Abstract
Background
Meralgia paresthetica is a mononeuropathy of the lateral femoral cutaneous nerve (LCFN). Surgical treatment involves transection or decompression of the LCFN. There is no clear consensus on the superiority of one technique over the other. We performed a systematic review of the literature to answer this question.
Methods
Eligible studies included those that compared neurolysis versus neurectomy for the treatment of meralgia paresthetica after failure of conservative therapy. Our outcome of interest was resolution of symptoms. We performed a computerized search of MEDLINE (PubMed; all years) and of the Cochrane Central Register of Controlled Trials. Eligible studies had to include the words “meralgia paresthetica” and “surgery.” All patients regardless of age were included, and there was no language restriction. We then reviewed the articles’ titles and abstracts. All studies that compared neurolysis to neurectomy were included in the analysis.
Results
Of the studies identified, none were randomized controlled trials. There were two German language articles that were translated by a third researcher.
Each study was evaluated by two independent researchers who assigned a level of evidence according to American Association of Neurologist algorithm and also performed data extraction (neurolysis vs. neurectomy and resolution of pain symptoms). Each study was found to be level four evidence.
Conclusion
After reviewing the data, there was insufficient evidence to recommended one method of treatment over the other. This highlights the importance of keeping a national registry in order to compare outcomes between the two methods of treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Meralgia paresthetica (MP) is a mononeuropathy of the lateral femoral cutaneous nerve (LFCN), which innervates the cutaneous distribution along the anterolateral thigh. The incidence has been estimated to be approximately 32.6 per 100,000 person-years [24]. MP most frequently is associated with symptoms of numbness, tingling, or burning that may be exacerbated by standing or extending the hip [30]. It usually occurs as a result of compression of the nerve as it courses deep to the inguinal ligament. Obesity tends to be the greatest risk factor, although trauma and external compression from tight fitting clothing have been noted to predispose to MP as well [7, 24].
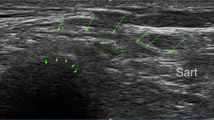
History and physical examination findings are usually sufficient to make the diagnosis of MP. In cases where the diagnosis is less clear, electrodiagnostic testing using either somatosensory evoked potentials or nerve conduction studies may be helpful [18, 26]. Additionally, injections containing corticosteroids and/or local anesthetic may be both diagnostic and therapeutic [34]. Finally, there is a growing body of literature suggesting the use of ultrasound (US) to diagnose MP [23, 31].
In most cases of MP, conservative measures including weight loss and loosening of tight fitting clothing are generally effective. In other cases, US has proven beneficial with some using it to guide corticosteroid/anesthetic injections and even perform radiofrequency ablation of the LCFN [1, 13, 15, 17, 32]. However, in refractory cases, surgical treatment may be considered. The two most frequent procedures performed are neurectomy and neurolysis. In neurectomy, the LCFN is transected at the level of the inguinal ligament. In neurolysis, incising the inguinal ligament decompresses the LCFN.
There have been only a handful of studies directly comparing outcomes from these two procedures [4, 5, 9, 10, 12, 14, 33]. Prior systematic reviews have attempted to provide guidance on surgical decision making but were unable to do so because of the paucity of data from well-designed studies [16]. This review seeks to provide an updated analysis of the current literature and to offer comments on how best to discern between these two approaches in the setting of an aggravating and painful disease.
Methods
Study selection criteria
Eligible studies included those that compared neurolysis (NL) versus neurectomy (NR) for the treatment of MP after failure of conservative therapy. Our outcome of interest was symptom resolution. We performed a computerized search of MEDLINE (PubMed; all years) and of the Cochrane Central Register of Controlled Trials. Eligible studies were required to include the words “meralgia paresthetica” and “surgery.” All patients, regardless of age, were included, and there was no language restriction. We then reviewed the articles’ titles and abstracts. All studies that compared NL to NR were included in the analysis. Of the studies identified, none were randomized controlled trials. There were two German-language articles, which were translated by a third reviewer.
Data synthesis and analysis
Each study was evaluated by two independent reviewers who assigned a level of evidence according to the American Association of Neurologist algorithm (Table 1). These reviewers also performed data extraction (neurolysis vs. neurectomy and resolution of pain symptoms). Every study was found to be class IV evidence. Given the low quality of evidence, a meta-analysis was not done. Similar to previous works, we used the grading of recommendations, assessment, development, and evaluations (GRADE) system to assess the body of evidence as a whole [3, 27]. We used the GRADE guidelines (Table 2), which include study design, inconsistency, risk of bias, indirectness, publication bias, imprecision, effect size, dose response, and confounders to designate the quality of the overall body of evidence.
Results
Our initial search returned 141 articles. None of these were duplicates. After screening the titles and abstracts, we found only seven articles that directly addressed the question of neurectomy vs. neurolysis for the treatment of meralgia paresthetica (Fig. 1). One of these articles was written in German and was translated by a third reviewer. All articles were evaluated by two independent reviewers and assigned a class of evidence. A fourth reviewer resolved any discrepancies.
Study discussion
A meta-analysis was not possible due to the low quality of evidence. The seven studies identified were heterogeneous in their inclusion criteria and outcome measurements. Several studies excluded cases with traumatic or secondary injury while others included these in their analysis. Some studies evaluated for complete relief of pain while others evaluated for varying degrees of symptom resolution. All of the studies were observational, and all but one were retrospective analyses. Overall, the majority of authors felt that neurectomy was superior to neurolysis. Only one paper favored neurolysis over neurectomy.
De Ruiter et al. authored two papers on the subject. The first article is a retrospective cohort study of patients who failed conservative therapy and underwent surgery for treatment of MP. Traumatic cases were excluded. Outcomes were assessed by means of a questionnaire, and symptom relief was defined as complete, partial, or no relief. A total of 22 procedures were carried out in 16 patients. Four patients underwent NL followed by NR after poor response. These patients were given two separate questionnaires to assess each procedure. The questionnaire response rate was 100%. Mean follow-up for the NR group was 93 months while for the NL group was 16 months. Results showed that 60% of those undergoing NL for the first time (primary neurolysis) had complete pain relief while 75% of those undergoing NR for the first time (primary neurectomy) had complete pain relief [10].
The second paper by De Ruiter et al. is a prospective cohort study where those with a clinical diagnosis of idiopathic MP refractory to conservative therapy were followed and assessed for symptom relief following surgery. The patients were allowed to choose NR or NL after a discussion of the risks/benefits of each. A total of 22 patients underwent 23 procedures (15 NR and 8 NL). The primary outcome was symptom resolution as described by the Likert scale (Likert 1 = complete recovery; Likert 2 = almost complete recovery). Patients were assessed 6 weeks postoperatively in the clinic. Pain relief with a Likert score of 1 or 2 was seen in 37.5% of primary neurolysis cases and in 93.3% of primary neurectomy cases, which was statistically significant (p = 0.0283) [9].
Benezis et al. performed a retrospective analysis of their experience with those who had failed conservative treatment for MP. One hundred sixty patients underwent a total of 167 procedures. Of these, 153 underwent NL while 14 underwent NR. NR was performed after failed neurolysis (3 cases) or because of neuroma or considerable narrowing of the nerve (11 cases). Selection criteria were different from other studies in that they did not exclude those who had a history of prior surgery or traumatic injury. Outcomes assessed were symptom improvement and surgical outcome satisfaction. This was done by means of a questionnaire. Mean follow-up was 98 months. In the group that received NL, 61% reported a complete recovery and complete satisfaction, and 17% reported partial relief and satisfaction. Of those in the NR group, 35.7% either improved or were satisfied with the surgery [4].
Van Eerten et al. performed a retrospective cohort study of those with MP who had failed conservative therapy. The outcome assessed was degree of relief. Twenty-one patients (10 NL and 11 NR) underwent surgery with a mean follow-up of 46 months after NL and 116 months after NR. In the NL group, 60% enjoyed complete or partial relief while 100% in the NR group had the same result [33].
Emamhadi et al. describe a prospective analysis of patients with a diagnosis of MP after failing conservative therapy that went on to receive surgery (5 NL and 9 NR). Those who had a known etiology of secondary MP were excluded from the analysis. Follow-up was 18 months in all patients. Outcomes assessed include pain relief and recurrence of symptoms. All of those undergoing NR had complete pain relief without recurrence while all of those undergoing NL had recurrence of symptoms within 9 months.
Ivins described his experience treating MP. Eight people underwent a total of 12 procedures. Follow-up ranged from 3 to 6 years. The outcome assessed was duration of relief of symptoms. NL was performed a total of four times. Each time, there was initial relief with recurrence of symptoms between 2 and 14 months. The eight NRs were successful with the patients enjoying persistent relief.
Finally, Antoniadis et al. performed a retrospective cohort study on 29 patients who underwent a total of 33 procedures. The outcome assessed was degree of pain relief. Follow-up was 32 months in the NL group and 87 months in the NR group. Overall, 72% of the NL group and 82% of the NR group had complete or partial relief of symptoms [2].
Body of evidence (GRADE Score)
After assessing all of the appropriate studies and grading their quality of evidence, we rated each article according to its strengths and weaknesses. We then assigned a score to the overall body of evidence according to the system proposed by Balshem et al. [3]. Our assessment of the overall body of evidence of the surgical treatment for MP was very low. We had initially estimated the quality of evidence to be low given that all of the studies were observational studies. This was then modified because of the risk of bias. In many of the studies evaluated, the person evaluating for improvement in symptoms was an unmasked treater. There were also inconsistencies in inclusion and exclusion criteria between studies. Furthermore, the way that treatment success was defined varied between studies. For all of these reasons, we downgraded the quality of evidence to very low.
Discussion
MP is a painful condition that often responds to conservative measures. Haim et al. highlighted this when they documented that 82 of 85 consecutive patients with idiopathic MP responded to non-surgical therapy [14].
However, the best treatment for idiopathic MP that has failed conservative measures is still debated within the literature [8]. Early papers mention both NL and NR as possible treatments [19, 25]. There are several case series that strongly endorse neurolysis as the procedure of choice and report good to excellent outcomes in up to 77–88% of cases [11, 21, 22, 28, 29]. Others such as Macnicol et al. had poor results with NL and reported that it was successful in less than half of their adult patients [20]. The success of NR also varies in the literature with some reporting pain relief without recurrence rates as high as 96% while others have documented less success [34]. There are very few papers that compare the result of NL versus NR, and these are all very poor quality evidence. Given this fact, we are unable to make a recommendation as to which method of surgical treatment is superior. It does appear that both neurolysis and neurectomy are still in use throughout the peripheral nerve surgery community. Those espousing neurectomy point to the histopathological changes of the LFCN at the inguinal ligament in those with a diagnosis of MP and theorize that these changes are a “pain generator” that needs to be resected [6, 33]. Dr. Kline summarized these thoughts well when he observed that MP seems to respond less favorably to NL than other compression neuropathies. In a comment on van Eerten et al.’s paper comparing NR versus NL, he explained: “It may be that in some cases, enough intraneural change has occurred to produce a painful neuropathy with hypesthesia; if so, neurolysis will not suffice and resection of the ‘pain generator’ is the most efficacious step in management” [33].
Those promoting the use of neurolysis point to the success of neurolysis in other entrapment syndromes. Others raise concern for the potentially detrimental effects of transecting a peripheral nerve. A well-known result of neurectomy is the resultant anesthesia in the distribution of the LCFN. What is unknown is the overall contribution of this postoperative anesthesia to patients’ quality of life. Most of the studies included in this systematic review did not look at postoperative numbness as a primary or secondary outcome. However, those conducted by deRuiter et al. did include postoperative numbness in their outcomes. Their first study found that after neurectomy, 3/8 patients reported improved numbness, 3/8 reported new numbness, 1/8 had unchanged numbness, and 1/8 suffered worse numbness. Out of the three that had numbness as a result of neurectomy, one found it frequently bothersome but was overall satisfied with outcome while the other two were unbothered and satisfied with outcome. The one patient with worsened numbness also had worsened pain and was the only patient to be dissatisfied with the procedure. In their second publication addressing neurolysis versus neurectomy, the bothersome scale was used to assess postoperative numbness. They found a value of 1.4 (±1) out of a possible value of 6. This showed that in their cohort of patients postoperative numbness was not particularly bothersome.
A review of the literature comparing NR to NL revealed that six studies favored NR as a treatment, and one study favored NL (Benezis et al.). It is important to note that the only study in favor of NL reserved NR only for those with neuroma formation or deformation of the nerve. This made comparison groups unequal. Also important to note is the heterogeneity between studies with different inclusion/exclusion criteria, difference in outcome assessment, and evaluation of outcomes by unmasked treaters.
Conclusion
There is insufficient evidence to recommend either NR or NL over the other. Both methods of surgical treatment appear to be well documented and accepted within the literature for the relief of symptoms in those with idiopathic MP. To assess for the superiority of one treatment over the other, high-quality studies are necessary. If feasible, a randomized controlled trial (RCT) would be ideal to appropriately address this question. Unfortunately, the amount of time and money necessary to conduct such a study is often prohibitive. A potential alternative is a prospective national registry that may serve to answer the questions of whether NR or NL is a superior treatment for MP and other questions.
References
Ahmed A, Arora D, Kochhar AK (2016) Ultrasound-guided alcohol neurolysis of lateral femoral cutaneous nerve for intractable meralgia paresthetica: a case series. Br J Pain 10(4):232–237
Antoniadis G, Braun V, Rath S, Moese G, Richter HP (1995) Meralgia paraesthetica and its surgical treatment. Nervenarzt 66(8):614–7
Balshem H, Helfand M, Schünemann HJ et al (2011) GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 64(4):401–406
Benezis I, Boutaud B, Leclerc J, Fabre T, Durandeau A (2007) Lateral femoral cutaneous neuropathy and its surgical treatment: a report of 167 cases. Muscle Nerve 36(5):659–663
Benini A (1992) Meralgia paresthetica. Pathogenesis, clinical aspects and therapy of compression of the lateral cutaneous nerve of the thigh. Schweiz Rundsch Med Prax 81(8):215–21
Berini SE, Spinner RJ, Jentoft ME, Engelstad JK, Staff NP, Suanprasert N, Dyck PJB, Klein CJ (2014) Chronic meralgia paresthetica and neurectomy: a clinical pathologic study. Neurology 82(17):1551–1555
Boyce JR (1984) Meralgia paresthetica and tight trousers. JAMA 251(12):1553
Cheatham SW, Kolber MJ, Salamh PA (2013) Meralgia paresthetica: a review of the literature. Int J Sports Phys Ther 8(6):883–93
De Ruiter GCW, Kloet A (2015) Comparison of effectiveness of different surgical treatments for meralgia paresthetica: results of a prospective observational study and protocol for a randomized controlled trial. Clin Neurol Neurosurg 134:7–11
De Ruiter GCW, Wurzer JAL, Kloet A (2012) Decision making in the surgical treatment of meralgia paresthetica: neurolysis versus neurectomy. Acta Neurochir (Wien) 154(10):1765–1772
Ducic I, Dellon AL, Taylor NS (2006) Decompression of the lateral femoral cutaneous nerve in the treatment of meralgia paresthetica. J Reconstr Microsurg 22(2):113–118
Emamhadi M (2012) Surgery for meralgia paresthetica: neurolysis versus nerve resection. Turk Neurosurg 22(6):758–762
Fowler IM, Tucker AA, Mendez RJ (2012) Treatment of meralgia paresthetica with ultrasound-guided pulsed radiofrequency ablation of the lateral femoral cutaneous nerve. Pain Pract 12(5):394–8
Haim A, Pritsch T, Ben-Galim P, Dekel S (2006) Meralgia paresthetica: a retrospective analysis of 79 patients evaluated and treated according to a standard algorithm. Acta Orthop 77(3):482–486
Hurdle MF, Weingarten TN, Crisostomo RA, Psimos C, Smith J (2007) Ultrasound-guided blockade of the lateral femoral cutaneous nerve: technical description and review of 10 cases. Arch Phys Med Rehabil 88(10):1362–1364
Khalil N, Nicotra A, Rakowicz W (2008) Treatment for meralgia paraesthetica. Cochrane Database Syst Rev. doi:10.1002/14651858.CD004159.pub2
Kim JE, Lee SG, Kim EJ, Min BW, Ban ong S, Lee JH (2011) Ultrasound-guided lateral femoral cutaneous nerve block in meralgia paresthetica. Korean J Pain 24(2):115–118
Lagueny A, Deliac MM, Deliac P, Durandeau A (1991) Diagnostic and prognostic value of electrophysiologic tests in meralgia paresthetica. Muscle Nerve 14(1):51–6
Lee FC (1941) An osteoplastic neurolysis operation for the cure of meralgia paresthetica. Ann Surg 113(1):85–94
Macnicol MF, Thompson WJ (1990) Idiopathic meralgia paresthetica. Clin Orthop Relat Res 270–274
Nahabedian MY, Dellon AL (1995) Meralgia paresthetica: etiology, diagnosis, and outcome of surgical decompression. Ann Plast Surg 35(6):590–4
Nouraei SAR, Anand B, Spink G, O’Neill KS (2007) A novel approach to the diagnosis and management of meralgia paresthetica. Neurosurgery 60(4):696–700
Onat SS, Ata AM, Ozcakar L (2016) Ultrasound-guided diagnosis and treatment of meralgia paresthetica. Pain Physician 19(4):E667–9
Parisi TJ, Mandrekar J, Dyck PJB, Klein CJ (2011) Meralgia paresthetica: relation to obesity, advanced age, and diabetes mellitus. Neurology 77(16):1538–1542
Rattananan W, Thaisetthawatkul P, Dyck PJB (2014) Postsurgical inflammatory neuropathy: a report of five cases. J Neurol Sci 337(1–2):137–40
Seror P, Seror R (2006) Meralgia paresthetica: clinical and electrophysiological diagnosis in 120 cases. Muscle Nerve 33(5):650–4
Sieg EP, Payne RA, Hazard S, Rizk E (2016) Evaluating the evidence: is phrenic nerve stimulation a safe and effective tool for decreasing ventilator dependence in patients with high cervical spinal cord injuries and central hypoventilation? Childs Nerv Syst 32(6):1033–1038
Siu TLT, Chandran KN (2005) Neurolysis for meralgia paresthetica: an operative series of 45 cases. Surg Neurol 63(1):19–23
Son B, Kim D-R, Kim I, Hong J, Sung J, Lee S (2012) Neurolysis for meralgia paresthetica. J Korean Neurosurg Soc 51(6):363–6
Stookey B (1928) Meralgia paraesthetica. JAMA 90(21):1705
Suh DH, Kim DH, Park JW, Park BK (2013) Sonographic and electrophysiologic findings in patients with meralgia paresthetica. Clin Neurophysiol 124(7):1460–1464
Tagliafico A, Serafini G, Lacelli F, Perrone N, Valsania V, Martinoli C (2011) Ultrasound-guided treatment of meralgia paresthetica (LFCN). J Ultrasound Med 1341–1346
Van Eerten PV, Polder TW, Broere CA (2015) Operative treatment of meralgia paresthetica: transection versus neurolysis. Neurosurgery 37(1):63–65
Williams PH, Trzil KP (1991) Management of meralgia paresthetica. J Neurosurg 74:76–80
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
This article does not contain any studies with human participants performed by any of the authors.
Additional information
Comments
The authors are to be commended on rigorously reviewing the literature for studies comparing the efficacy of decompression versus neurectomy of the lateral femoral cutaneous nerve in patients with a clinical diagnosis of merralgia paresthetica refractory to non-surgical therapies. It is humbling to realize that despite 131 years having elapsed since the first surgical procedure for this condition, we still have no definitive study comparing the two types of surgical procedure for this condition. The authors make the very good point that surgical registries should be kept so that such a comparison can be made going forward. Although not the major focus of this article, I wonder if the authors would like to comment on the potential downside of performing a neurectomy that results in long-lasting analgesia in the distribution of the lateral femoral cutaneous nerve, which can produce unpleasant paresthesias. The authors also mention steroid injections as both a treatment and diagnostic test but do not mention injections of local anesthetic to help in diagnosing this condition. The authors also might want to at least mention the growing ultrasound literature showing the ability to both help diagnose and surgically treat this condition by being able to preoperatively localize the nerve, which can sometimes be a challenge to find.
Michel Kliot
Illinois, USA
Rights and permissions
About this article
Cite this article
Payne, R., Seaman, S., Sieg, E. et al. Evaluating the evidence: is neurolysis or neurectomy a better treatment for meralgia paresthetica?. Acta Neurochir 159, 931–936 (2017). https://doi.org/10.1007/s00701-017-3136-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-017-3136-x