Abstract
Background
Compared to vertebral body fusion, artificial discs are thought to lessen the risks of adjacent segment disease and the need for additional surgery by maintaining spinal mobility as they mimic the intervertebral disc structure. No studies have compared the rates of postoperative complications and the requirement for secondary surgery at adjacent segments among patients who have undergone anterior lumbar interbody fusions (ALIF) versus those undergoing lumbar arthroplasty.
Methods
An all-payer claims database identified 11,367 individuals who underwent single-level ALIF and lumbar arthroplasty for degenerative disc disease (DDD) between January 2010 and October 2020. Rates of complications following surgery, the need for additional lumbar surgeries, length of stay (LOS), and postoperative opioid utilization were assessed in matched cohorts based on logistic regression models. Kaplan-Meyer plots were created to model the probability of additional surgery.
Results
Following 1:1 exact matching, 846 records of patients who had undergone ALIF or lumbar arthroplasty were analyzed. All-cause readmission within 30–30 days following surgery was significantly higher in patients undergoing ALIF versus arthroplasty (2.6% vs. 0.71%, p = 0.02). LOS was significantly lower among the patients who had undergone ALIF (1.043 ± 0.21 vs. 2.17 ± 1.7, p < .001).
Conclusions
ALIF and lumbar arthroplasty procedures are equally safe and effective in treating DDD. Our findings do not support that single-level fusions may biomechanically necessitate revisional surgeries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lower back pain is among the most prevalent causes of long-term disability worldwide [29]. Degenerative disc disease (DDD), the progressive deterioration of the intervertebral disc, is a common etiology of lower back pain [21]. Although there is a wide selection of available pharmacological treatments and physical therapy, patients with lumbar DDD refractory to conservative measures must often resort to discectomy, fusion, or lumbar disc arthroplasty for a definitive solution. Currently, lumbar fusion procedures are the most commonly utilized technique, well known for their stability and time-tested effectiveness on pain relief [12]. However, lumbar fusions are not benign procedures— the high frequency of complications such as adjacent segment disease (ASD) and pseudoarthrosis has continued to stimulate research into more optimal techniques for surgical management [10].
Total disc replacement (TDR), also known as arthroplasty or artificial disc replacement, is a newer surgical approach that may offer benefits over traditional arthrodesis, including preserved range of motion, restoration of disc height, and reduced disc subsidence [2, 4, 19]. Additionally, several studies have reported lower pain and disability scores and higher patient satisfaction rates with TDR versus lumbar fusion. However, some of these studies reflect outcomes for posterolateral fusion instead of anterior fusion [18, 28, 34]. Recently, Auerbach et al. directly compared the lumbar motion profiles in patients undergoing fusion versus TDR and concluded that fusions have steeper lumbar motion gradients at the adjacent segment during flexion and extension compared with TDR and control [1]. However, as previous studies have not adequately evaluated the incidence of surgical complications and the need for additional surgery, controversy remains regarding whether TDR is superior to ALIF [11, 13, 14, 23, 32]. To this end, we assess postoperative outcomes, including reoperation rates following single-level arthroplasty compared to single-level ALIFs in patients with DDD.
Methods
Data source
This retrospective cohort study utilized longitudinal data from the MARINER database (PearlDiver Technologies, Colorado Springs, USA), an all-payer claims database that includes records for over 120 million patients across all 50 US states. This database includes all healthcare encounters and prescription claims billed to all payers from 2010 to 2020. Independent third parties audit all claims. Diagnoses, procedures, and patient demographics can be identified in the database with International Classification of Diseases (ICD) 9 and 10 codes and Current Procedural Terminology (CPT) codes. Our institution’s Institutional Review Board provided exemption status for this study due to the minimal risk to participating individuals. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.
Study population
Patients undergoing single-level ALIF or arthroplasty procedures between January 2010 and October 2020 were identified using ICD-9, ICD-10, and CPT codes. To be included in the study, patients had to be 18–84 years old, have complete records with demographic information, and have a continuous active insurance record in the database for at least 5 years following their index procedure. Additionally, patients with a history of previous spine surgery or those diagnoses of spine fractures, spondylolysis, spondylolisthesis, lumbar stenosis, and osteoporosis were excluded.
The ALIF and arthroplasty cohorts were matched based on patient age, sex, and comorbidities. Patient comorbidities within 1 year before their index procedure date were identified using ICD-9 and ICD-10 codes. These comorbidities included the Charlson Comorbidity Index, type 2 diabetes mellitus, hypertension, hyperlipidemia, obesity, history of smoking, and prescribed opioid use within 30 days before surgery. The patient selection procedure is detailed in Fig. 1. Patient demographics and comorbidities are tabulated in Table 1.
Outcome definitions
The primary outcome of this retrospective cohort study was the need for additional lumbar surgery within 5 years of the index procedure. This was identified using ICD-9, ICD-10, and CPT codes. Other outcomes that were measured similarly included length of stay, the number of patients taking opioids at 30 days following surgery, morphine milligram equivalents per day among patients taking opioids at 30 days following surgery, all-cause readmissions within 30 days of surgery, urinary tract infections, pneumonia, hematoma, wound dehiscence, and deep vein thrombosis within 30 days following surgery.
Statistical analysis
Descriptive characteristics calculated were all patients. Binomial and logistic regression models were utilized to match the two cohorts (ALIF vs. arthroplasty) based on age, sex, and comorbidities (Supplemental Tables 2 and 3). Categorical variables such as sex, age ranges, and comorbidities were compared using χ2 tests. Quantitative variables such as mean length of stay and morphine milligram equivalents were compared using Student’s t tests. Additionally, odds ratios with 95% confidence intervals were calculated for 30-day postoperative complication rates and 5-year additional lumbar surgery rates. Statistical analysis was performed using R version 4.1 (R Foundation, Vienna, Austria).
Results
Descriptive characteristics
Our database query yielded 51,410 patients who underwent single-level arthroplasty or ALIF procedures between 2010 and 2020. Of these, 3287 were excluded who were missing demographic information, did not have active insurance for 5 years following their index procedure, or did not meet our age criteria. An additional 36,756 patients were excluded due to diagnoses of spondylolisthesis, spondylolysis, lumbar stenosis, lumbar spine fractures, osteoporosis, or previous spine surgery (Fig. 1). Descriptive characteristics for the remaining 11,367 eligible patients are tabulated in Supplemental Table 1.
Eight hundred forty-six patients were matched 1:1 and distributed equally between the arthroplasty and ALIF cohorts. Age range distributions were identical between groups (p > 0.99). The most prevalent comorbidities in the study population were hypertension (21.28%), history of smoking (17.73%), and hyperlipidemia (10.64%). Between ALIF and arthroplasty patients, there was no statistically significant difference in rates of diabetes mellitus type II, hypertension, hyperlipidemia, chronic kidney disease, obesity, smoking, and prior opioid use. Demographic and comorbidity data for the matched patient population are detailed in Table 1.
Outcomes
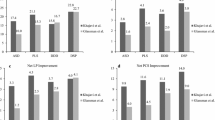
The rate of all-cause readmissions at 30 days was significantly higher in the ALIF cohort compared to the arthroplasty cohort (2.60% vs. 0.71%, p = 0.02). On the other hand, the mean length of stay was significantly shorter in the ALIF cohort compared to the arthroplasty cohort (1.043 days vs. 2.174 days, p < 0.001). There were no significant differences in the other outcomes measured, including the number of patients still taking opioids, morphine milligram equivalents per day, urinary tract infections, pneumonia, hematoma, wound dehiscence, deep vein thrombosis, and composite complications. Outcomes following single-level arthroplasty or ALIF are summarized in Table 2.
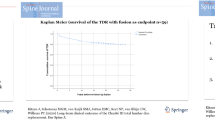
The odds of 30-day postoperative complications were no different for patients in the arthroplasty cohort compared to the ALIF cohort (OR 0.72, 95% CI 0.29 to 1.81). Likewise, the odds of additional lumbar surgery within 5 years of the index operation were not significantly different among patients who underwent arthroplasty versus ALIF (OR 0.83, 95% CI 0.51 to 1.35) (Table 3). The 5-year free probability of additional lumbar surgery among patients who underwent ALIF versus arthroplasty is plotted in Fig. 2.
Discussion
Arthroplasty devices are a well-established surgical option for patients with DDD [26, 34]. Nevertheless, arthroplasty has yet to be widely adopted in the USA as an alternative to ALIF, even though arthroplasty has been shown to better preserve the biomechanics of the spine compared to ALIF [2, 4, 19, 25]. Proponents of arthroplasty suggest that by mimicking the intervertebral disc structure, artificial discs attenuate the progression of ASD and reduce rates of further surgical intervention. However, opponents contend that the degeneration that eventually occurs is simply inherent to the natural progression of the underlying disease and that the literature has not borne out the claim of arthroplasty superiority over ALIF [13, 22, 24].
This is the largest retrospective cohort study to compare the rates of additional lumbar surgery at adjacent segments following ALIF versus arthroplasty. Our study utilized 91 million patient records from the MARINER database and ultimately analyzed 846 patients in 1:1 exact matched cohorts with no significant difference in patient characteristics. Our investigation did not identify an increased risk of further surgery in patients who underwent fusion compared to arthroplasty, as additional surgery rates nor 30-day postoperative complications were statistically different between cohorts.
These results align with several other studies published in the literature, although these are primarily industry-supported trials whose results should be taken with a grain of salt [15, 16, 22]. For example, Kitzen et al. followed up with 141 patients who had undergone TDR for DDD, with a mean follow-up of 16.7 years. They found long-term motion preservation in only 38.0% of patients; nonetheless, there was no association between residual mobility and the occurrence of ASD [15]. Indeed, the literature suggests that arthroplasty may not provide long-term preservation of motion in most patients and may not be associated with a reduction in ASD or reoperation regardless of motion preservation. Instead, the natural progression of DDD may predispose patients to further procedures on adjacent segments in the lumbar spine [6].
Although arthroplasty may not provide significant benefit over ALIF regarding reoperation on adjacent segments, it may still be a reasonable alternative. Several studies on arthroplasty versus lumbar fusion have established the noninferiority of arthroplasty in terms of both short-term and long-term outcomes for the treatment of DDD [7, 9, 30]. Our matched cohort analysis corroborated these findings compared to ALIF; both approaches demonstrated similar risk of complications at 30 days post-op or additional surgery at 5 years.
On the other hand, we found a shorter stay with ALIF at 1.043 days versus 2.174 days in contrast to published literature [16, 27]. Previous literature on this topic has been mixed. Shultz et al. in 2018 found a slightly increased length of stay by 0.28 days for ALIF patients. However, they also discussed the unclear clinical significance of this minor difference, as there was no translation to perioperative outcomes [27]. The length of stay difference uncovered in this study is much greater and warrants consideration by surgeons considering either ALIF or arthroplasty, especially given the costs associated with prolonged hospital stays.
Further research on this topic will be needed to better understand the cause of this finding which is especially surprising when considering the similarities between the ALIF and arthroplasty procedures. We also identified high readmission rates with ALIF compared to arthroplasty, similar to prior studies, which found higher or no different rates of readmissions with ALIF compared to arthroplasty [7, 27]. One possible explanation for the lower readmissions in arthroplasty patients is that the operation is performed in a limited selection of institutions given its novelty and thus only by a few surgeons now experienced with the technique. This could minimize the length of the operation, extraneous tissue manipulation, and invasiveness of the operation, leading to a decrease in postoperative problems causing readmission. It is also worth considering that the cohort of patients undergoing arthroplasty has been cherry-picked to some extent again, given the novelty of the technology and the industry’s desire to demonstrate positive results. No difference in 30-day postoperative opioid use was found between procedures, indicating that arthroplasty may comparably improve pain. A previous retrospective analysis by Mattei et al. suggested that arthroplasty patients may experience less back pain [18].
There are several limitations to this investigation that should be considered. Classification of patient demographics, comorbidities, and outcomes relies on accurate and reliable ICD-9, ICD-10, and CPT coding. Coding errors, including underreporting and miscoding, may have affected the results of our analysis. Additionally, while this investigation focused on reoperation rates at adjacent segments, the database used in this study lacks sufficient detail to assess the extent of adjacent segment degeneration in patients who underwent additional surgery within the 5-year follow-up period. Likewise, the assessment of motion preservation among patients who underwent ALIF or arthroplasty fell outside the scope of this study due to insufficient available data. In addition, arthroplasty is performed at fewer centers than ALIF, and thus the analyzed arthroplasty patients may be from a few overrepresented centers in the USA. However, the impact of this possibility is somewhat mitigated given the large sample size of 846.
Conclusion
ALIF and lumbar arthroplasty procedures are equally safe and effective in treating DDD. Our findings suggest that lumbar arthroplasty should take a larger role in DDD management in the USA as it did not increase reoperation rates. Interestingly, we found that ALIF was associated with a lower LOS. However, further prospective, retrospective, and biomechanical studies will need to be undertaken to better characterize this finding and considerations for ASD in the surgical management of DDD.
Data Availability
Data used in this study is publically available from PearlDiver Inc.
Abbreviations
- DDD:
-
Degenerative disc disease
- LOS:
-
Length of stay
- CI:
-
Confidence interval
- OR:
-
Odds ratio
- ASD:
-
Adjacent segment disease
- TDR:
-
Total disc replacement
- ALIF:
-
Anterior lumbar interbody fusions
- ICD:
-
International Classification of Diseases
- CPT:
-
Current procedural terminology
- STROBE:
-
Strengthening the Reporting of Observational Studies in Epidemiology
References
Auerbach JD, Wills BPD, McIntosh TC, Balderston RA (2007) Evaluation of spinal kinematics following lumbar total disc replacement and circumferential fusion using in vivo fluoroscopy. Spine 32(5):527–536. https://doi.org/10.1097/01.brs.0000256915.90236.17
Barrett RS, Lichtwark GA, Armstrong C, Barber L, Scott-Young M, Hall RM (2015) Fluoroscopic assessment of lumbar total disc replacement kinematics during walking. Spine 40(7):436–442. https://doi.org/10.1097/BRS.0000000000000787
Cheh G et al (2007) Adjacent segment disease followinglumbar/thoracolumbar fusion with pedicle screw instrumentation: a minimum 5-year follow-up. Spine 32(20):2253–2257. https://doi.org/10.1097/BRS.0b013e31814b2d8e
Chung SS, Lee CS, Kang CS, Kim SH (2006) The effect of lumbar total disc replacement on the spinopelvic alignment and range of motion of the lumbar spine. J Spinal Disord Tech 19(5):307–311. https://doi.org/10.1097/01.bsd.0000208255.14329.1e
Eck JC et al (2002) Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine 27(22):2431–2434. https://doi.org/10.1097/00007632-200211150-00003
Elfering A, Semmer N, Birkhofer D, Zanetti M, Hodler J, Boos N (2002) Risk factors for lumbar disc degeneration: a 5-year prospective MRI study in asymptomatic individuals. Spine 27(2):125–134. https://doi.org/10.1097/00007632-200201150-00002
Eliasberg CD, Kelly MP, Ajiboye RM, SooHoo NF (2016) Complications and rates of subsequent lumbar surgery following lumbar total disc arthroplasty and lumbar fusion. SPINE 41(2):173–181. https://doi.org/10.1097/BRS.0000000000001180
Fuller DA, Kirkpatrick JS, Emery SE, Wilber RG, Davy DT (1998) A kinematic study of the cervical spine before and after segmental arthrodesis. Spine 23(15):1649–1656. https://doi.org/10.1097/00007632-199808010-00006
Geisler FH et al (2004) Neurological complications of lumbar artificial disc replacement and comparison of clinical results with those related to lumbar arthrodesis in the literature: results of a multicenter, prospective, randomized investigational device exemption study of Charité intervertebral disc: invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves, March 2004. J Neurosurg Spine 1(2):143–154. https://doi.org/10.3171/spi.2004.1.2.0143
Ghiselli G, Wang JC, Bhatia NN, Hsu WK, Dawson EG (2004) Adjacent segment degeneration in the lumbar spine. J Bone Joint Surg Am 86(7):1497–1503. https://doi.org/10.2106/00004623-200407000-00020
Gornet MF, Burkus JK, Dryer RF, Peloza JH (2011) Lumbar disc arthroplasty with maverick disc versus stand-alone interbody fusion: a prospective, randomized, controlled, multicenter investigational device exemption trial. Spine 36(25):E1600–E1611. https://doi.org/10.1097/BRS.0b013e318217668f
Greenough CG, Taylor LJ, Fraser RD (1994) Anterior lumbar fusion: results, assessment techniques, and prognostic factors. Eur Spine J 3(4):225–230. https://doi.org/10.1007/BF02221598
Guyer RD et al (2009) Prospective, randomized, multicenter Food and Drug Administration investigational device exemption study of lumbar total disc replacement with the CHARITÉ artificial disc versus lumbar fusion: five-year follow-up. Spine J 9(5):374–386. https://doi.org/10.1016/j.spinee.2008.08.007
Harrop JS et al (2008) Lumbar adjacent segment degeneration and disease after arthrodesis and total disc arthroplasty. Spine 33(15):1701–1707. https://doi.org/10.1097/BRS.0b013e31817bb956
Kitzen J et al (2021) Long-term residual-mobility and adjacent segment disease after total lumbar disc replacement. Glob Spine J 11(7):1032–1039. https://doi.org/10.1177/2192568220935813
Kurtz SM et al (2010) National revision burden for lumbar total disc replacement in the united states: epidemiologic and economic perspectives. Spine 35(6):690–696. https://doi.org/10.1097/BRS.0b013e3181d0fabb
Lee CK (1988) Accelerated degeneration of the segment adjacent to a lumbar fusion. Spine 13(3):375–377. https://doi.org/10.1097/00007632-198803000-00029
Mattei TA, Beer J, Teles AR, Rehman AA, Aldag J, Dinh D (2017) Clinical outcomes of total disc replacement versus anterior lumbar interbody fusion for surgical treatment of lumbar degenerative disc disease. Glob Spine J 7(5):452–459. https://doi.org/10.1177/2192568217712714
McAfee PC et al (2005) A prospective, randomized, multicenter food and drug administration investigational device exemption study of lumbar total disc replacement with the CHARITÉ TM artificial disc versus lumbar fusion: part II: evaluation of radiographic outcomes and correlation of surgical technique accuracy with clinical outcomes. Spine 30(14):1576–1583. https://doi.org/10.1097/01.brs.0000170561.25636.1c
Miyakoshi N, Abe E, Shimada Y, Okuyama K, Suzuki T, Sato K (2000) Outcome of one-level posterior lumbar interbody fusion for spondylolisthesis and postoperative intervertebral disc degeneration adjacent to the fusion. Spine 25(14):1837–1842. https://doi.org/10.1097/00007632-200007150-00016
Phillips FM, Slosar PJ, Youssef JA, Andersson G, Papatheofanis F (2013) Lumbar spine fusion for chronic low back pain due to degenerative disc disease: a systematic review. Spine 38(7):E409. https://doi.org/10.1097/BRS.0b013e3182877f11
Radcliff KE et al (2013) Adjacent segment disease in the lumbar spine following different treatment interventions. Spine J 13(10):1339–1349. https://doi.org/10.1016/j.spinee.2013.03.020
Ren C, Song Y, Liu L, Xue Y (2014) Adjacent segment degeneration and disease after lumbar fusion compared with motion-preserving procedures: a meta-analysis. Eur J Orthop Surg Traumatol 24(S1):245–253. https://doi.org/10.1007/s00590-014-1445-9
Saavedra-Pozo FM, Deusdara RAM, Benzel EC (2014) Adjacent segment disease perspective and review of the literature. Ochsner J 14(1):78–83
Saifi C et al (2018) National trends for primary and revision lumbar disc arthroplasty throughout the United States. Glob Spine J 8(2):172–177. https://doi.org/10.1177/2192568217726980
Sandhu FA, Dowlati E, Garica R (2020) Lumbar arthroplasty: past, present, and future. Neurosurgery 86(2):155–169. https://doi.org/10.1093/neuros/nyz439
Shultz BN et al (2018) Total disc arthroplasty versus anterior interbody fusion in the lumbar spine have relatively a few differences in readmission and short-term adverse events. Spine 43(1):E52–E59. https://doi.org/10.1097/BRS.0000000000002337
Sköld C, Tropp H, Berg S (2013) Five-year follow-up of total disc replacement compared to fusion: a randomized controlled trial. Eur Spine J 22(10):2288–2295. https://doi.org/10.1007/s00586-013-2926-y
Vos T et al (2016) Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. The Lancet 388(10053):1545–1602. https://doi.org/10.1016/S0140-6736(16)31678-6
Wei J, Song Y, Sun L, Lv C (2013) Comparison of artificial total disc replacement versus fusion for lumbar degenerative disc disease: a meta-analysis of randomized controlled trials. Int Orthop 37(7):1315–1325. https://doi.org/10.1007/s00264-013-1883-8
Wu W, Thuomas K-Å, Hedlund R, Leszniewski W, Vavruch L (1996) Degenerative changes following anterior cervical discectomy and fusion evaluated by fast spin-echo MR imaging. Acta Radiol 37(3P2):614–617. https://doi.org/10.1177/02841851960373P239
Yue JJ et al (2019) Five-year results of a randomized controlled trial for lumbar artificial discs in single-level degenerative disc disease. Spine 44(24):1685–1696. https://doi.org/10.1097/BRS.0000000000003171
Zencica P, Chaloupka R, Hladíková J, Krbec M (2010) Adjacent segment degeneration after lumbosacral fusion in spondylolisthesis: a retrospective radiological and clinical analysis. Acta Chir Orthop Traumatol Cech 77(2):124–130
Zigler J, Ferko N, Cameron C, Patel L (2018) Comparison of therapies in lumbar degenerative disc disease: a network meta-analysis of randomized controlled trials. J Comp Eff Res 7(3):233–246. https://doi.org/10.2217/cer-2017-0047
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the (place name of institution and national research committee) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Khalid, S.I., Deysher, D., Thompson, K. et al. Outcomes of patients undergoing single-level arthroplasty versus anterior lumbar interbody fusion. Acta Neurochir 165, 1915–1921 (2023). https://doi.org/10.1007/s00701-023-05616-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-023-05616-4