Abstract
Background
One of the main drawbacks in the surgery of large craniopharyngiomas is the presence of a prefixed optic chiasm. Our main objective in this study is to compare the predictive value of the optic nerve length and optic chiasm location on large craniopharyngiomas’ extent of resection.
Method
We retrospectively studied 21 consecutive patients with large craniopharyngiomas who underwent tumor resection through the trans-eyebrow supraorbital approach. Clinical and radiological findings on preoperative MRI were recorded, including the optic chiasm location classified as prefixed, postfixed or normal. We registered the optic nerve length measured intraoperatively prior to tumor removal and confirmed the measurements on preoperative MRI. Using a linear regression model, we calculated a prediction formula of the percentage of the extent of resection as a function of optic nerve length.
Results
On preoperative MRI, 15 patients were considered to have an optic chiasm in a normal location, 3 cases had a prefixed chiasm, and the remaining 3 had a postfixed chiasm. In the group with normal optic chiasm location, a wide range of percentage of extent of resection was observed (75–100%). The percentage of extent of resection of large craniopharyngiomas was observed to be dependent on the optic nerve length in a linear regression model (p < 0.0001). According to this model in the normal optic chiasm location group, we obtained an 87% resection in 9-mm optic nerve length patients, a 90.5% resection in 10-mm optic nerve length patients and 100% resection in 11-mm optic nerve length patients.
Conclusions
Optic chiasm location provides useful information to predict the percentage of resection in both prefixed and postfixed chiasm patients but not in the normal optic chiasm location group. Optic nerve length was proven to provide a more accurate way to predict the percentage of resection than the optic chiasm location in the normal optic chiasm location group.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Surgical treatment of craniopharyngiomas is challenging owing to their deep location, size and propensity to adherence to surrounding critical structures, such as the optic chiasm, hypothalamus and carotid arteries. Craniopharyngioma surgery can lead to a significant operative morbidity and mortality whose incidence can increase substantially in association with specific anatomic features, especially with the optic chiasm location.
The optic chiasm lies over the body of the sphenoid bone, typically above the diaphragma sellae, but its relative position over the sella is variable. This variability was first described in the 1920s by Schaeffer [1] and later by Bergland et al. [2] in 1968 who introduced the terms “prefixed” and “postfixed” chiasms to designate optic chiasm location overlying either the tuberculum sellae (prefixed) or dorsum sellae (postfixed).
The position of the chiasm with respect to the sella in patients with sellar lesions may have significance on clinical presentation. Thereby, bitemporal hemianopia has been reported to appear more likely when a sellar lesion compresses a prefixed chiasm [2–4].
Optic chiasm position is also relevant in terms of surgical planning for sellar and parasellar tumors, given that a prefixed chiasm can limit surgical access to the tumoral area. This appears to be more critical in so-called minimally invasive or keyhole approaches, such as the trans-eyebrow supraorbital approach [5, 6].
The usually accepted classification of optic chiasm location in three groups, prefixed, normal and postfixed chiasm, is mostly based on cadaveric or imaging studies (MRI studies) in normal patients. To the best of our knowledge, there are few published studies describing the preoperative optic chiasm location in patients with pathological conditions (such as sellar or parasellar tumors that can distort the optic chiasm location) or studying the impact of optic chiasm location on the extent of resection of tumors in the sellar area. Likewise, optic nerve length has not been studied to date as a variable to be considered to predict the extent of tumor resection. However, optic nerve length is a quantitative variable, can be less affected than optic chiasm location by interobserver variability and may provide more accurate information than the optic chiasm location.
The aim of the study was to compare the predictive value of the optic nerve length and optic chiasm location on the extent of resection of large craniopharyngiomas when using the trans-eyebrow supraorbital approach.
Methods and materials
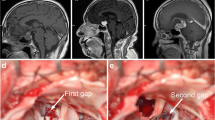
We included adult patients with a diagnosis of large craniopharyngioma (defined as those occupying the suprasellar cistern and the third ventricle) in the study; all of them underwent surgery through a trans-eyebrow supraorbital approach between January 2009 and January 2015 by the senior author (R.P.). The trans-eyebrow supraorbital approach was chosen in all cases because of the tumor size and surgeon experience. Data were obtained retrospectively from medical records, clinical notes and imaging studies of all patients and included age, sex, preoperative visual disturbances and postoperative visual improvement, whether the large craniopharyngioma was mainly cystic or solid on T2-weighted MRI and optic chiasm location (per the literature as defined by Schaeffer and later by Bergland: prefixed chiasm overlying the tuberculum sellae, normal chiasm located above the diaphragm sellae and postfixed chiasms above the dorsum sellae) and the vertical extension of the craniopharyngiomas in all three groups in mm above the sella (horizontal line from anterior to posterior tubercle. We also recorded the values of optic nerve length that were measured routinely during surgery and the surgery-related complications. An independent blinded radiologist measured the optic nerve length on axial preoperative MRI using heavily T2-weighted images. Optic nerve length was defined as the intracranial segment of the right optic nerve between two landmarks: the optic chiasm and the optic nerve entrance into the optic canal (Fig. 1).
Postoperative MRI was performed in all cases approximately 6 weeks after surgery to detect residual tumor. Resection rates were defined in terms of percentage of tumor resection after review by an independent radiologist measured using image fusion and volumetric software (BrainLab iPlan Cranial 2.6; BrainLab AG, Feldkirchen, Germany).
Surgical procedure
Surgery was performed via a right supraorbital trans-eyebrow approach in all cases. The skin incision extended medial to the supraorbital nerve groove (usually at the junction of the medial one third and lateral two thirds of the eyebrow) and lateral to the eyebrow tail, 1 cm below the superior temporal line. A neuronavigation (Medtronic Stealth Station) system was routinely used to design the limits of the craniotomy, mainly in the location of the frontal sinus, to prevent sinus opening during surgery. A 2.5-cm-wide, 1.5-cm-high craniotomy was performed parallel to the orbital rim. The dura was incised in a curvilinear manner following the bone edge and retracted toward the orbital roof. Following the floor of the anterior fossa, and by using gentle retraction, the arachnoid cisterns were opened and frontal lobe relaxation obtained. Then, the tumor, both optic nerves and chiasm, both internal carotid arteries and both anterior cerebral arteries and the anterior communicating artery were visualized. Prior to tumor removal, the right optic nerve length was routinely measured. We defined the optic nerve length as the distance of the intracranial segment of the right optic nerve between two landmarks: the optic chiasm and the optic nerve entrance into the optic canal. The nerve was measured using a navigation system under a microscope. All measurements were made to the nearest 0.5 mm. The tumor was approached through the subchiasmatic and optico-carotid triangles, and the lamina terminalis was opened in all cases to remove the tumor.
A 30-degree endoscope was also routinely used to confirm adequate tumor resection. After dural closure, the bone flap was secured with three titanium microplates and the skin closed in two layers with absorbable sutures.
Statistical analysis
Statistical analysis was performed using a linear regression model, with the objective of obtaining a prediction formula of the percentage of extent of resection as a function of optic nerve length measured intraoperatively. We used the Durbin Watson test to detect the presence of autocorrelation.
Unpaired t-test was used to compare the optic nerve length and percentage of resection in the three groups of optic chiasm location.
The statistical program SPSS, version 16.0 (SPSS, Inc., Chicago, IL), was used to evaluate our results with significance set at p < 0.05.
Results
Our series (Table 1) included 21 patients with large craniopharyngiomas; 12 were males and 9 females (mean age: 51.6 years; range: 22–67 years). Preoperatively, 14 patients showed some deficit in anterior pituitary hormone: 11 deficit in adrenal function, 10 deficit in thyroid function, 7 deficit in somatotroph function, and 2 deficit in gonadal function. Seven patients had diabetes insipidus preoperatively. All patients had visual disturbances, with 14 suffering bitemporal hemianopia and 7 unilateral visual deficit. On MRI, 11 patients had predominantly cystic lesions, whereas in 10 cases appeared mainly solid. On preoperative MRI 15 patients were considered to have an optic chiasm in normal location, 3 cases had a prefixed chiasm, and the remaining 3 had a postfixed chiasm.
Optic nerve length measurement obtained during surgery (Table 2) gave a mean length of 10.6 mm (±2.4) with a range between 14.1 and 5.7 mm.
Optic nerve length was significantly shorter in patients suffering preoperative hemianopia (9.8 mm ± 2.4) than in patients presenting with unilateral visual acuity deficit (12.1 mm ± 1.3) (p = 0.032). Optic nerve length measurements obtained during surgery were confirmed in all cases by an independent blinded radiologist on preoperative MRI.
Extent of resection
Eleven (52.3%) patients had complete resection, three patients had a resection of 80% or less (two patients 80%, one patient 75%), and the remaining 7 (33.3%) had a percentage of resection between 80 and 90%. Anatomically residual tumor was usually intrasellar and under the chiasm.
A normally positioned chiasm was associated with a mean percentage of resection of 93.6% ± 7.6, prefixed chiasm 78.3 ± 2.8 and postfixed chiasm 100% in all three cases. All three groups of optic chiasm location presented statistically significantly different optic nerve lengths: prefixed chiasm, mean optic nerve length 7.4 mm ± 1.7; normal chiasm, 10.6 mm ± 1.8; postfixed chiasm, 13.6 mm ± 0.5 (unpaired t-test p < 0.05).
We found a statistically significant different percentage of resection between cases with a prefixed and normal chiasm (unpaired t-test p = 0.0041) and prefixed and postfixed chiasms (unpaired t-test p = 0.002), but we did not find significant differences in the percentage of resection between normal and postfixed cases (p = 0.18).
In all patients with postfixed chiasms, 100% resection was obtained, but no patient with prefixed chiasm had complete resection (range 75–80%). In the group of normal position of the optic chiasm a wide range of percentages of resection was observed (75–100%). In all patients presenting an optic nerve length ≥11 mm complete resection was achieved.
As a result of a linear regression model (Fig. 2), we obtained a prediction formula of the percentage of extent of resection as a function of optic nerve length (p < 0.0001).
The coefficient of determination of this linear regression model was R2 = 0.77.
The calculated Durbin-Watson statistic of 1.71 discarded any autocorrelation: there were no other variables (including whether the craniopharyngiomas was cystic or solid or had vertical extension) that could affect the percentage of resection.
No differences due to any variable were observed to affect the postoperative visual improvement. We did not find preoperative MRI appearance of large craniopharyngiomas (cystic or solid on T2 weighted images) to be related with the extent of resection.
Two cases of superficial infection were recorded and were solved with a course of antibiotics. No CSF leak or opening of the frontal sinus during surgery occurred in any case in our series.
Postoperatively, 15 patients (71.4%) had improvement of visual acuity. Postoperatively, 15 patients received replacement of anterior pituitary hormone and 12 patients had diabetes insipidus.
Discussion
Craniopharyngiomas are generally slow-growing tumors with a propensity to adherence to adjacent structures, such as the optic chiasm. Accordingly, it has been accepted that craniopharyngioma patients, and mostly if they harbor large craniopharyngiomas, tend to present prefixed optic chiasms due to the tumoral effect [7]. Although this assertion could be intuitively accepted, to our knowledge a detailed study on this topic has not been published. In our series of large craniopharyngiomas, we did not observe this trend: only three patients harbored a prefixed chiasm, with most of the patients presenting a normal optic chiasm location (15 patients, 71.4% of cases).
The terms prefixed and postfixed were first applied to the optic chiasm location in 1924 [1] in a study by Bergland et al. in 1968 [2]. They defined as prefixed those chiasms overlying the tuberculum sellae and postfixed those overlying the dorsum sellae. Occurrence of prefixed and postfixed chiasm varies between 5 to 15 and 11 to 17%, respectively [3, 8, 9].
However, the classical classification of optic chiasm location as prefixed, normal and postfixed presents some limitations [10]: it is based on cadaveric measurements and could not correctly reflect the real situation in vivo (e.g., some anatomical studies, compared to data collected in MRI studies, showed that the proportion of prefixed optic chiasms was underestimated in cadaveric measurements) [11, 12], and also most of the MRI studies using this classification have been performed in healthy volunteers without studying cases with tumors.
Complete removal of large craniopharyngiomas has been reported in 31 to 100% of cases [11, 13–20]. Knowing whether the chiasm is normal, prefixed or postfixed has been previously reported to be of great value in this surgery in order to predict the surgical anatomy and consequently select the most appropriate surgical approach to obtain a greater resection [21–23].
In the surgery of large craniopharyngiomas, optic chiasm location is usually of less concern in the transsphenoidal approach than in the subfrontal or pterional approaches, but in the trans-eyebrow supraorbital approach, where most of the resection is obtained from the prechiasmatic area and the opticocarotid triangle, the position of the chiasm can be critical to obtain enough surgical working space [7, 9, 24–26] and an increased percentage of tumor resection.
The trans-eyebrow supraorbital approach provides a minimally invasive subfrontal approach through which a wide variety of pathologies (from vascular to tumoral cases) can be approached [27–31].
However, when using the trans-eyebrow supraorbital approach, particularly in patients with a prefixed chiasm, gaining access to the infraoptic and subchiasmatic regions as operative windows can be difficult and challenging, and surgical handling of these areas during tumor resection can lead to a significant increase in operative morbidity and mortality [15, 32].
In our study, we found significant differences in the extent of resection of large craniopharyngiomas between the prefixed chiasm group of patients and the two other groups (postfixed and normal optic chiasm location). However, no differences in the extent of resection were observed between patients with normal and postfixed chiasm.
A possible displacement of the optic chiasm by the tumor should be taken into consideration because it in turn may influence the length of the optic nerves, e.g., if the chiasm is lifted upwards it may appear prefixed, yet the optic nerve length could be greater than in some normal chiasms. However, the optic nerve length directly correlates with whether the chiasm is prefixed or post-fixed. As could be expected, shorter nerves are associated with prefixed chiasms and longer nerves with post-fixed ones, but in our study we observed there was a large number of cases with normal optic chiasm locations that needed to be studied more in depth to decide whether they might benefit from surgery.
A thorough study of the normal optic chiasm location patients (15 out of 21 patients of our series) showed a great range of percentages of resection (75–100%) in this group. We considered it relevant to find an anatomic variable that could explain such a variety in the percentage of resection in this group. Due to the retrospective nature of the study, we obtained limited information of each case from the clinical and imaging records, but we found that the optic nerve length had been intraoperatively measured and recorded in all cases because of the interest for a different study. Thus, we used these measurements to calculate a linear regression formula of the extent of resection as a function of optic nerve length.
When we compared the optic chiasm location and optic nerve length in our series; all three groups of optic chiasm locations presented statistically significantly different optic nerve lengths, revealing a good correlation between both parameters. However, optic nerve length measurements in the normal optic chiasm location group (ONL = 10.6 mm ± 1.8) allowed us to refine our prediction of the extent of resection according to the linear regression model obtained. According to this model, and using optic nerve length in the normal optic chiasm location group, we obtained an 87% resection in 9-mm optic nerve length patients, 90.5% resection in 10-mm optic nerve length patients and 100% resection in 11-mm optic nerve length patients. In our opinion, optic nerve length appears to be a more accurate tool than optic chiasm location to predict the extent of resection in normal optic chiasm location patients, and other surgical approaches should be considered especially when the optic nerve is short.
Noticeably, optic nerve length only could be considered a real predictive variable if it could be measured before surgery on preoperative MRI. However, conventional MRI has limitations in obtaining reliable optic nerve length in large suprasellar tumors [11]. This possibly is due to optic nerve atrophy or little intensity difference between the optic nerve and tumor, perhaps due to edematous changes of the optic pathways caused by chemical irritation of the tumor or cyst content [33].
Although some studies [22, 25] have evaluated the location of anterior optic pathways in patients with sellar and parasellar tumors, on preoperative MRI, using heavily T2-weighted images with 95% positive identifications, they have included different types of tumors (pituitary tumors, craniopharyngiomas and meningiomas) with different surgical approaches. Besides, no quantitative analysis of resection was performed according to preoperative MRI measurement of optic nerve length. Although in our analysis preoperative MRI measurement of optic nerve length was only recorded after intraoperative data had been obtained, we may suggest that optic nerve length measurement on preoperative MRI can provide a more precise prediction of large craniopharyngiomas’ extent of resection.
The position of the chiasm with respect to the sella is also of clinical significance since a suprasellar lesion is more likely to compress a prefixed chiasm than a postfixed one [34]. In our study, we did not observe differences in clinical presentation among the three groups of optic chiasm location. When we studied the clinical effect according to intraoperative optic nerve length values, we observed that optic nerve length was significantly shorter in patients suffering preoperative hemianopia (9.8 mm ± 2.4).
Two cases of superficial infection were recorded and were solved with a course of antibiotics. No cerebrospinal fluid (CSF) leak or opening of the frontal sinus during surgery occurred in any case in our series, although this complication has been reported in up to 4% of patients operated on via the supraorbital craniotomy [30]. This absence of CSF leakage cases can be attributed to the use of neuronavigation systems during the preoperative planning of craniotomy, which helped us to avoid the frontal sinus during surgery.
Postoperatively, 15 of our patients (71.4%) had improvement of visual acuity to a functional level although some series report improvement of visual function in all patients. All patients in our series had persistence or increase of preoperative hormonal deficit data comparable with that reported in the literature [23].
Although we are aware of the small number of patients included in this series and its retrospective nature, we consider that according to our data, optic nerve length can emerge as a valid and easy tool to be used preoperatively to predict the extent of resection of large craniopharyngiomas operated on through the trans-eyebrow supraorbital approach. However, despite the predictive value of optic nerve length, the extent of tumor resection has also been described to depend on the anatomical location of craniopharyngiomas [35, 36], leading to recommendations on surgical resection. The results obtained from this methodology can only be applied to patients operated on through the trans-eyebrow supraorbital approach; however, similar studies could be performed to validate the optic nerve length’s role in predicting the extent of resection of large craniopharyngiomas in the most commonly used surgical approaches.
Conclusion
According to the results observed in our series, classification of the optic chiasm location as prefixed, normal and postfixed remains a useful tool to predict the extent of resection of large craniopharyngiomas in patients operated on via the trans-eyebrow supraorbital approach. However, direct preoperative measurement of optic nerve length was more accurate in predicting the percentage of resection, especially in cases with normal optic chiasm location.
The derived prediction formula of the percentage of extent of resection as a function of optic nerve length could be useful in estimating the extent of resection of large craniopharyngiomas operated on via the trans-eyebrow supraorbital approach.
Abbreviations
- MRI:
-
Magnetic resonance imaging
- CSF:
-
Cerebrospinal fluid
References
Schaeffer J (1924) Some points in the regional anatomy of the optic pathway, with especial reference to tumors of the hypophysis cerebri and resulting ocular changes. Anat Rec 28:243–279
Bergland RM, Ray BS, Torack RM (1968) Anatomical variations in the pituitary gland and adjacent structures in 225 human autopsy cases. J Neurosurg 28:93–99
Griessenauer CJ, Raborn J, Mortazavi MM, Tubbs RS, Cohen-Gadol AA (2014) Relationship between the pituitary stalk angle in prefixed, normal, and postfixed optic chiasmata: an anatomic study with microsurgical application. Acta Neurochir 156:147–151
Maira G, Anile C, Rossi GF, Colosimo C (1995) Surgical treatment of craniopharyngiomas: an evaluation of the transsphenoidal and pterional approaches. Neurosurgery 36:715–724
Krause F (1908) Surgery of the brain and spinal cord in our experience [Chirurgie des Gehirns und Rückenmarks nach eigenen Erfahrungen]. Urban & Schwarzenberg, Berlin
Prat-Acín R, Galeano-Senabre I, Pancucci G, Evangelista R, Ayuso-Sacido A, Botella C (2013) Supraorbital trans-eyebrow craniotomy and fluorescence-guided resection of fronto-basal high grade gliomas. Clin Neurol Neurosurg 115:1586–1590
Beretta F, Andaluz N, Chalaala C, Bernucci C, Salud L, Zuccarello M (2010) Image-guided anatomical and morphometric study of supraorbital and transorbital minicraniotomies to the sellar and perisellar regions: comparison with standard techniques. J Neurosurg 113:975–981
Doyle AJ (1990) Optic chiasm position on MR images. AJNR Am J Neuroradiol 11:553–555
Gulsen S, Dinc AH, Unal M, Canturk N, Altinors N (2010) Characterization of the anatomic location of the pituitary stalk and its relationship to the dorsum sellae, tuberculum sellae and chiasmatic cistern. J Korean Neurosurg Soc 47:169–173
Won HS, Han SH, Oh CS, Lee JI, Chung IH, Kim SH (2010) Topographic variations of the optic chiasm and the foramen diaphragma sellae. Surg Radiol Anat 32:653–657
Long H, Qi ST, Song Y, Pan J, Zhang XA, Yang KJ (2014) Topographic variations of the optic chiasm and the pituitary stalk: a morphometric study based on midsagittal T2-weighted MR images. Surg Radiol Anat 36:775–781
Yilmazlar S, Kocaeli H, Eyigor O, Hakyemez B, Korfali E (2008) Clinical importance of the basal cavernous sinuses and cavernous carotid arteries relative to the pituitary gland and macroadenomas: quantitative analysis of the complete anatomy. Surg Neurol 70:165–174
Ammirati M, Samii M, Sephernia A (1990) Surgery of large retrochiasmatic craniopharyngiomas in children. Childs Nerv Syst 6:13–17
Bhagwati SN, Deopujari CE, Parulekar GD (1990) Lamina terminalis approach for retrochiasmal craniopharyngiomas. Childs Nerv Syst 6:425–429
Fahlbusch R, Honegger J, Paulus W, Huk W, Buchfelder M (1999) Surgical treatment of craniopharyngiomas: experience with 168 patients. J Neurosurg 90:237–250
Fatemi N, Dusick JR, de Paiva Neto MA, Malkasian D, Kelly DF (2009) Endonasal versus supraorbital keyhole removal of craniopharyngiomas and tuberculum sellae meningiomas. Neurosurgery 64:269–284
Gazzeri R, Nishiyama Y, Teo C (2014) Endoscopic supraorbital eyebrow approach for the surgical treatment of extraaxialand intraaxial tumors. Neurosurg Focus 37:E20
Kang JK, Song JU (1988) Results of the management of craniopharyngioma in children. An endocrinological approach to the treatment. Childs Nerv Syst 4:135–138
Weiner HL, Wisoff JH, Rosenberg ME, Kupersmith MJ, Cohen H, Zagzag D, Shiminski-Maher T, Flamm ES, Epstein FJ, Miller DC (1994) Craniopharyngiomas: a clinicopathological analysis of factors predictive of recurrence and functional outcome. Neurosurgery 35:1001–1010
Wilson DA, Duong H, Teo C, Kelly DF (2014) The supraorbital endoscopic approach for tumors. World Neurosurg 82:S72–80
Rhoton AL, Renn WH, Harris FS (1985) Microsurgical anatomy of the sellar region and cavernous sinuses. In: Rand RW (ed) Microneurosurgery. Mosby, St. Louis, p 113
Saeki N, Murai H, Kubota M, Fujimoto N, Iuchi T, Yamaura A, Sunami K (2002) Heavily T2 weighted MR images of anterior optic pathways in patients with sellar and parasellar tumours—prediction of surgical anatomy. Acta Neurochir 144:25–35
Van Effenterre R, Boch AL (2002) Craniopharyngioma in adults and children: a study of 122 surgical cases. J Neurosurg 97:3–11
Carmel P (1993) Transcranial approach in craniopharyngiomas. In: Appuzo ML (ed) Brain surgery, vol 1. Churchill Livingstone, New York, pp 339–357
Eda M, Saeki N, Fujimoto N, Sunami K (2002) Demonstration of the optic pathway in large pituitary adenoma on heavily T2 weighted MR images. Br J Neurosurg 16:21–29
Tang CT, Baidya NB, Ammirati M (2013) Endoscope-assisted supraorbital approach to the retroinfundibular area: a cadaveric study. Neurosurg Rev 36:249–256
Fischer G, Stadie A, Reisch R, Hopf NJ, Fries G, Böcher-Schwarz H, van Lindert E, Ungersböck K, Knosp E, Oertel J, Perneczky A (2011) The keyhole concept in aneurysm surgery: results of the past 20 years. Neurosurgery 68(1 Suppl Op):45–51
McLaughlin N, Ditzel Filho LF, Shahlaie K, Solari D, Kassam AB, Kelly DF (2011) The supraorbital approach for recurrent or residual suprasellar tumors. Minim Invasive Neurosurg 54:155–161
Raza SM, Garzon-Muvdi T, Boaehene K, Olivi A, Gallia G, Lim M, Subramanian P, Quinones-Hinojosa A (2010) The supraorbital craniotomy for access to the skull base and intraaxial lesions: a technique in evolution. Minim Invasive Neurosurg 53:1–8
Reisch R, Perneczky A (2005) Ten-year experience with the supraorbital subfrontal approach through an eyebrow skin incision. Neurosurgery 57:242–255
van Lindert E, Perneczky A, Fries G, Pierangeli E (1998) The supraorbital keyhole approach to supratentorial aneurysms: concept and technique. Surg Neurol 49:481–489
Tawk RG, Binning MJ, Thomas JM, Siddiqui AH, Grand W (2014) Transciliary supraorbital approach (eyebrow approach) for resection of retrochiasmatic craniopharyngiomas: an alternative approach, case series, and literature review. J Neurol Surg A Cent Eur Neurosurg 75:354–364
Nagahata M, Hosoya T, Kayama T, Yamaguchi K (1998) Edema along the optic tract: useful MRfinding for the diagnosis of craniopharyngiomas. AJNR 19:1753–1757
Naheedy MH, Haag JR, Azar-Kia B, Mafee MF, Elias DA (1987) MRI and CT of sellar and parasellar disorders. Radiol Clin North Am 25:819–847
Morisako H, Goto T, Goto H, Bohoun CA, Tamrakar S, Ohata K (2016) Aggressive surgery based on an anatomical subclassification of craniopharyngiomas. Neurosurg Focus 41:E10
Yaşargil MG, CurcicM KM, Siegenthaler G, Teddy PJ, Roth P (1990) Total removal of craniopharyngiomas. Approaches and long-term results in 144 patients. J Neurosurg 73:3–11
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Our study is retrospective; for this type of study formal consent is not required.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional informed consent was obtained from all individual participants for whom identifying information is included in this article.
Rights and permissions
About this article
Cite this article
Prat, R., Galeano, I., Evangelista, R. et al. Trans-eyebrow supraorbital approach in large suprasellar craniopharyngioma surgery in adults: analysis of optic nerve length and extent of tumor resection. Original article. Acta Neurochir 159, 873–880 (2017). https://doi.org/10.1007/s00701-017-3148-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-017-3148-6