Abstract
Enterogenous cysts (ECs) are endodermal lesions resulting from splitting anomalies in the neuroenteric canal. We report the case of a 64-year-old patient who presented with a sudden headache followed by collapse. Brain computed tomography revealed a hyperdense lesion in the anterior part of the third ventricle with obstructive hydrocephalus. A presumptive diagnosis of colloid cyst was made and he underwent a right transcortical approach for lesion resection. The histopathological examination revealed an EC. ECs are common lesions in the cervical-thoracic spine but rare in the supratentorial compartment with only two previously described cases occurring in the third ventricle.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Enterogenous cysts (ECs) belong to a large group of developmental abnormalities denominated as epithelial cysts, particularly to the subgroup derived from the endodermal layer—endodermal cysts—accounting for 0.15–0.35% of all intracranial lesions [5]. Considering other well-known endodermal cystic lesions, namely colloid cysts, supratentorial ECs are rare lesions [2]. Although the majority of cases occur in the midline, only two third-ventricular ECs have been reported in the literature [2, 7].
We report the case of an EC mimicking a colloid cyst in clinical presentation, radiological features and macroscopic appearance.
Case report
A 64-year-old woman with no significant past medical history presented to her local emergency department after a sudden headache followed by a collapse with loss of consciousness and no recollection of subsequent events. She fully regained consciousness (to a Glasgow Coma Scale [GCS] score of 15/15) in the following hour and had no neurological impairments when she presented to hospital.
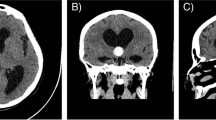
Brain computed tomography (CT) (Fig. 1) showed a hyperdense lesion in the third ventricle in the region of the Foramen of Monro. The patient was diagnosed with a colloid cyst with obstructive hydrocephalus and transferred to our neurosurgical centre, where surgical treatment was discussed and accepted by the patient.
The patient underwent a right frontal craniotomy and transcortical transventricular approach to the lesion with image guidance. A part solid part cystic lesion was found obstructing the Foramen of Monro. The lesion was adherent to the roof of the third ventricle and removed with suction, bipolar and sharp dissection. The septum pellucidum was widely opened at the end of the procedure and an external ventricular drain was placed in the ventricle prior to closure.
The patient had an uneventful post-operative recovery. The post-operative brain CT showed no residual lesion. The hydrocephalus had resolved (Fig. 2) and the ventricular drain was removed 3 days later.
The histopathology report revealed an enterogeneous cyst (Fig. 3).
At 6-month follow-up, the patient remained well with no clinical or radiological evidence of recurrence.
Discussion
The embryonic origin of ECs is a matter of discussion, even though an anomaly in the splitting of endoderm and ectoderm layers during neuroenteric canal separation during the 3rd week of gestation is the most accepted one [5]. Therefore, it is not surprising that the vast majority of these lesions are located in the inferior cervical and upper thoracic spine where the communication between these layers are more extensive [1]. In the intracranial compartment, the posterior fossa is the most common location in relation with the posterior closure of the notochord [6]. However, endodermal cystic lesions may appear in the supratentorial compartment through migration of germ layer remnants in Rathke’s cleft after their origin in Seessel’s pouch. Therefore, their appearance in the sella turcica (Rathke’s cleft cysts) or in the third ventricle (colloid cysts and enterogenous cysts) is justified [4].
Self-resolving sudden onset headache in the context of an obstructive hydrocephalus in a patient with a third-ventricular lesion occluding the Foramen of Monro is a neurosurgical emergency commonly related to colloid cysts. Nevertheless, this report highlights the variety of pathological entities that may present in this way. The differential diagnosis may include sellar-suprasellar lesions (e.g. craniopharyngioma), hypothalamic-chiasmatic lesions (e.g. opto-chiasmatic glioma in the paediatric population), choroid plexus lesions, ependymal cysts, arachnoid cyst, infectious cystic lesions, subependymoma, subependymal giant cell astrocytoma in a tuberous complex context, metastasis, lymphoma, vascular malformations of the plexus and other endodermal cystic lesions, such as enterogenous cyst [3].
Considering the clinical presentation with a collapse and brain CT revealing acute hydrocephalus, no magnetic resonance imaging was done before surgery. This patient presented with a hyperdense mass on non-contrast CT, although the typical appearance of an EC is of a low-density mass where contrast enhancement was difficult to access (Fig. 1 and Table 1). The tomographic density of a cyst is related to its protein content. Indeed, intraoperatively the cyst was found to have a gelatinous and thick fluid content, which supports the unusual hyperdense radiological appearance in this case.
Table 1 summarises the previously reported cases of third-ventricular enterogenous cysts. All reported patients are female, although our patient is older than the previous reported cases. This is consistent with the demographic characteristics of ECs in other locations (female preponderance and an age distribution between the 3rd and 7th decades) [6]. The surgical approach differed from the two previously published cases. There were two reasons why a transcortical approach was favoured in this case. First, the presence of acute hydrocephalus that would have rendered the transcallosal approach comparatively difficult and potentially requiring more brain retraction due to a tight inter-hemispheric fissure. Second, as the lesion was in contact with a dilated Foramen of Monro, there was less manipulation of the ipsilateral fornix due to a direct angle of view with a frontal transcortical approach. The transcortical approach has, however, been associated with an increased risk of seizures [8].
Conclusions
Acute hydrocephalus due to a third-ventricular lesion is a common presentation of colloid cyst. Nevertheless, other differential diagnoses should be considered, including ECs.
References
Al-Ahmed IH, Boughamoura M, Dirks P, Kulkarni AV, Rutka JT, Drake JM (2013) Neurosurgical management of neurenteric cysts in children. J Neurosurg Pediatr 11:511–517
Büttner A, Winkler PA, Weis S (1997) Endodermal cyst of the third ventricle: case report. Neurosurgery 40(4):832–835, discussion 835
Glastonbury CM, Osborn AG, Salzman KL (2011) Masses and malformations of the third ventricle: normal anatomic relationships and differential diagnoses. Radiographics 31(7):1889–1905
Graziani N, Dufour H, Figarella-Branger D, Donnet A, Bouillot P, Grisoli F (1995) Do the suprasellar neuroenteric cyst, the Rathke cleft cyst and the colloid cyst constitute a same entity? Acta Neurochir (Wien) 133:174–180
Hasegawa M, Nouri M, Nagahisa S, Hayashi T, Adachi K, Hirose Y, Abe M (2015) Neuroepithelial cyst of the fourth ventricle. Childs Nerv Syst 31(1):155–159
Rangarajan V, Mahore A, Patil MK, Shendarkar AD (2016) Supratentorial endodermal cysts—report of two cases. Asian J Neurosurg 11(3):310
Salvetti DJ, Williams BJ, Posthumus JS, Shaffrey ME (2014) Enterogenous cyst of the third ventricle. J Clin Neurosci 21(1):161–163
Sheikh AB, Mendelson ZS, Liu JK (2014) Endoscopic versus microsurgical resection of colloid cysts: a systematic review and meta-analysis of 1,278 patients. World Neurosurg 82(6):1187–1197
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organisation or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Patient consent
The patient has consented to submission of this case report to the journal
Additional information
This work has not been presented at a conference
Rights and permissions
About this article
Cite this article
Lavrador, J.P., Brogna, C., Vergani, F. et al. Third-ventricle enterogenous cyst presentation mimicking a colloid cyst: uncommon presentation of a rare disease and literature review. Acta Neurochir 159, 465–468 (2017). https://doi.org/10.1007/s00701-016-3052-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-016-3052-5