Abstract
Background
Anterior cranial fossa dural arterio-venous fistulas (DAVFs) represent 6% of all intracranial DAVFs; characteristically they show an aggressive behaviour with high risk of intracranial haemorrhage. Peculiar anatomical features, such as feeding by the ethmoidal arteries and the pattern of venous drainage (frequently with varices that mimic aneurysmal dilatation), can be evaluated in detail only by digital subtraction angiography (DSA), which represents the “gold standard” in the diagnosis of such cranial fistulas. Recent technological developments in endovascular management of this type of DAVF have partially reduced the morbidity risk related to this modality of treatment. Our purpose is to present our experience in the surgical management of 14 patients with anterior cranial fossa DAVFs, with attention paid to the possible role of preoperative embolisation in these cases and to the surgical technique.
Method
Between 1999 and 2015, 14 patients with anterior cranial fossa DAVFs were submitted to surgery in two neurosurgical departments; the mean age was 63 years old; nine DAVFs caused intracranial haemorrhage (subarachnoid haemorrhage in three cases, intracerebral haemorrhage in six cases). Pre-operative embolisation was attempted in an early case and was successfully done in one recent case. In all patients, the surgical approach chosen was a pterional craniotomy with a low margin on the frontal bone in order to gain the exposure of the anterior cranial fossa and especially of the olphactory groove region; the resection of the falx at its insertion on the crista galli was needed in five cases in order to get access to the contralateral afferent vessels. Cauterisation of all the dural feeders on and around the lamina cribrosa was needed in all cases; venous dilatations were evident in eight patients (in seven out of nine patients with ruptured DAVF and in one out of five patients with unruptured DAVF) and were removed in all cases. One patient harboured an ophthalmic artery aneurysm, which was excluded by clipping.
Results
One patient died 5 days after surgery due to the severity of the pre-operative haemorrhage. Postoperative DSA showed the disappearance of the DAVF and of the venous pseudo-aneurysms in all cases. Clinical outcome was favourable (without neurological deficits) in 11 patients; three patients presented an unfavourable clinical outcome, due to the severity of the initial haemorrhage.
Conclusions
Surgical exclusion of the anterior cranial fossa DAVFs still represents the gold standard for such lesions, due to low post-operative morbidity and to complete protection against future rebleedings; endovascular techniques may help the surgeon in complex cases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dural arterio-venous fistulas (DAVFs) of the anterior cranial fossa represent a rare and peculiar subgroup of DAVFs (5.8% of all type of DAVFs), characterised by an aggressive haemorrhagic pattern (91%) [6]. The recent trend in the clinical management of DAVF has been significantly affected by the endovascular techniques, especially for the treatment of cavernous sinus, transverse sinus and torcula DAVFs. This trend towards a wider use of endovascular techniques can be easily related to the recent development of new modalities and materials employed: transarterial and transvenous techniques in particular, together with new microcatheters [3, 12–14, 22]. DAVFs of the anterior cranial fossa have been previously described as an exception to the trend towards endovascular management: the risk of embolisation of the central retinal artery, the small calibre of vessels and the risk of reflux of embolising agents into the cerebral circulation were the main deterrents for endovascular surgeons [1]. More recently, further improvements of technology and techniques created the basis for the endovascular management of such lesions and small clinical series are becoming available in the literature [1, 3, 4, 12, 13, 15, 16, 22, 23].
Surgical management of anterior cranial fossa DAVFs carries a low morbidity rate [11] but some pitfalls can complicate their surgical exclusion; thorough analysis of digital subtraction angiography (DSA) and especially the characteristics of afferent arteries, the venous drainage pattern, particularly if a venous aneurysm is present, are all determinant factors for the final complete exclusion of the DAVF and for a good clinical results.
In this article we report our results in the surgical management of anterior cranial fossa DAVFs in two neurosurgical departments, in order to describe the DSA characteristics that determine the surgical strategy for the exclusion, the surgical technique and the postoperative outcome (at discharge and at follow-up).
Materials and methods
Patient population
Between 1999 and 2015, 14 consecutive patients who were referred to the Neurosurgical Departments of Verona and Bergamo for treatment of anterior cranial fossa DAVFs were identified via a retrospective chart review. The following parameters were recorded: there were 12 men and 2 women; the mean age was 63 years (range, 54-80 years); the clinical presentation was haemorrhage in nine patients; computed tomography (CT) scan at the admission demonstrated an intracerebral haemorrhage in six patients (with acute subdural haematoma in one case and intraventricular haemorrhage in one case); three patients were admitted to the emergency room while in coma; a subarachnoid haemorrhage (SAH) was detected in the other three patients. The diagnosis was incidental in five cases and was related to epilepsy in one case, to persistent headache in two cases, to visual disturbances in one case. In the last patient, the DAVF was incidentally diagnosed during the follow-up after a sub-total surgical removal of a cavernous sinus meningioma.
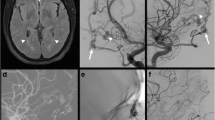
All patients were submitted to preoperative DSA in order to visualise: (1) the main features of the afferent arteries (anterior and posterior ethmoidal arteries, monolateral or bilateral; transosseus branches of the internal maxillary artery and of the external carotid artery, monolateral or bilateral; meningeal branches of the external carotid artery); (2) the venous drainage pattern (direction of the drainage to the superior sagittal sinus, to the cavernous sinus, to the sylvian veins or to the Rosenthal vein), the possible presence of a venous varix and the side of the drainage (Fig. 1). More recently, CT angiography was also introduced as a preoperative diagnostic tool, which can be helpful in planning the surgical approach. Clinical and angiographical details of the DAVFs are reported in Table 1. A venous varix was evident in eight cases and it was double in one of them; more specifically, the venous varix was present in seven out of nine patients with ruptured DAVF and in one out of five patients with unruptured DAVF. A left paraclinoid unruptured aneurysm was also detected during DSA in one patient.
A 68-year-old patient with a ruptured anterior cranial fossa DAVF; DSA showed bilateral ethmoidal feeders—only right feeders are shown (a, b) and monolateral right maxillary feeders (c, d) to the DAVF (white arrowhead shows the point of fistula from the ethmoidal and maxillary feeders) and a single venous varix. Postoperative DSA showed complete exclusion of the DAVF (e, f)
Preoperative embolisation was attempted in an early case of this series, but technical difficulties (mainly catheter–dependent) did not allow occlusion of the feeders. More recently, a preoperative partial embolisation with n-butyl-2-cyanoacrylate (nBCA) was conducted in one patient with bilateral ethmoidal feeders, in order to facilitate the surgical exclusion of the DAVF; a left anterior ethmoidal artery was embolised without neurological deficits (Fig. 2); the patient was submitted to surgery 3 weeks later.
A 55-year-old patient with a ruptured anterior cranial fossa DAVF with an intracerebral haematoma; DSA showed the presence of bilateral ethmoidal feeders (left ethmoidal artery, shown in a and c, white arrowheads). The patient was submitted to embolisation of the left anterior ethmoidal artery; white arrowheads show the origin of the vessel embolised (b, d)
Surgical technique
The surgical approaches were represented by a pterional and bifrontal craniotomy. The former consisted in a modification of the regular pterional craniotomy with a low margin on the frontal bone in order to gain the exposure of the anterior cranial fossa and of the olfactory groove region (where the DAVF usually presents the point of fistula) and a medial extension to the superior sagittal sinus (SSS) in order to get access to the interhemispheric fissure. According to the preoperative DSA, if bilateral afferent arteries were evident, a section of the falx was done near to its insertion on the crista galli to obtain exposition of the contralateral anterior cranial fossa. The removal of the crista galli was made with a diamond high-speed drill in order to control bleeding from transosseus afferent arteries (branches of the internal maxillary artery); haemostasis on the bone was obtained with the heat generated by the drill and bone wax.
The standard bifrontal craniotomy permits a simultaneous exposition of the anterior cranial base and the olfactory groove region on both sides and of the bilateral interhemispheric fissure.
The exclusion of the fistula started with the cauterisation of the main arteries directed to the point of the fistula; the draining vein was sectioned only when it became dark and soft; the lamina cribrosa was sealed with surgicel and fibrin glue and—if present—the venous varix was removed. If an intracerebral haemorrhage was present, a careful partial evacuation of the haematoma was done first in order to relax the brain enough to get access to the anterior cranial base without excessive retraction on the frontal lobe; after the exclusion of the fistula, the haematoma was completely removed together with the venous varix (Fig. 3) The surgical exclusion of the paraclinoid aneurysm required an optic foraminotomy and partial intradural clinoidectomy with diamond high-speed drill to obtain exposure of the distal carotid ring and of the origin the ophthalmic artery.
Surgical procedure for the exclusion of the anterior cranial fossa DAVF: through a right pterional approach, the olphactory groove region is identified (a) and ethmoidal feeders are cauterised (b). If a contralateral feeder is present, a small incision of the antero-inferior segment of the falx is made in order to access the contralateral olphactory groove region (c). An interhemispheric approach is used to get access to the feeders and the draining vein (d), and finally to remove the venous varix (e); at the end of the procedure, the olphactory groove is covered with surgicel and fibrin glue (f)
Outcome and follow-up
After the surgical procedure, most patients were submitted to DSA to confirm the surgical exclusion of the DAVF. Outcome was reported at discharge, at 6 months and beyond (follow-up range, 24-72 months) according to the modified Rankin score (mRS); the clinical outcome was divided into favourable (0-2) and unfavourable (3-6).
Results
Clinical outcome was favourable in 11 cases; in two cases, the mRS at discharge was 4 due to the poor clinical grade at the admission; one patient died 5 days after surgery due to the severity of the bleeding at admission. Surgical details and clinical outcome are reported in Table 2.
The surgical approach chosen was the pterional craniotomy in 13 case (93%) and the bifrontal craniotomy in one case (7%). The pterional approach was right-sided in all patients except in two cases, due to the presence of a left paraclinoid aneurysm in one case and to a left venous varix in the other case. The complete exclusion of the DAVF required the incision of the falx to expose the contralateral anterior cranial base in five cases; in all cases the venous varices were removed. The patient submitted to exclusion of the unruptured carotid-ophthalmic aneurysm, together with the exclusion of the DAVF, did not present visual deficits after the procedure. No intraoperative complications were reported during the surgical procedures.
Postoperative DSA was carried out in 12 patients and confirmed the exclusion of the DAVF in all of them and also the exclusion of the carotid-ophthalmic aneurysm in one patient. DSA was not performed in two cases: the first one due to early postoperative death, the second one due to the age and the co-morbidity of the patient.
Discussion
Anterior cranial fossa DAVFs represent a small percentage of cranial DAVFs with peculiar differences: first of all male predominance, which is confirmed in our series (6:1) and correlates well with a recent new embryologically based classification of DAVFs [6]: fistulas located at the lateral epidural space, which includes the lamina cribrosa, have a strong male predominance and an aggressive pattern.
In our series, the main clinical manifestation was haemorrhage (64%), which is lower than previously reported [1, 11, 18]; a possible reason for this lower bleeding rate is the large availability of CT and magnetic resonance imaging that nowadays are performed widely even in scarcely symptomatic patients. The explanation for such a bleeding rate has been previously related to the draining pattern of the DAVF: the point of fistula is usually located at the lamina cribosa and is basically a connection between the ethmoidal arteries (most frequently the anterior) and the fronto-basal veins. Furthermore, as recently reported by Gross et al. [7], it should be kept in mind that these DAVFs may drain posteriorly and into the deep venous circulation; this pattern of drainage can be related with haemorrhages remote from the fistula site. The haemodynamic stress to which the fragile pial basal veins are exposed determinates a progressive structural modification of the vessel towards the formation of a venous aneurysm [11]. This kind of venous anomaly is highly related with the risk of bleeding. In our series, patient with a bleeding DAVF presented a venous varix in 77% of cases (double in one patient), whereas patients with unruptured DAVFs showed this characteristic less frequently (20%). This strong relation with an aggressive natural history had justified an interventional management for these lesions [9].
Treatment options described are mainly surgical; however, recent trends towards a minimally invasive approach have forced the evolution of endovascular techniques, in order to overcome the three main problems in endovascular management of anterior cranial fossa DAVFs: the risk of embolisation of the central retinal artery, the small calibre of vessels that have to be navigated and the risk of systemic diffusion of embolic agents [11]. The approaches to the DAVF described are transarterial and transvenous; according to different authors each technique presents some advantages and disadvantages. The transarterial technique presents a shorter route to the target but requires navigation of the ophthalmic artery towards the ethmoidal artery; nowadays, new microcatheter technologies often permit safe positioning of the catheter well beyond the origin of the central retinal artery [1, 16]. The embolisation materials used are various: glue (nBCA, Onyx), particles or detachable coils. The use of Onyx present a higher risk of complications due to the requirement of partial reflux of the material upstream in order to allow pushing the Onyx forward [16]; however, Onyx does not polymerise and it precipitates as the solvent diffuses. The latter characteristic permits a prolonged injection and exit vein occlusion [21]. By contrast, polyvinyl glue as nBCA is injected forward towards the venous side of the shunt; therefore, reflux is not part of the technique [1]. However, nBCA may fail to penetrate deeply enough to achieve a cure. Defreyne et al. [3] successfully used the transvenous route to the DAVF; however, the length and difficulties of the navigation, especially inside the venous varix, discourage most endovascular surgeons. Despite these technological ameliorations, the rate of complete occlusion in larger series (63.3-91%) [1, 12, 13] is still lower than after surgical occlusion. Therefore, due to the technical skill requirements and the rarity of the pathology, the endovascular management should be limited only to high volume centres and should be probably accepted as a preoperative treatment.
In our series, the occlusion was verified with DSA in 12 out of 14 cases (one patient died 5 days after surgery, the other patient was not submitted to DSA because of age and comorbidities). The final outcome was dramatically influenced by the clinical presentation: all patients with unruptured DAVF submitted to surgery showed a favourable outcome, whereas a good outcome was achieved in six out of nine patients (67%) with a bleeding DAVF. As previously reported, an unfavourable outcome is mainly related to the initial haemorrhagic event, which prevents a clinical amelioration after surgery [9, 11, 18]. In a haemorrhagic patient, frequently with intracerebral haematomas, surgical management is mandatory due to the possibility of both occluding the fistula and evacuating the haematoma, frequently located near the venous varix.
The surgical approaches described are various, according to the preference and confidence of the surgeon [10, 11, 17–19]; the target is to expose the lamina cribrosa and the crista galli in order to visualise the afferent vessels and the venous drainage on the surface of the anterior cranial fossa. The technological evolution of the surgical instrumentation recently permits new routes to the olphactory groove region to be created: Magro et al. [17] reported the use of a transfrontal sinus approach to exclude anterior cranial fossa DAVFs, whereas Ding et al. [5] described a minimally invasive endoscopic interhemispheric approach to treat such vascular malformations. In our experience, a pterional approach with a low inferior limit on the frontal bone was adequate to expose the region of interest and was the approach chosen in 93% of the procedures. When a bilateral supply to the fistula is present, the incision of the falx becomes necessary to visualise the contralateral half of the olfactory groove region; thus, the perspective offered by the pterional approach can be very useful. The medial extension of the bone flap towards and beyond the midline is sometimes helpful when direct access to the interhemispheric fissure is needed [11, 19]. The characteristics of the surgical technique must be tailored to the preoperative DSA: in our series, a bilateral supply of the fistula required an incision of the falx and drilling of the crista galli in 36% of cases in order to completely exclude the DAVF.
In our series, we also report a case with a concomitant unruptured left paraclinoid aneurysm. The coexistence of both intracranial DAVF (of any kind) and aneurysms are reported in 13-21% of cases [8]; more specifically, in a literature review by Chen et al. [2], the presence of both an anterior cranial fossa DAVF and aneurysm was reported in 14 cases; the authors also reported a case of anterior cranial fossa DAVF and an unruptured ophthalmic aneurysm that were treated respectively with Gamma Knife and embolisation. Reinard et al. [20] reported another case of an unruptured ophthalmic aneurysm and a contralateral anterior cranial fossa DAVF: during surgery for the DAVF exclusion, clipping of the contralateral aneurysm was attempted but finally abandoned because of excessive brain retraction; 28 days after discharge a scheduled DSA demonstrated an 85% reduction in the size of the aneurysm that finally was not treated. In our case the approach chosen was ipsilateral to the aneurysm in order to get an easier access to the aneurysm itself; the exclusion of the DAVF, which presented bilateral ethmoidal feeders, required also the incision of the anterior-inferior segment of the falx in order to visualise and cauterise the contralateral ethmoidal arteries. The exclusion of both the DAVF and the aneurysm was achieved and confirmed at the DSA without visual disturbances for the patient.
Conclusions
Anterior cranial fossa DAVFs are rare vascular malformations exhibiting an aggressive natural history, mainly due to the peculiar pattern of the venous drainage of the fistula. Endovascular management may represent a valid option in the management of such lesions, but should be possibly limited to a preoperative use. In our opinion, the surgical management of this type of DAVF must be considered as the main treatment option because of the higher rate of fistula exclusion and the very low morbidity risk. In order to obtain a good surgical result, a careful preoperative planning is mandatory (especially if bilateral supply is evident at the DSA) in order to tailor the surgical strategy on the DAVF architecture. Finally, anterior cranial fossa DAVFs are frequently related to intracerebral haematomas that can be evacuated in the same surgical procedure.
References
Agid R, Terbrugge K, Rodesch G, Andersson T, Soderman M (2009) Management strategies for anterior cranial fossa (ethmoidal) dural arteriovenous fistulas with an emphasis on endovascular treatment. J Neurosurg 110:79–84
Chen Z, Zhu G, Feng H, Tang W, Wang X (2008) Dural arteriovenous fistula of the anterior cranial fossa associated with a ruptured ophthalmic aneurysm: case report and review of the literature. Surg Neurol 69:318–321
Defreyne L, Vanlangenhove P, Vandekerckhove T, Deschrijver I, Sieben G, Klaes R, Kunnen M (2000) Transvenous embolization of a dural arteriovenous fistula of the anterior cranial fossa: preliminary results. AJNR Am J Neuroradiol 21:761–765
Deng JP, Li J, Zhang T, Yu J, Zhao ZW, Gao GD (2014) Embolization of dural arteriovenous fistula of the anterior cranial fossa through the middle meningeal artery with Onyx. Clin Neurol Neurosurg 117:1–5
Ding D, Starke RM, Crowley RW, Liu KC (2015) Interhemispheric approach for endoscopic ligation of an anterior cranial fossa dural arteriovenous fistula. J Clin Neurosci 22:1969–1972
Geibprasert S, Pereira V, Krings T, Jiarakongmun P, Toulgoat F, Pongpech S, Lasjaunias P (2008) Dural arteriovenous shunts: a new classification of craniospinal epidural venous anatomical bases and clinical correlations. Stroke 39:2783–2794
Gross BA, Moon K, Kalani MY, Albuquerque FC, McDougall CG, Nakaji P, Zabramski JM, Spetzler RF (2016) Clinical and anatomic insights from a series of ethmoidal dural arteriovenous fistulas at the Barrow Neurological Institute. World Neurosurg 93:94–99
Gross BA, Ropper AE, Du R (2012) Cerebral dural arteriovenous fistulas and aneurysms. Neurosurg Focus 32:E2
Hashiguchi A, Mimata C, Ichimura H, Morioka M, Kuratsu J (2007) Venous aneurysm development associated with a dural arteriovenous fistula of the anterior cranial fossa with devastating hemorrhage—case report. Neurol Med Chir 47:70–73
Latini F, Basma J, Ryttlefors M, Krisht AF (2014) Epidural skull base approach for dural arteriovenous fistulas (DAVF) of the anterior and middle cranial fossa. Acta Neurochir (Wein) 156:93–95
Lawton MT, Chun J, Wilson CB, Halbach VV (1999) Ethmoidal dural arteriovenous fistulae: an assessment of surgical and endovascular management. Neurosurgery 45:805–810
Lee B, Mehta VA, Amar AP, Tenser MS, Mack WJ (2014) Transarterial embolization of an anterior fossa cranial base dural arteriovenous fistula. Neurosurg Focus 37:1
Li C, Wu Z, Yang X, Li Y, Jiang C, He H (2014) Transarterial treatment with Onyx of Cognard type IV anterior cranial fossa dural arteriovenous fistulas. J Neurointervent Surg 6:115–120
Li Q, Fang YB, Huang QH, Zhang Q, Hong B, Zhao WY, Liu JM, Xu Y (2013) Transarterial embolization of dural arteriovenous fistulas of the anterior cranial fossa with Onyx. J Clin Neurosci 20:287–291
Lv X, Li Y, Liu A, Lv M, Jiang C, Wu Z (2008) Endovascular embolization of dural arteriovenous fistulas of the anterior cranial fossa: three case reports. Neurol Res 30:852–859
Mack WJ, Gonzalez NR, Jahan R, Vinuela F (2011) Endovascular management of anterior cranial fossa dural arteriovenous malformations. A technical report and anatomical discussion. Interv Neuroradiol 17:93–103
Magro E, Engel D, Bojanowski MW (2014) Transfrontal sinus approach for an anterior cranial fossa, ethmoidal, dural arteriovenous fistula. Surg Neurol Int 5:172
Martin NA, King WA, Wilson CB, Nutik S, Carter LP, Spetzler RF (1990) Management of dural arteriovenous malformations of the anterior cranial fossa. J Neurosurg 72:692–697
Mayfrank L, Reul J, Huffmann B, Bertalanffy H, Spetzger U, Gilsbach JM (1996) Microsurgical interhemispheric approach to dural arteriovenous fistulas of the floor of the anterior cranial fossa. Minim Invasive Neurosurg 39:74–77
Reinard K, Basheer A, Pabaney A, Marin H, Malik G (2014) Spontaneous resolution of a flow-related ophthalmic-segment aneurysm after treatment of anterior cranial fossa dural arteriovenous fistula. Surg Neurol Int 5:S512–515
Rezende MT, Piotin M, Mounayer C, Spelle L, Abud DG, Moret J (2006) Dural arteriovenous fistula of the lesser sphenoid wing region treated with Onyx: technical note. Neuroradiol 48:130–134
Spiotta AM, Hawk H, Kellogg RT, Turner RD, Chaudry MI, Turk AS (2014) Transfemoral venous approach for Onyx embolization of anterior fossa dural arteriovenous fistulae. J Neurointervent Surg 6:195–199
Xianli L, Youxiang L, Aihua L, Ming L, Zhongxue W (2007) Transarterial embolization of dural arteriovenous fistulas of the anterior cranial fossa using onyx-18. A case report. Neuroradiol J 20:348–354
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Funding
No funding was received for this research.
Rights and permissions
About this article
Cite this article
Meneghelli, P., Pasqualin, A., Lanterna, L.A. et al. Surgical treatment of anterior cranial fossa dural arterio-venous fistulas (DAVFs): a two-centre experience. Acta Neurochir 159, 823–830 (2017). https://doi.org/10.1007/s00701-017-3107-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-017-3107-2