Abstract
Background
Increasing use of decompressive craniectomies has led to a corresponding number of cranioplasties performed to replace the subsequent bone defect created. We aimed to evaluate the morbidity associated with cranioplasty using an autologous bone flap sterilised in an autoclave.
Methods
We retrospectively analysed data from 149 patients who underwent cranioplasty following decompressive craniectomy during the time period January 1998 to December 2012. Autologous bone flaps were sterilised in an autoclave and stored in a refrigerator at a temperature of 8 degrees above zero until cranioplasty was performed. Complications were registered and patient data were analysed in order to identify risk factors for surgical site infection and bone flap resorption after cranioplasty. Only the patients with a follow-up period of >24 months were included in the analysis of bone flap resorption (110 patients).
Results
Surgical side infection occurred in only five patients (3.3%), whereas bone flap resorption developed in 22 patients (20%). The multivariate analysis of the presented data identified the operating time of >120 min (p = 0.0277; OR, 16.877; 95% CI, 1.364–208.906) and the presence of diabetes mellitus (p = 0.0016; OR, 54.261; 95% CI, 4.529–650.083) as independent risk factors of development of infection and the presence of ventriculo-peritoneal (VP) shunt (p < 0.0001; OR, 35.564; 95% CI, 9.962–126.960) as independent risk factor of development of the bone flap resorption.
Conclusions
Reimplantation of the autoclaved autologous bone flap following decompressive craniectomy is a simple and cheep alternative to other techniques and is available to any institution that provides autoclaving sterilisation services. This method is associated with a low rate of surgical site infection, but with a significant rate of the bone flap resorption.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Raised intracranial pressure (ICP) occurs in several brain disorders and is increasingly treated with decompressive craniectomy. The use of this procedure brings with it a corresponding number of cranioplasties performed to replace the subsequent bone defect created. Replacing the cranium is not only a cosmetic and protective measure but it also has curative effects. Cranioplasty can improve the alteration of cerebral blood flow, cerebrospinal fluid dynamics and clinically apparent neurological abnormalities. Cranioplasty may serve to treat the syndrome of the trephined or syndrome of the sinking skin flap, which have long been recognised [2, 10, 11, 18].
Various materials have been used to repair cranial defects (methyl methacrylate, titanium, hydroxyapatite, alumina ceramics, polyetheretherketone, polyethylene), nevertheless an autologous bone flap is often preferred to allograft due to its perfect match to the bone defect and its low cost [3, 8, 12, 21, 30, 31, 37–40] . Conventional methods of preserving the autologous bone flap involve subcutaneous implantation or cryopreservation [45]. Alternatively, the bone flap can be sterilised in an autoclave or using ethylene oxide and storage at operating room temperature [9, 22, 23, 26–28, 32]. The objectives of the study here presented were to identify the rate of complications (particularly two of the most serious complications—bone flap resorption and surgical site infection) following cranioplasty with an autologous bone flap sterilised in an autoclave in a large case series.
Materials and method
Data collection
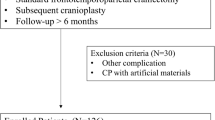
We identified 187 patients who underwent cranioplasty with an autoclaved bone flap following decompressive hemicraniectomy for various indications during a 15-year period (1 January 1998 to 31 December 2012) at the Neurosurgical Department, Faculty Hospital Pilsen, Czech Republic. Of these, 38 patients were excluded because they were lost to follow-up. One patient underwent cranioplasty bilaterally after bilateral decompressive hemicraniectomy. Thus, we retrospectively reviewed a cohort of 149 patients who had undergone 150 cranioplasties and had a follow-up period of >6 months. Only the patients with a follow-up period of >24 months were included in the analysis of bone flap resorption (110 patients).
All patients underwent cranioplasty with an autologous bone flap sterilised in an autoclave. Study approval was granted by the institutional review/ethics board.
Abstracted data included age, sex, indications for craniectomy, time between craniectomy and cranioplasty (days), operative time (minutes), method of bone flap fixation (sutures, miniplates), side of cranioplasty, medical comorbidities (diabetes mellitus, chronic obstructive pulmonary disease, in-hospital infection), prophylactic antibiotic treatment, subcutaneous drainage after cranioplasty and follow-up.
Perioperative and postoperative complications were recorded. Patient data were analysed in a search for predictive factors of surgical side infection and postoperative bone flap resorption. Bone flap resorption was evaluated with physical examinations and computed tomography (CT). CT was performed in patients with suspected resorption arising from the physical examinations.
Bone flap sterilisation and preservation
The bone flap removed during the initial decompressive hemicraniectomy was cleaned of any remaining soft tissue and boiled for 30 min in distilled water. The flap was then sterilised in a one-stage cycle (for 20 min at 121 °C) by using a steam autoclave (HS 6620 DR-II; Getinge Sterilization, Getinge Sweden). The bone flap, hermetically sealed in double sterilisation bags (Steriking; Wipack, Nastola, Finland) and labelled with the patient’s identification, was stored in a refrigerator at 8 °C. When the time between sterilisation and cranioplasty exceed 3 months the bone flap was autoclaved again immediately before cranioplasty.
Cranioplasty procedure
The sterilised bone flap was moved to the main operating table and placed in sterile gentamycin/NaCl solution. The skin was cut corresponding to the previous incision and dissected from the cranium, dura and from the temporal muscle. The temporal muscle was carefully dissected as a separate layer from the dura and the duraplasty, avoiding any cerebrospinal fluid (CSF) leak. The bone margins encasing the craniectomy defect were exposed and the bone flap was fixed using titanium miniplates and screws or nylon sutures. The galea was stitched together with the dura through several burr holes due to the superior revascularisation and revitalisation of the bone flap and as a prevention of subgaleal haematoma.
The temporal muscle was reattached to the bone flap with sutures with the use of small burr holes. In all cases a subgaleal drain was left in place for 24 h. All patients received a preoperative injection of cephalosporine antibiotics, which were discontinued at the time of the removal of the drain catheter.
Statistical analysis
Statistical analysis was performed using SW SAS (SAS Institute, Cary, NC, USA).
The descriptive statistics such as frequency, mean, standard deviation, variance, median, interquartile range, minimum, maximum were computed for investigated groups and subgroups. The non-parametric test (Wilcoxon two-sample test) was used for comparisons of the differences in investigated parameters such as age, operating time between given groups (bone flap resorption, surgical site infection). To evaluate the influence of the examined parameters on given outcome (bone flap resorption, surgical site infection) the univariate tests (chi-squared test or Fisher’s exact test) and the odds ratio + 95% confidence interval were computed. Multivariate analysis was performed using multivariate stepwise logistic regression. Statistical significance was determined at a level of 5%.
Results
Demographic and perioperative data are summarised in Table 1. Indications for hemicraniectomy followed by cranioplasty included trauma (73%), ischaemic stroke (17%), subarachnoid haemorrhage (7%) and intracerebral haemorrhage (3%). The mean time period (SD) between craniectomy and cranioplasty was 46 days (35.6), the mean operative time (SD) was 98 min (19.3). The bone flap was fixated during the operation with sutures (66%) or with miniplates (44%). Prophylactic antibiotics and subgaleal drainage were used in all patients. Ventriculo-peritoneal (VP) shunt had 14.7% of patients. Medical comorbidities were detected in 45.3% of patients. The follow-up period was a median of 11 months (range, 6–60) for all patients. The median follow-up period for bone flap resorption was 32 months (range, 24–60).
Complications are shown in Table 2. Complications included wound infection (5), bone flap resorption (22), wound dehiscence (1), removal of the bone flap because of brain oedema (1), extradural haematoma (3), subdural hydroma (5) and seizures (13).
Bone flap resorption was the most common complication (20%, 22/110). Four of the 22 patients with resorption underwent secondary cranioplasty using polymethyl-methacrylate (PMMA). The multivariate analysis of the presented data identified the presence of VP shunt (p < 0.0001; OR, 35.564; 95% CI, 9.962–126.960) as an independent risk factor for the development of resorption.
The fixation of the bone flap using sutures exhibited a higher rate of resorption, but this trend was not statistically significant (p = 0.161). Other variables did not influence the development of resorption.
Surgical site infection developed in 3.3% (5/150). The bone flap was removed and secondary cranioplasty using PMMA was later performed in all cases. The pathogens found and assumed to be responsible for the infection were: Styphylococcus aureus (3), Escherichia coli (1) and Peptostreptococcus species (1). The multivariate analysis of the presented data identified an operating time >120 min (p = 0.0277; OR, 16.877; 95% CI, 1.364–208.906) and the presence of diabetes mellitus (p = 0.0016; OR, 54.261; 95% CI, 4.529–650.083) as independent risk factors of the development of infection. No other variables predicted the infection rate.
Epileptic seizures were encountered in 13 patients (8.7%). No factors predicted a statistically significant rate of seizures.
Wound dehiscence, developed in one case, was associated with necrosis of the scalp. It was not necessary to remove the bone flap in this patient.
Three patients (2%) had an extradural haematoma necessitating surgical evacuation.
Fourteen patients (9.4%) died during the analysed follow-up period. The deaths were attributable to medical causes (five from pulmonary embolism, three from myocardial infarction, three from pneumonia, two from ischaemic stroke, two from sepsis).
Discussion
Despite cranioplasty being a relatively simple procedure, it has been shown to be associated with a high complication rate (12–50%) compared with the standard elective craniotomy (2–5%) [8, 4, 12, 40, 42, 43]. Some clinical studies showed that the complication rate used to be associated with the use of materials, the use of techniques for the storage of the bone flap prior to reconstruction and with the timing of cranioplasty [15, 23, 33, 36, 41].
Many types of materials can be used for cranial reconstruction, while autologous bone flap replacement, using the previously removed bone flap, is traditionally performed. Reimplantation of the patient’s own bone flap is the preferred method because of a theoretical decreased risk of immuno-rejection, its efficacy as a substrate for bone regrowth and revascularisation, its perfect match to the bone defect and its low cost [6, 45]. The most frequent preservation techniques involve cryopreservation and subcutaneous implantation in the abdominal pocket. However, several alternative methods of preserving the autologous bone flap were also presented.
In the study of Martin et al. [26] the previously cryopreserved bone flap was boiled for 20 min before surgical reinsertion.
Nagayama et al. [30] described a method of preserving the autologous bone flap through immersion in amikacin and cryopreservation at −16 °C in 206 cases.
Shimizu et al. [38] presented excellent results of cryopreservation with 10% dimethylsulphoxide as a cryoprotective agent in 24 cases.
To decrease the incidence of infection, autoclaving of previously cryopreserved bone graft before implantation is advocated by some authors [27, 32]. Autoclaving is also recommended in the treatment of infected craniotomies or when the bone flap comes into contact with the floor [9, 22].
Matsuno at al. [27] cryopreserved autologous bone flap in 100% ethanol at −20 °C and sterilised the flap in an autoclave before cranioplasty. Bone flap infection was noted in 25.9% of patients in this study.
Missori et al. [28] and Jho et al. [23] presented the effectiveness of ethylene oxide sterilisation of autologous bone flap with storage at operating room temperature.
This study presented the preservation technique through boiling, autoclaving and storing of the bone flap in a refrigerator at 8 °C as another simple alternative method available to any institution with autoclaving sterilisation services. The unavailability of a safe freezer container in our units was the main reason for the use of this technique. Despite having relatively satisfactory experience with this technique during the past 4 decades we knew that autoclaving used to be associated with a significant risk of resorption. This is why we particularly wanted to identify both resorption and infection rate along with its predictive factors in this large cohort of patients.
A surgical side infection (SSI) and bone flap resorption are two of the most serious complications associated with autologous cranioplasty. SSI is described particularly in patients after traumatic brain injury. The reported incidence of SSI among that population ranged from 0% to 38.5% [7, 19–21, 27, 30, 40]. If the bone flap is deep-frozen there is always the risk of contamination in a non-sterile environment. Bacteria can survive long-term freezing and still have considerable growth activity [32]. Moreover various freezing temperatures (raging from −16 °C to −84 °C) have been described in the literature [45]. Hence the subcutaneous pocket may be the preferred method in these patients because cryopreservation may have a higher infection rate [20]. By contrast, abdominal subcutaneous pocketing needs an additional surgical site and increased surgical time, thereby naturally increasing infection rates. Nevertheless, the meta-analysis showed that no difference exists between the infection rates of cryopreservation and subcutaneous preservation [45]. The infection rate for the above-mentioned alternative methods of preserving the bone flap ranged from 0% to 25.9 % [23, 26–28, 30, 32, 38].
In our series of 149 patients, surgical site infection only developed in five cases (3.3%). The infected bone flap was removed and secondary cranioplasty, using PMMA, was later performed in all five patients. None of these patients with secondary cranioplasty developed infection.
Prolonged operation time >120 min (p = 0.0277) was the significant risk factor of infection in our study, which corresponds well with recently published results [24, 25, 40]. The multivariate analysis also showed that the presence of diabetes mellitus significantly increased the risk of SSI (p = 0.0016). The low incidence of infection in our study could also be related to the prescribing of prophylactic antibiotics in all cases and the relatively short operating time (mean, 98 min; range, 55–175).
We did not find any statistically significant relationship between the timing of cranioplasty and the risk of SSI, which is in accordance with the meta-analysis published by Yadla et al. [45]. Neither did we detect any association between the risk of SSI and the aetiology of hemicraniectomy.
Bone flap resorption is a well known long-term complication after autologous bone cranioplasty with incidence varying from 2% to 17% in adults [17, 34, 37]. In paediatric populations, bone flap resorption is even reported to be as high as 81.8% [26]. In addition to young age, other factors, such as the presence of multiple fractures of the flap [37], the size of the flap [13], shunt operation [3] and the storage of the bone graft [37], have been suggested as possible reasons for the development of resorption.
Autoclaving bone flaps has previously been reported as a factor associated with resorption [1, 3, 16, 31]. Hallfeldt et al. [14] investigated the effects of different sterilisation techniques (gamma irradiation, ethylene oxide, ethanol, autoclaving) on osteoinductive properties of partially demineralised bone matrix. They found that only sterilisation by autoclaving showed no satisfactory new bone formation. Osawa et al. [32] evaluated the effect of freezing and autoclaving on bone morphology. While frozen bone showed similar microscopic features to normal fresh bone, in the autoclaved bone osteocytes were destroyed. Although the bone flap is devitalised after autoclaving, it is always the calcium apatite plate with a natural structure which should induce bone formation [32, 35, 44]. Bone flap incorporation and remodelling after cranioplasty is achieved by revascularisation, osteoconduction, resorption and osteogenesis [35].
Bone flap resorption was the most common complication in our study. It occurred in 22 patients (20%). It has become clear that autoclaving in combination with boiling significantly lessens the osteogenic potential of the flap and hence increases the risk of bone resorption. Furthermore, in cases of late cranioplasty (more than 3 months after craniectomy) the bone flap was resterilised before the operation.
In addition to the sterilisation procedure there are other factors which could influence the development of bone resorption in our patients. Several burr holes in the bone flap, through which we stitch galea with the dura due to the improved revascularisation and prevention of extradural collection, weakens the flap and hence probably raises the risk of resorption.
A higher rate of resorption in bone flaps larger than 75 cm2 than in smaller bone flaps was described by Grant et al. [13]. All our patients were decompressed with large hemicraniectomy (around 150 cm2), which may also partially explain the high resorption rate.
Revascularisation and osteoblast penetration into the reimplanted bone flap occur from the adjacent bone edges [35]. Therefore the direct contiguity between the edge of the craniotomy and the bone flap and firm fixation of the bone flap seem to be important factors [35]. The fixation of the bone flap by sutures (less firm fixation than with the use of miniplates) which was used in 66% of patients exhibited a trend towards a higher rate of resorption. Nevertheless it was not statistically significant (p = 0.161).
The multivariate analysis of our series identified the presence of VP shunt (p < 0.0001) as independent predictors of the development of resorption. The presence of permanent CSF shunt is associated with higher rates of bone flap resorption, particularly in a paediatric population [5, 26]. Shunt placement reduces ICP fluctuations and therefore negatively influences skull growth and may well contribute to resorption [5, 26]. Other variables, including the timing of cranioplasty and trauma patients, did not predict the development of bone flap resorption in this study.
Despite resorption occurring in 22 patients, it was only significant enough in four cases for it to be necessary to remove the bone flap and perform a secondary cranioplasty.
Schuss et al. [37] found that 60% of bone resorption after cranioplasty developed within the 1st year and no development was observed in patients with a follow-up period of over 5 years. Hence the follow-up period for resorption was determined from 24 to 60 months in our study.
Our study has several limitations. The data analysis was retrospective, so there may be all the anticipated deficiencies of a retrospective analysis including the loss of patient information and poor follow-up. These results represent only a single-centre experience. Despite the long time period (15 years) of the present study our surgical approach was standardised. This fact, in combination with the large number of patients, may outweigh some of these drawbacks.
Our complication rate of 38.7% reflects a significant level of morbidity associated with cranioplasty and is consistent with findings from other published series [8, 4, 12, 42]. It demonstrates the risks of this seemingly routine procedure. Therefore, when evaluating the need to perform decompressive craniectomy, the neurosurgeon should be aware that the patient is not only subject to the risk of the initial operation but also the risk of subsequent cranioplasty. The high complication rate of cranioplasty is one of the main reasons for performing osteoplastic decompressive craniotomy (hinge decompressive craniotomy) in our institution [29].
Conclusions
Reimplantation of the autoclaved autologous bone flap following decompressive craniectomy is a simple and cheep alternative to other techniques which is available to a majority of institutions. This method is associated with a low rate of surgical site infection, however with a significant rate of bone flap resorption. The overall complication rate was high in the present study, but comparable to other cranioplasty methods.
References
Abott KH (1953) Use of frozen cranial bone flaps for autogenous and homologous grafts in cranioplasty and spinal interbody fusion. J Neurosurg 10(4):380–338
Agner C, Dujovny M, Gaviria M (2002) Neurocognitive assessment before and after cranioplasty. Acta Neurochir (Wien) 144(10):1033–1040, discussion 1040
Asano Y, Ryuke Y, Hasuo M, Simosawa S (1993) Cranioplasty using cryopreserved autogenous bone. No To Shinkei 45(12):1145–1150
Bobinski L, Koskinen LO, Lindvall P (2013) Complications following cranioplasty using autologous bone or polymethylmethacrylate–retrospective experience from a single center. Clin Neurol Neurosurg 115(9):1788–1791
Bowers CA, Riva-Cambrin J, Hertzler DA 2nd, Walker ML (2013) Risk factors and rates of bone flap resorption in pediatric patients after decompressive craniectomy for traumatic brain injury. J Neurosurg Pediatr 11(5):526–532
Cabraja M, Klein M, Lehmann TN (2009) Long-term results following titanium cranioplasty of large skull defects. Neurosurg Focus 26(6):E10
Cheng YK, Weng HH, Yang JT, Lee MH, Wang TC, Chang CN (2008) Factors affecting graft infection after cranioplasty. J Clin Neurosci 15(10):1115–1119
Coulter IC, Pesic-Smith JD, Cato-Addison WB, Khan SA, Thompson D, Jenkins AJ, Strachan RD, Mukerji N (2014) Routine but risky: a multi-centre analysis of the outcomes of cranioplasty in the Northeast of England. Acta Neurochir (Wien) 156(7):1361–1368
Delgado-López PD, Martín-Velasco V, Castilla-Díez JM, Galacho-Harriero AM, Rodríguez-Salazar A (2009) Preservation of bone flap after craniotomy infection. Neurocirugia (Astur) 20(2):124–131
Dujovny M, Agner C, Aviles A (1999) Syndrome of the trephined: theory and facts. Crit Rev Neurosurg 9(5):271–278
Fodstad H, Love JA, Ekstedt J, Fridén H, Liliequist B (1984) Effect of cranioplasty on cerebrospinal fluid hydrodynamics in patients with the syndrome of the trephined. Acta Neurochir (Wien) 70(1–2):21–30
Gooch MR, Gin GE, Kenning TJ, German JW (2009) Complications of cranioplasty following decompressive craniectomy: analysis of 62 cases. Neurosurg Focus 26(6):E9
Grant GA, Jolley M, Ellenbogen RG, Roberts TS, Gruss JR, Loeser JD (2004) Failure of autologous bone-assisted cranioplasty following decompressive craniectomy in children and adolescents. J Neurosurg 100(2 Suppl Pediatrics):163–16
Hallfeldt KK, Stützle H, Puhlmann M, Kessler S, Schweiberer L (1995) Sterilization of partially demineralized bone matrix: the effects of different sterilization techniques on osteogenetic properties. J Surg Res 59(5):614–620
Hammon WM, Kempe LG (1971) Methyl methacrylate cranioplasty. 13 years experience with 417 patients. Acta Neurochir (Wien) 25(1):69–77
Hancock DO (1963) The fate of replaced bone flaps. J Neurosurg 20:983–984
Honeybul S (2010) Complications of decompressive craniectomy for head injury. J Clin Neurosci 17(4):430–435
Honeybul S, Janzen C, Kruger K, Ho KM (2013) The impact of cranioplasty on neurological function. Br J Neurosurg 27(5):636–641
Huang YH, Yang TM, Lee TC, Chen WF, Yang KY (2013) Acute autologous bone flap infection after cranioplasty for postinjury decompressive craniectomy. Injury 44(1):44–47
Inamasu J, Kuramae T, Nakatsukasa M (2010) Does difference in the storage method of bone flaps after decompressive craniectomy affect the incidence of surgical site infection after cranioplasty? comparison between subcutaneous pocket and cryopreservation. J Trauma 68(1):183–187
Iwama T, Yamada J, Imai S, Shinoda J, Funakoshi T, Sakai N (2003) The use of frozen autogenous bone flaps in delayed cranioplasty revisited. Neurosurgery 52(3):591–596
Jankowitz BT, Kondziolka DS (2006) When the bone flap hits the floor. Neurosurgery 59(3):585–590
Jho DH, Neckrysh S, Hardman J, Charbel FT, Amin-Hanjani S (2007) Ethylene oxide gas sterilization: a simple technique for storing explanted skull bone. technical note. J Neurosurg 107(2):440–445
Kim H, Sung SO, Kim SJ, Kim SR, Park IS, Jo KW (2013) Analysis of the factors affecting graft infection after cranioplasty. Acta Neurochir (Wien) 155(11):2171–2176
Lee CH, Chung YS, Lee SH, Yang HJ, Son YJ (2012) Analysis of the factors influencing bone graft infection after cranioplasty. J Trauma Acute Care Surg 73(1):255–260
Martin KD, Franz B, Kirsch M, Polanski W, von der Hagen M, Schackert G, Sobottka SB (2014) Autologous bone flap cranioplasty following decompressive craniectomy is combined with a high complication rate in pediatric traumatic brain injury patients. Acta Neurochir (Wien) 156(4):813–824
Matsuno A, Tanaka H, Iwamuro H, Takanashi S, Miyawaki S, Nakashima M, Nakaguchi H, Nagashima T (2006) Analyses of the factors influencing bone graft infection after delayed cranioplasty. Acta Neurochir (Wien) 148(5):535–540
Missori P, Polli FM, Rastelli E, Baiocchi P, Artizzu S, Rocchi G, Salvati M, Paolini S, Delfini R (2003) Ethylene oxide sterilization of autologous bone flaps following decompressive craniectomy. Acta Neurochir (Wien) 145(10):899–902
Mracek J, Choc M, Mork J, Vacek P, Mracek Z (2011) Osteoplastic decompressive craniotomy—an alternative to decompressive craniectomy. Acta Neurochir (Wien) 153(11):2259–2263
Nagayama K, Yoshikawa G, Somekawa K, Kohno M, Segawa H, Sano K, Shiokawa Y, Saito I (2002) Cranioplasty using the patient’s autogenous bone preserved by freezing–an examination of post-operative infection rates. No Shinkei Geka 30(2):165–169
Odom GL, Woodhall B, Wrenn FR (1952) The use of refrigerated autogenous bone flaps for cranioplasty. J Neurosurg 9(6):606–610
Osawa M, Hara H, Ichinose Y, Koyama T, Kobayashi S, Sugita Y (1990) Cranioplasty with a frozen and autoclaved bone flap. Acta Neurochir (Wien) 102(1–2):38–41
Piedra MP, Ragel BT, Dogan A, Coppa ND, Delashaw JB (2013) Timing of cranioplasty after decompressive craniectomy for ischemic or hemorrhagic stroke. J Neurosurg 118(1):109–114
Polin RS, Shaffrey ME, Bogaev CA, Tisdale N, Germanson T, Bocchicchio B, Jane JA (1997) Decompressive bifrontal craniectomy in the treatment of severe refractory posttraumatic cerebral edema. Neurosurgery 41(1):84–92
Prolo DJ, Burres KP, McLaughlin WT, Christensen AH (1997) Autogenous skull cranioplasty: fresh and preserved (frozen), with consideration of the cellular response. Neurosurgery 4(1):18–29
Rish BL, Dillon JD, Meirowsky AM, Caveness WF, Mohr JP, Kistler JP, Weiss GH (1997) Cranioplasty: a review of 1030 cases of penetrating head injury. Neurosurgery 4(5):381–385
Schuss P, Vatter H, Oszvald A, Marquardt G, Imöhl L, Seifert V, Güresir E (2013) Bone flap resorption: risk factors for the development of a long-term complication following cranioplasty after decompressive craniectomy. J Neurotrauma 30(2):91–95
Shimizu S, Morikawa A, Kuga Y, Mouri G, Murata T (2002) Cranioplasty using autogenous bone cryopreserved with dimethylsulfoxide (DMSO). No Shinkei Geka 30(5):479–485
Shah AM, Jung H, Skirboll S (2014) Materials used in cranioplasty: a history and analysis. Neurosurg Focus 36(4):E19
Sundseth J, Sundseth A, Berg-Johnsen J, Sorteberg W, Lindegaard KF (2014) Cranioplasty with autologous cryopreserved bone after decompressive craniectomy. complications and risk factors for developing surgical site infection. Acta Neurochir (Wien) 156(4):805–811
Tokoro K, Chiba Y, Tsubone K (1989) Late infection after cranioplasty—review of 14 cases. Neurol Med Chir (Tokyo) 29(3):196–201
Wachter D, Reineke K, Behm T, Rohde V (2013) Cranioplasty after decompressive hemicraniectomy: underestimated surgery-associated complications? Clin Neurol Neurosurg 115(8):1293–1297
Walcott BP, Kwon CS, Sheth SA, Fehnel CR, Koffie RM, Asaad WF, Nahed BV, Coumans JV (2013) Predictors of cranioplasty complications in stroke and trauma patients. J Neurosurg 118(4):757–762
Wester K (1994) Cranioplasty with an autoclaved bone flap, with special reference to tumour infiltration of the flap. Acta Neurochir (Wien) 131(3–4):223–225
Yadla S, Campbell PG, Chitale R, Maltenfort MG, Jabbour P, Sharan AD (2011) Effect of early surgery, material, and method of flap preservation on cranioplasty infections: a systematic review. Neurosurgery 68(4):1124–1129
Acknowledgements
Supported by MH CZ—DRO (Faculty Hospital in Pilsen—FNPl, 00669806)
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mracek, J., Hommerova, J., Mork, J. et al. Complications of cranioplasty using a bone flap sterilised by autoclaving following decompressive craniectomy. Acta Neurochir 157, 501–506 (2015). https://doi.org/10.1007/s00701-014-2333-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-014-2333-0