risks associated with a transcranial approach include the need for brain retraction [2]. In the past decade, EEA has been more commonly utilized as an alternative approach for suprasellar masses allowing for a clearer view of and access of midline tumors without the need for brain retraction and manipulation of the optic pathways [10]. Complications of EEA include postoperative cerebrospinal fluid (CSF) leak, although the rate of CSF leaks has considerably decreased over the past decade due to improved closure techniques [22]. Despite extensive research, there is no consensus in the literature regarding the timing of surgery, use of radiotherapy, or the appropriate surgical approach for the management of recurrent or residual craniopharyngiomas.
Thus, we performed a systematic review of the literature to determine the safety and efficacy of the EEA approach for recurrent or residual craniopharyngioma following a transcranial approach. We evaluated the endocrine and visual outcomes following secondary resection by EEA and compared the results to other series on primary resection using EEA.
Materials and methods
Search strategy and study eligibility
An electronic search of the literature was performed using the online PubMed/MEDLINE database in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA). The keywords used singly or in combination included “recurrent,” “recurrence,” “remnant,” “craniopharyngioma,” “endoscopic,” “endonasal,” and “transsphenoidal.” Eligibility of the articles was limited to English articles with human subjects with recurrent or residual craniopharyngiomas published between 2005 and 2018. The abstracts of qualifying studies were reviewed. Full-text articles were obtained for studies meeting the defined inclusion criteria. Finally, references of the relevant articles were examined for any potential studies missed from the original literature search that met our inclusion criteria.
Inclusion criteria
Studies included in this study were limited to all English-language, retrospective case series or case reports on EEA for recurrent or residual craniopharyngiomas with a previous primary transcranial approach. Only studies which provided individual patient outcome data were included.
Exclusion criteria
The exclusion criteria included non-English articles, review articles, EEA approach for non-specified recurrent or residual sellar lesions, craniopharyngioma case series without recurrence, recurrent craniopharyngioma cases without a primary transcranial approach, articles reporting only aggregate outcomes of the entire series, and those that did not report the visual or endocrine outcomes following the EEA approach.
Data extraction
All data were extracted by 2 independent authors, and any discrepancies were addressed following discussion among the senior authors. Variables collected for each study included sex, age, previous surgery type, prior radiotherapy, number of prior surgeries, tumor location, tumor size, tumor type, visual outcomes, endocrine outcomes, extent of resection, CSF leak, recurrence, complication, and follow up period. All studies used formal visual field and acuity testing postoperatively. Postoperative visual outcomes were classified as “improved,” “unchanged,” or “worse.” Postoperative assessment of extent of resection was based on postoperative computed tomography or magnetic resonance imaging in all studies. Since studies included in this article had different definitions of near total resection (NTR) and subtotal resection (STR), all cases with \(\ge\)50.0% resection of tumor was classified as STR and cases with \(>\)50.0% resection of tumor as partial resection (PR).
Data analysis
Microsoft Excel (Microsoft, Redmond, WA, USA) was used for data aggregation and analysis. Categorical variables were analyzed using chi-squared or the Fischer exact test for smaller samples. Significance was established as p < 0.05. Data included in this study did not have identifying patient information and therefore did not require approval from the Rutgers New Jersey Medical School Institutional Review Board.
Results
Our search using the keywords listed above identified a total of 369 articles (Fig. 1). Three duplicates were removed, and a total of 366 abstracts were screened. Only 55 articles were considered potentially eligible, and their full-text articles were reviewed for inclusion after exclusion of review articles and articles without cases with a primary transcranial approach. After applying the aforementioned inclusion criteria, 15 articles were included in this systematic review with a total of 75 cases [1, 3, 8, 9, 12, 13, 17,18,19,20, 23, 24, 29, 35, 39].
Patient demographics and tumor characteristics
The average age of the 75 cases in this review was 38 years old (range, 2–80 years). There were 50 males and 25 females (Table 1). In 60 cases, only one prior primary transcranial approach was done; six cases had two prior transcranial surgeries; six cases had three prior transcranial surgeries; two cases had four prior transcranial surgeries; and one case had six prior transcranial surgeries. A total of 18 cases (24.0%) had radiotherapy prior to EEA resection. The location of the tumor was reported in 57 cases. The most common location of the tumor was suprasellar (64.9%), followed by sellar and suprasellar (29.8%) and intrasellar (5.3%). Tumor size was reported in 35 cases, and the average tumor size was 2.84 cm (range 0.9–5.1 cm). Tumor type was reported in 49 cases with 31 cases having a mixed tumor with solid and cystic components; 13 cases with a cystic type; and 5 cases with a solid type. The average follow-up was 41.2 months (range, 1–182 months).
Visual outcomes
Visual outcomes were reported in 74 patients. Four patients had normal visual function before and after the procedure. Following resection, vision improved in 42 cases (60.0%), was unchanged in 22 cases (31.4%), and worsened in 6 cases (8.6%). There were no significant differences in the visual outcomes when analyzed based on sex, age, number of prior surgeries, previous radiotherapy, location of the tumor, tumor size, tumor type, and extent of resection (Table 2).
Endocrine outcomes
Changes in anterior pituitary function were reported in 73 cases (Table 1). Following resection, hypopituitarism or panhypopituitarism developed in 18 patients (24.6%). Of those who had normal preoperative pituitary function, 69.0% (18/26) developed new anterior hypopituitarism. The majority of cases (n = 47, 64.4%) did not experience any change in their endocrine outcomes and continued to experience their pre-existing hypopituitarism or panhypopituitarism. There were 8 cases (11.0%) who had normal endocrine function before and after the procedure. There was no statistically significant difference in new endocrine dysfunction when analyzed based on sex, age, number of prior surgeries, previous radiotherapy, location of the tumor, tumor size, tumor type, and extent of resection (Table 2). Diabetes insipidus (DI) outcomes following the EEA were reported in 73 cases (Table 1). DI was not present before or after the procedure in 25 cases, present preoperatively in 32 cases, and there was new DI after the procedure in 16 cases. The total incidence of DI in cases with no previous DI was 16 out of 41 (39.0%) (Table 2). The incidence of DI was significantly greater in younger patients (p = 0.0043) and those with a greater number of prior surgeries (p = 0.018). There was no significant difference in the incidence of DI with regards to gender, previous radiotherapy, location, tumor size, tumor type, or extent of resection.
Extent of resection
GTR was achieved in 48 cases (64.0%), STR in 24 cases (32.0%), and PR in 3 cases (4.0%) (Table 1). In patients \(\ge\)60 years old, GTR was achieved in 83.0% of cases (p = 0.0008) (Table 3). The rate of GTR was not significantly impacted by the total number of prior transcranial surgeries (p = 0.0222). GTR was achieved in 39.0% of cases that had previous radiotherapy compared to 72.0% that did not have any previous radiotherapy (p = 0.0372). The recurrence rate was only 10.0% with GTR compared to the 80.0% recurrence rate when STR was achieved (p = 0.0019). The rate of GTR was lower for tumors involving both the sellar and suprasellar region than tumors involving either sellar only or suprasellar region only, although this was not statistically different. The gender, number of prior surgeries, tumor size, presence of CSF leak, and tumor type were not significantly associated with the extent of resection.
Complications and recurrence
Postoperative CSF leak was noted in 8 (10.7%) cases (Table 1). Complications other than a CSF leak were reported in 66 cases and were present in 9 cases (13.6%). There was one case of meningitis, one case of fungal ventriculitis, and three cases of cognitive decline. One patient, a 2-year-old male with STR, developed postoperative cognitive decline, meningitis, hydrocephalus, and a seizure. Three patients died postoperatively. Two patients died from disease progression on follow-up, and one patient died from large left hemisphere infarct postoperatively. Recurrence occurred in 10 of the 57 cases (17.5%) in which recurrence was reported.
Discussion
Studies have shown that EEA offers a superior view of the tumor, greater extent of resection with less morbidity, and lower complication rates compared to transcranial approaches for primary craniopharyngiomas [21, 22, 25]. There is no consensus on the optimal timing or surgical approach for the management of recurrent or residual craniopharyngiomas. Although various case series on EEA for recurrent or residual craniopharyngioma have been published, few of these studies have analyzed the impact of the primary surgical approach on the outcomes of the secondary EEA approach. We conducted a review of the literature to determine the efficacy and safety of an EEA for recurrent or residual craniopharyngioma following a primary transcranial approach. In this review, we included 15 articles with a total of 75 recurrent or residual craniopharyngioma cases [1, 3, 8, 9, 12, 13, 17,18,19,20, 23, 24, 29, 35, 39].
Approach selection for craniopharyngioma
Careful consideration should be given to type of surgical approach that is used when resecting craniopharyngiomas. The decision between selecting an endoscopic endonasal route and/or trasnscranial route depends on many anatomical considerations including relationship of the tumor to the optic chiasm and pituitary gland, extension into the third ventricle, lateral extension to the carotid artery, and extension into the interhemispheric fissure. Liu et al. emphasized the importance of a tailored approach in determining the optimal surgical and treatment modalities for individual patients based on the extent of the tumor and its proximity and relationship to neighboring structures [30]. Transcranial approaches provide direct access to the parasellar compartments and are beneficial in situations where tumors extend laterally beyond the internal carotid artery bifurcation. A transcranial approach, however, may not provide access to the retrochiasmatic space especially with a prefixed chiasm. An endoscopic endonasal approach provides direct access to the anterior skull base and is appropriate for intrasellar lesions. The retrochiasmatic space including extension into the third ventricle can be accessed from an endonasal route. The endoscopic endonasal route may not provide access to tumor lateral to the carotid artery or purely intraventricular craniopharyngiomas. Intraoperative CSF leak repair options may also be limited with multiple resections via an endoscopic endonasal routes.
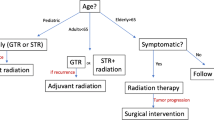
Recurrent craniopharyngioma
Due to the high recurrence rate of craniopharyngiomas and the associated morbidity, various modalities have been utilized and developed to achieve disease control including adjuvant radiation, brachytherapy, chemotherapy, and immunotherapy [28]. While gross total resection is generally the goal of surgery to achieve long-term disease control, subtotal resection followed by radiation may provide similar progression-free survival and improved endocrine outcome [38]. Emerging therapies including BRAF-MEK inhibitors for papillary type craniopharyngiomas have been shown to provide to significant reduction in tumor volume after resection or biopsy [5].
When considering salvage surgery for recurrent craniopharyngioma, it is important to understand that the arachnoidal planes have been violated during the primary surgery. Not only does the loss of arachnoidal planes between the tumor and the normal tissue make dissection more difficult, it also places structures, such as the hypothalamus at risk for injury [40]. Additionally, primary surgery or previous adjuvant radiotherapy causes adhesions and adherence of the tumor to neurovascular structures, which makes complete resection of the tumor difficult and places vital vasculature at risk of injury, resulting in permanent neurological deficits or death. The EEA is an optimal approach for recurrent craniopharyngioma especially after a primary transcranial approach since it offers an untouched route. The EEA allows direct visualization of the hypothalamic stalk and surrounding neurovascular anatomy without requiring brain retraction. The EEA can be used to resect inferior and posterior portions of the tumor in locations such as the subchiasmatic, retrosellar, and intraventricular areas that cannot be reached with the transcranial approach [9]. The remnant tumors in these areas can be accessed by the EEA, which were previously inaccessible by the transcranial approach and thus will have preserved arachnoidal planes.
Visual outcomes
The EEA allows for direct visualization of the infrachiasmatic space without manipulation of the optic apparatus, thereby reducing the risk of injury to neurovascular structures. In a systematic review of the literature of resection of primary and recurrent craniopharyngiomas, Komotar et al. reports the visual improvement rate to be 33.1% with a transcranial approach and 56.2% with the EEA [25]. Cavallo et al. reported improvement in vision in 74.7% of their patients and worsening vision in 2.5% of their patients with an EEA for mostly primary craniopharyngiomas [11]. In studies of recurrent craniopharyngiomas that did not differentiate the primary approach, vision improvements rates are higher for the EEA for recurrent cases than the 33.0–64.0% visual improvement reported for transcranial approach [15, 16]. This is presumably due to the wider view of the under surface of the optic chiasm offered by the EEA. We found the rate of vision improvement to be 60.0% with EEA for recurrent cases following a craniotomy, with only 8.6% of cases experiencing worsening of the visual outcomes. Although our reported visual improvement is not high as those reported in individual series of recurrent cases, this study demonstrates that an EEA following a transcranial approach can achieve improvement in vision despite the increased risk of injury to the optic pathways secondary to scarring and displacement of the chiasm.
Endocrine outcomes
EEA for primary craniopharyngiomas offers better visibility and lighting, allowing for decreased manipulation and risk of damage to the hypothalamus and the pituitary stalk. Anterior pituitary dysfunction ranges from 57.1 to 100%, and DI ranges from 56.3 to 100% in the literature following EEA for primary craniopharyngiomas [7]. The average incidence of DI after EEA in primary cases (27.7%) is significantly lower compared to the transcranial approach (54.8%), although there was no significant difference between the rates of hypopituitarism between the two approaches [25]. In recurrent craniopharyngioma cases, without accounting for the impact of the primary approach, Turel et al. reported new onset panhypopituitarism in 73.3% of their patients managed by endoscopic, transcranial, or both approaches [40]. Similarly, Koutourousio et al. reported pituitary dysfunction in 60.0% and DI in 50.0% of recurrent cases managed by a transcranial approach that had a primary resection with either an EEA or transcranial approach. This is in comparison to pituitary dysfunction in 51.1% and DI in 46.3% of primary cases managed by EEA [26]. In our review of the literature, we found new pituitary dysfunction in 69.0% of the cases and new long-term DI in 39.0% of the cases. The risk of DI was also significantly impacted by the number of prior transcranial surgeries. The EEA for recurrent craniopharyngiomas can be associated with a high risk of postoperative endocrine dysfunction requiring careful resection of tumor with minimal manipulation of the hypothalamus and pituitary stalk. Although we did not analyze the correlation of endocrine dysfunction with resection of pituitary stalk, this may be unavoidable during resection of large adherent recurrent tumors.
Extent of resection
Several studies have advocated for radical resection as the primary surgical management of craniopharyngiomas, which offers a definitive cure, but can result in significant morbidity [41, 42]. In cases for which GTR is not possible, to avoid the endocrinological and visual deficits, partial resection of the tumor can be followed up by radiotherapy [37]. The average rate of GTR with EEA (66.9%) is significantly greater than the 48.3% GTR rate through a transcranial approach for all craniopharyngiomas [25]. GTR can be difficult to achieve in recurrent cases due to the adherence of the tumor to critical neurovascular structures. The EEA for recurrent craniopharyngiomas with either a primary EEA or transcranial resection resulted in GTR in 29.4–80.0% of cases [14, 26]. The GTR rate of 64.0% in this study is within the range reported within series of primary and recurrent craniopharyngiomas managed by EEA, which did not differentiate the outcomes based on the primary approach. Although tumor resection through this approach can be technically challenging and, as with a transcranial approach, is associated with a high risk of endocrine and visual dysfunction, we did not find a statistically significant effect of the extent of resection on visual (p = 0.2841), anterior pituitary (p = 0.4921), or DI outcomes (p = 0.1561).
In patients who received radiotherapy prior to EEA, GTR rate was 39.0% compared to 72.0% in patients who did not receive radiotherapy. The effect of radiotherapy on the extent of resection has been illustrated by previous studies [9, 14]. Dhandapani et al. found a 50.0% rate of GTR and NTR in patients with prior radiotherapy and 85.0% in patients with no prior radiotherapy [14]. The extent of resection achieved for primary tumors may depend on whether tumor resection was done by an experienced surgeon at a specialized medical center with a high volume of endoscopically managed craniopharyngioma cases. Therefore, it might be reasonable for patients with STR for a primary craniopharyngioma to be evaluated by an experienced endoscopically trained neurosurgeon to determine if greater extent of resection can be achieved with an EEA prior to considering radiotherapy to control tumor growth, which can potentially decrease the effectiveness of future surgical attempts of complete resection.
Complications/recurrence
CSF leak following EEA is a well-known complication in the literature [4, 26, 30]. In a review of 800 patients treated with an EEA, CSF leak rate was the most common complication (15.9%) [22]. However, this CSF leak rate decreased to 5.4% after a pedicled vascularized flap was utilized for reconstruction. Review of the literature of all EEAs done for anterior skull base pathologies has demonstrated an average CSF leak rate of 8.9%, ranging from 0 to 40.0% [4]. The 10.0% CSF leak rate in this study is within the range reported in the literature. Borg et al. also reported an average mortality rate of 0.4% and an average meningitis rate of 1.7% in the literature with an EEA. The meningitis rate was 2.4% in patients with CSF leaks compared to 1.3% in patients without a CSF leak [4]. We found that only two patients (3.0%) developed postoperative meningitis, of which one had a documented CSF leak.
Craniopharyngiomas are difficult to manage due to their high rate of recurrence even after GTR. Koutourousiou et al. reported an overall recurrence rate of 34.4% and a 25.0% recurrence rate after GTR compared to 40.0% in non-GTR cases [26]. Other studies have also highlighted the higher rate of recurrence with STR, demonstrating the importance of achieving GTR during the primary surgery or treatment with adjuvant radiotherapy following STR [14, 40]. The recurrence rate in this study was 17.5% in the 57 cases with reported long-term outcomes. Only one of the ten patients with recurrence initially had GTR, while eight patients had STR and one had PR.
Limitations
The major limitation of this systematic review is inherent to the quality and number of case series currently available in the literature on EEA for recurrent or residual craniopharyngioma cases. Although more case series on craniopharyngiomas have been published, many of them could not be included in this review due to the lack of individual patient data included in the articles or lack of recurrent cases with a primary transcranial approach. Additionally, for the majority of the cases included in this review, not all outcome variables were mentioned in the original articles. The heterogeneity in the reporting of outcomes limited the power of the analysis of the categorical variables. However, this review presents the largest group of recurrent or residual craniopharyngiomas managed by EEA after a transcranial approach.
Conclusion
Surgical management of recurrent craniopharyngioma poses many challenges including loss of the dissection planes and adherence of the tumor to surrounding anatomical structures. EEA after a transcranial approach can offer better visualization of the tumor via an untouched route and allow greater excision of previously inaccessible tumor. The visual and endocrinological outcomes are comparable to rates reported in the literature for EEA for primary tumors. Radiotherapy following STR may limit the extent of resection during repeat surgery due to increased adherence of the tumor.
References
Alalade AF, Ogando-Rivas E, Boatey J, Souweidane MM, Anand VK, Greenfield JP, Schwartz TH (2018) Suprasellar and recurrent pediatric craniopharyngiomas: expanding indications for the extended endoscopic transsphenoidal approach. J Neurosurg Pediatr 21:72–80
Alli S, Isik S, Rutka JT (2016) Microsurgical removal of craniopharyngioma: endoscopic and transcranial techniques for complication avoidance. J Neurooncol 130:299–307
Bal E, Oge K, Berker M (2016) Endoscopic endonasal transsphenoidal surgery, a reliable method for treating primary and recurrent/residual craniopharyngiomas: nine years of experience. World Neurosurg 94:375–385
Borg A, Kirkman MA, Choi D (2016) Endoscopic endonasal anterior skull base surgery: a systematic review of complications during the past 65 years. World Neurosurg 95:383–391
Brastianos PK, Twohy E, Geyer S, Gerstner ER, Kaufmann TJ, Tabrizi S, Kabat B, Thierauf J, Ruff MW, Bota DA, Reardon DA, Cohen AL, De La Fuente MI, Lesser GJ, Campian J, Agarwalla PK, Kumthekar P, Mann B, Vora S, Knopp M, Iafrate AJ, Curry WT Jr, Cahill DP, Shih HA, Brown PD, Santagata S, Barker FG 2nd, Galanis E (2023) BRAF-MEK inhibition in newly diagnosed papillary craniopharyngiomas. N Engl J Med 389(2):118–126
Caldarelli M, di Rocco C, Papacci F, Colosimo CJ (1998) Management of recurrent craniopharyngioma Acta Neurochir (Wien) 140:447–454
Campbell PG, McGettigan B, Luginbuhl A, Yadla S, Rosen M, Evans JJ (2010) Endocrinological and ophthalmological consequences of an initial endonasal endoscopic approach for resection of craniopharyngiomas. Neurosurg Focus 28:E8
Cavallo LM, Prevedello DM, Solari D, Gardner PA, Esposito F, Snyderman CH, Carrau RL, Kassam AB, Cappabianca P (2009) Extended endoscopic endonasal transsphenoidal approach for residual or recurrentcraniopharyngiomas. J Neurosurg 111:578–589
Cavallo LM, Frank G, Cappabianca P, Solari D, Mazzatenta D, Villa A, Zoli M, D’Enza AI, Esposito F, Pasquini E (2014) The endoscopic endonasal approach for the management of craniopharyngiomas: a series of 103 patients. J Neurosurg 121:100–113
Cavallo LM, Solari D, Esposito F, Cappabianca P (2013) The endoscopic endonasal approach for the management of craniopharyngiomas involving the third ventricle. Neurosurg Rev 36:27–37
Cavallo LM, Solari D, Esposito F, Villa A, Minniti G, Cappabianca P (2014) The role of the endoscopic endonasal route in the management of craniopharyngiomas. World Neurosurg 82:S32–40
de Divitiis E, Cavallo LM, Cappabianca P, Esposito F (2007) Extended endoscopic endonasal transsphenoidal approach for the removal of suprasellar tumors: part 2. Neurosurgery 60:46–49
Dehdashti AR, Ganna A, Witterick I, Gentili F (2009) Expanded endoscopic endonasal approach for anterior cranial base and suprasellar lesions: indications and limitations. Neurosurgery 64:677–679
Dhandapani S, Singh H, Negm HM, Cohen S, Souweidane MM, Greenfield JP, Anand VK, Schwartz TH (2017) Endonasal endoscopic reoperation for residual or recurrent craniopharyngiomas. J Neurosurg 126:418–430
Elliott RE, Hsieh K, Hochm T, Belitskaya-Levy I, Wisoff J, Wisoff JH (2010) Efficacy and safety of radical resection of primary and recurrent craniopharyngiomas in 86 children. J Neurosurg Pediatr 5:30–48
Fahlbusch R, Honegger J, Paulus W, Huk W, Buchfelder M (1999) Surgical treatment of craniopharyngiomas: experience with 168 patients. J Neurosurg 90:237–250
Frank G, Pasquini E, Doglietto F, Mazzatenta D, Sciarretta V, Farneti G, Calbucci F (2006) The endoscopic extended transsphenoidal approach for craniopharyngiomas. Neurosurgery 59:ONS75–83; discussion ONS75–83 .
Gardner PA, Kassam AB, Snyderman CH, Carrau RL, Mintz AH, Grahovac S, Stefko S (2008) Outcomes following endoscopic, expanded endonasal resection of suprasellar craniopharyngiomas: a case series. J Neurosurg 109:6–16
Jane JAJ, Prevedello DM, Alden TD, Laws ERJ (2010) The transsphenoidal resection of pediatric craniopharyngiomas: a case series. J Neurosurg Pediatr 5:49–60
Jane JAJ, Kiehna E, Payne SC, Early SV, Laws ERJ (2010) Early outcomes of endoscopic transsphenoidal surgery for adult craniopharyngiomas. Neurosurg Focus 28:E9
Kassam AB, Gardner PA, Snyderman CH, Carrau RL, Mintz AH, Prevedello DM (2008) Expanded endonasal approach, a fully endoscopic transnasal approach for the resection of midline suprasellar craniopharyngiomas: a new classification based on the infundibulum. J Neurosurg 108:715–728
Kassam AB, Prevedello DM, Carrau RL, Snyderman CH, Thomas A, Gardner P, Zanation A, Duz B, Stefko ST, Byers K, Horowitz MB (2011) Endoscopic endonasal skull base surgery: analysis of complications in the authors’ initial 800 patients. J Neurosurg 114:1544–1568
Kim SK, Kim YH, Park C-K, Kim DG, Jung H-W (2014) Extended endoscopic endonasal approach for recurrent or residual adult craniopharyngiomas. Acta Neurochir (Wien) 156:1917–1922
Kitano M, Taneda M (2009) Extended transsphenoidal surgery for suprasellar craniopharyngiomas: infrachiasmatic radical resection combined with or without a suprachiasmatic trans-lamina terminalis approach. Surg Neurol 71:290–298
Komotar RJ, Starke RM, Raper DMS, Anand VK, Schwartz TH (2012) Endoscopic endonasal compared with microscopic transsphenoidal and open transcranial resection of craniopharyngiomas. World Neurosurg 77:329–341
Koutourousiou M, Gardner PA, Fernandez-Miranda JC, Tyler-Kabara EC, Wang EW, Snyderman CH (2013) Endoscopic endonasal surgery for craniopharyngiomas: surgical outcome in 64 patients. J Neurosurg 119:1194–1207
Lania A, Spada A, Lasio G (2016) Diagnosis and Management of Craniopharyngiomas: Key current topics. Springer International Publishing
Lara-Velazquez M, Mehkri Y, Panther E, Hernandez J, Rao D, Fiester P, Makary R, Rutenberg M, Tavanaiepour D, Rahmathulla G (2022) Current advances in the management of adult craniopharyngiomas. Current Oncology (Toronto Ont) 29(3):1645–1671
Leng LZ, Greenfield JP, Souweidane MM, Anand VK, Schwartz TH (2012) Endoscopic, endonasal resection of craniopharyngiomas: analysis of outcome including extent of resection, cerebrospinal fluid leak, return to preoperative productivity, and body mass index. Neurosurgery 70:110–114
Liu JK, Sevak IA, Carmel PW, Eloy JA (2016) Microscopic versus endoscopic approaches for craniopharyngiomas: choosing the optimal surgical corridor for maximizing extent of resection and complication avoidance using a personalized, tailored approach. Neurosurg Focus 41:E5
Liubinas SV, Munshey AS, Kaye AH (2011) Management of recurrent craniopharyngioma. J Clin Neurosci Off J Neurosurg Soc Australas 18:451–457
Minamida Y, Mikami T, Hashi K, Houkin K (2005) Surgical management of the recurrence and regrowth of craniopharyngiomas. J Neurosurg 103:224–232
Mortini P, Gagliardi F, Bailo M, Losa M (2016) Surgical approach to craniopharyngiomas: transcranial routes. In: Lania A, Spada A, Lasio G (eds) Diagnosis and Management of Craniopharyngiomas. Springer, Cham
Müller HL (2014) Craniopharyngioma. Endocr Rev 35:513–543
Park C-S, Kim B-G, Shin J-H, Cho J-H (2014) Endoscopic transnasal transsphenoidal approach for craniopharyngioma: report of 6 cases. Ear Nose Throat J 93:E16-20
Rubin BA, Kim I, Wisoff JH (2015) Management of the recurrence of craniopharyngiomas. In: Kenning TJ, Evans JJBT-C (eds) Academic press, Boston, pp 419–425
Savateev AN, Trunin YY, Mazerkina NA (2017) Radiotherapy and radiosurgery in treatment of craniopharyngiomas. Zh Vopr Neirokhir Im N N Burdenko 81:94–106
Schoenfeld A, Pekmezci M, Barnes MJ, Tihan T, Gupta N, Lamborn KR, Banerjee A, Mueller S, Chang S, Berger MS, Haas-Kogan D (2012) The superiority of conservative resection and adjuvant radiation for craniopharyngiomas. J Neuro-Oncol 108(1):133–139
Tang B, Xiao L, Xie S, Huang G, Wang Z, Zhou D, Zeng E, Hong T (2018) Extended endoscopic endonasal approach for recurrent or residual symptomatic craniopharyngiomas. Clin Neurol Neurosurg 168:38–45
Turel MK, Tsermoulas G, Gonen L, Klironomos G, Almeida JP, Zadeh G, Gentili F (2016) Management and outcome of recurrent adult craniopharyngiomas: an analysis of 42 cases with long-term follow-up. Neurosurg Focus 41:E11
Van Effenterre R, Boch A-L (2002) Craniopharyngioma in adults and children: a study of 122 surgical cases. J Neurosurg 97:3–11
Zuccaro G (2005) Radical resection of craniopharyngioma. Childs Nerv Syst 21:679–690
Author information
Authors and Affiliations
Contributions
Author contributions to the study and manuscript preparation include the following. Conception and design: James K. Liu. Acquisition of data: all authors. Analysis and interpretation of data: all authors. Drafting the article: Gurkirat Kohli, Phabinly James Gabriel, Melanie Brady, and Christina Fang. Critically revising the article: James K. Liu and Jean Anderson Eloy. Reviewed submitted version of manuscript: James K. Liu. Study supervision: James K. Liu.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study formal consent is not required.
Consent to participate
N/A.
Consent for publication
N/A.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kohli, G., Gabriel, P.J., Brady, M. et al. The role of endoscopic endonasal salvage surgery in recurrent or residual craniopharyngioma after a transcranial approach: a systematic review. Acta Neurochir 166, 120 (2024). https://doi.org/10.1007/s00701-024-05980-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00701-024-05980-9