Abstract
Despite recent advances in perioperative management and surgical techniques, postoperative mortality and morbidity associated with bacteremia after orthotropic and living donor liver transplantation (OLT and LDLT) are still prevalent. Bacteremia is the most serious complication, and the most frequent cause of in-hospital death after OLT and LDLT [1, 2].
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Branched chain amino acids
- Orthotopic liver transplantation
- Living donor liver transplantation
- Bacteremia
- Oral supplementation
- Enteral nutrition
Abbreviations
- BCAA:
-
Branched chain amino acid
- OLT:
-
Orthotopic liver transplantation
- LDLT:
-
Living donor liver transplantation
- mTOR:
-
Mammalian target of rapamycin
Key Points
-
Posttransplant bacteremia is one of the most serious complications after liver transplantation.
-
Unfortunately, there are few therapies for preventing posttransplant bacteremia currently available.
-
For prevention of bacteremia, nutritional support is a promising strategy.
-
After orthotopic liver transplantation (OLT), serum levels of branched chain amino acids (BCAAs) generally decrease and severely decreased levels of BCAAs after OLT have been reported to be a risk factor for posttransplant bacteremia.
-
Pretransplant and/or posttransplant BCAA supplementation may be promising nutritional strategy in patients undergoing OLT and living donor liver transplantation (LDLT).
-
In this chapter, we review previous studies on the beneficial effects of BCAA supplementation in OLT and LDLT for preventing bacteremia and its mechanism of action, and provide a perspective on avenues for future research.
Introduction
Despite recent advances in perioperative management and surgical techniques, postoperative mortality and morbidity associated with bacteremia after orthotropic and living donor liver transplantation (OLT and LDLT) are still prevalent. Bacteremia is the most serious complication, and the most frequent cause of in-hospital death after OLT and LDLT [1, 2].
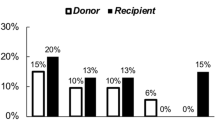
Risk factors for bacteremia after liver transplantation have been widely reported. For example, Singh et al. [1] reported that diabetes mellitus and serum albumin levels were independent predictors of bacteremia in patients undergoing orthotropic liver transplantation. Meanwhile, Iida et al. [2] reported that Child-Pugh class C, massive pleural effusion or ascites before the operation, ABO incompatibility, older donor age, and postoperative cytomegalovirus infections were independent risk factors in LDLT patients. Alexopoulos et al. [3] reported that the incidence of posttransplant bacteremia reached 42 % in patients achieving a model for end-stage liver disease score of ≥40. These data suggest that, in liver transplant recipients, deteriorated liver function before transplantation is related to postoperative bacteremia.
Nutritional support therapy after OLT and LDLT has been examined over the last 30 years (Table 15.1). The goal of nutritional support in most previous studies was prevention of posttransplant sepsis. After OLT, administration of 1.5–2.0 g of protein/kg body weight was reported to be necessary to achieve a positive nitrogen balance [4]. Reilly et al. [5] designed a randomized prospective study in which they randomly assigned 28 hypoalbuminemic cirrhotic patients to receive, immediately after liver transplantation, one of three regimens: group 1, no nutritional support (n = 10); group 2, total parenteral nutrition (TPN) (35 kcal/kg/day) with standard amino acids (1.5 g/kg/day) (n = 8); or group 3, isocaloric isonitrogenous TPN with added branched chain amino acids (BCAAs; n = 10). TPN with either standard or BCAA-enriched amino acids is tolerated well immediately after successful liver transplant. A positive nitrogen balance was achieved, and the large protein loads did not worsen encephalopathy. Nutritional support may improve respiratory muscle function, allowing earlier weaning from ventilatory support. A shortened ICU stay justifies the expense of TPN. Nevertheless, the number of patients in each group was too small to be evaluated, and while the authors showed the necessity of amino acids, they did not clearly show the beneficial effects of BCAAs over conventional amino acids.
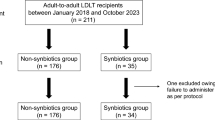
Our recent study [6] showed that the incidence of early graft loss was eightfold higher in recipients with massive intraoperative blood loss without early enteral nutrition, and that the main cause of early graft loss was bacteremia. An immune-modulating diet supplemented with arginine, glutamine, and omega-3 fatty acids was reported to have beneficial effects of enteral nutrition preventing bacteremia after LDLT [7]. Several previous prospective, randomized studies [8–10] have shown that perioperative synbiotic treatment prevents infectious complications in patients after elective OLT and LDLT. These studies confirmed the importance of nutritional support, especially enteral nutrition, for the prevention of bacteremia after liver transplantation. Nevertheless, the best nutritional substrate for preventing bacteremia remains unclear. Herein, we focus on the effects of BCAA supplementation in the light of prevention of posttransplant bacteremia.
Serum Levels of BCAA After Liver Transplant
Tietge et al. [11] investigated hepatic amino acid metabolism in patients with liver cirrhosis and over the long term after OLT. After OLT, BCAA levels remained subnormal, although higher than in cirrhosis. BCAA levels decreased with increasing catecholamine and insulin levels. These authors concluded that, despite normal liver function, BCAA levels remain subnormal after OLT. This decreased BCAA level after OLT was accompanied by normalization of aromatic amino acid levels, and this change in amino acid profile was observed in adults and children who had undergone OLT. The decreased serum BCAA levels might be explained by an increased requirement for BCAAs after OLT. Mager et al. [12] showed that the total BCAA requirement increased after OLT by measuring the oxidation of L-[1-13C] phenylalanine to 13CO2 after a primed, continuous infusion of the tracer. Furthermore, Luzi et al. [13] demonstrated that whole-body proteolysis, protein synthesis, and leucine oxidation were reduced in comparison to previously obtained values in a normal population. The rate of phenylalanine appearance across the forearm was equally suppressed in healthy adults and those who had undergone OLT, under condition of a euglycemic/insulin clamp. Conversely, whole-body leucine flux was not suppressed by insulin in adults after OLT, suggesting that the site of aberrant BCAA metabolism is insulin-sensitive tissues (liver or muscle). This may be partly due to insulin resistance and suppression of insulin secretion mediated by immunosuppressive therapy prescribed in the post-OLT period.
Previous studies have shown that decreased serum BCAA levels are related to posttransplant bacteremia. Munoz et al. [14] showed that a logistic regression model constructed using the BCAA/aromatic amino acid ratio predicted the occurrence of sepsis after OLT 77 % of the time. Figueiredo et al. [4] demonstrated that lower BCAA levels after liver transplantation were strongly associated with an increased likelihood of postoperative infections. Interestingly, Roth et al. [15] also showed decreased levels of BCAAs in orthotropic liver transplant patients suffering from sepsis. Taken together, these data suggested that BCAA supplementation after both OLT and LDLT may be useful for preventing bacteremia.
Effects of BCAA Supplementation for Prevention of Bacteremia
The effects of BCAA supplementation in patients who have undergone liver transplantation have been evaluated in only a few studies (Table 15.2). We previously found in Child-Pugh class C patients, no BCAA supplementation was a risk factor for bacteremia [16]. Kaido et al. demonstrated that low preoperative body cell mass and the absence of preoperative BCAA supplementation and hydrolyzed whey peptide, which is easily absorbed as BCAA, were significant risk factors for posttransplant bacteremia [17, 18].
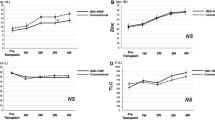
Yoshida et al. [19] designed a randomized prospective pilot study for evaluating the effect of posttransplant BCAA supplementation in patients who underwent LDLT. Although there were only 12 patients treated with BCAAs and 12 without BCAAs, synthesis of short-turnover protein, amino acid profile, and nonprotein respiratory quotient were significantly improved in the patients with BCAA supplementation. Although there was no significant difference in the incidence of sepsis between the two groups, a large-scale multicenter trial is necessary to determine the effect of BCAAs on prevention of bacteremia.
Mechanism Underlying the Beneficial Effects of BCAAs
Preoperative oral BCAA supplementation may reduce the incidence of posttransplant bacteremia in LDLT patients. The mechanism underlying this effect remains unclear. One possible mechanism is the improvement of nutritional status. Mattick et al. [20] showed that the changes following trauma and sepsis, termed systemic inflammatory response syndrome, elicit major changes in carbohydrate, protein, and energy metabolism. When these events persist for too long they result in a severe depletion of lean body mass, multiple organ dysfunction, and eventually death. Recently, various effects of BCAAs on liver, skeletal muscle, and the immune system have been examined (Table 15.3). The beneficial effects of BCAAs in critically ill patients can be understood more easily by considering the close relationship between muscle and liver, known as muscle-liver cross-talk. BCAAs are metabolized in two major steps that occur differentially in muscle and liver. In muscle, BCAAs are reversibly transaminated to the corresponding α-keto acids. For the complete degradation of BCAAs, the α-keto acids must travel to the liver to undergo oxidation. The liver, in contrast to muscle, does not significantly express branched chain aminotransferase. Thus, BCAA degradation is under the joint control of both liver and muscle. Recent evidence [21–23] suggests that in liver, BCAAs may perform signaling functions, more specifically activation of the mTOR (mammalian target of rapamycin) signaling pathway, influencing a wide variety of metabolic and synthetic functions, including protein translation, insulin signaling, and oxidative stress following severe injury and infection. In an in vitro study, BCAAs, especially leucine, activated the mTOR signaling pathway and inhibited protein degradation, resulting in the promotion of protein synthesis [21, 22]. Furthermore, in a cirrhotic rat model, leucine activated glycogen synthase via mTOR signaling and improved glucose metabolism [23]. Thus, BCAAs activate both PI3 kinase and mTOR pathways, and glucose uptake and glycogen synthesis are upregulated (Fig. 15.1). As mentioned previously, in a prospective study by Yoshida et al. [19], synthesis of short-turnover protein, amino acid profile, and nonprotein respiratory quotient were significantly improved after LDLT.
This metabolic improvement, such as the improvements in protein synthesis and glucose metabolism, may occur in immunocompetent cells. There have been several reports suggesting that BCAA supplementation can restore or regulate naturally acquired immunity. In previous cohort studies [24, 25], the BCAA supplementation groups showed elevated absolute lymphocyte counts. Bassit et al. [26] reported that BCAA supplementation restored the ability of peripheral blood mononuclear cells to proliferate in response to mitogens after long-distance intensive exercise. In a review article, Calder et al. [27] emphasized the necessity of BCAAs for lymphocytes to be able to synthesize protein, RNA, and DNA, and to divide in response to stimulation. Previous studies have shown that BCAAs increase the absolute lymphocyte number count [26, 28], and this may partly explain the reduced incidence of bacteremia in the BCAA group.
Nakamura et al. [29, 30] reported that, in patients with chronic liver disease, the phagocytic functions of neutrophils and the natural killer activity of lymphocytes obtained from patients with liver cirrhosis were restored by oral supplementation with BCAAs. Even in patients with advanced cirrhosis, Kakazu et al. [31, 32] reported that an elevation of the BCAA level improved the function of myeloid dendritic cells, and that this was beneficial to immune function. Our previous retrospective study [16] showed that, particularly in Child-Pugh class C patients who underwent LDLT, the lymphocyte ratio tended to be higher in the BCAA group than in the non-BCAA group. The beneficial effects of BCAA supplementation on posttransplant bacteremia may reflect the restoration of immune function.
Perspective on BCAA Therapy for the Prevention of Posttransplant Bacteremia with Special Reference to Skeletal Muscle Loss
Sarcopenia is primarily used to describe skeletal muscle loss that occurs during aging [33]. It can occur in patients with a variety of chronic illnesses, such as cancer, cardiovascular disease, bone fractures, and chronic liver disease. Among patients with liver cirrhosis, >40 % were reported to have accompanying sarcopenia [34] (Table 15.3). Although there are many causes of sarcopenia in cirrhotic patients, one of the most important causes is thought to be malnutrition (Table 15.4). Malnutrition has been reported in 60–80 % of patients with cirrhosis. However, identification of malnutrition is extremely difficult in such patients [35, 36]. Measurements of albumin and prealbumin levels do not necessarily reflect nutritional status, because hepatocellular protein synthesis is usually impaired in these patients. The assessment and interpretation of body weight is also difficult because of the presence of ascites, pleural effusion, and peripheral edema. The nonprotein respiratory quotient (npRQ) is a unitless number estimated from carbon dioxide production, and is used to evaluate the nutritional status of liver cirrhotic patients [36], although its measurement is sometimes difficult to perform in the clinical setting.
Thus, sarcopenia evaluated by computed tomography may be the most objective measurement of malnutrition of cirrhotic patients. Recently, evaluation of muscle loss in patients with liver cirrhosis was reported to be an important and a novel predictor of survival. Montano-Loza et al. [34] showed that sarcopenia was not correlated with the degree of liver dysfunction evaluated by a conventional scoring system. Thus, the extent of sarcopenia can be an independent marker of survival in patients with end-stage liver failure. Recently, Englesbe et al. [37] and Kaido et al. [38] reported that central sarcopenia strongly correlates with mortality after OLT. Sarcopenia in candidates for LT may be due to an extended catabolic phase and muscle breakdown in those with liver failure.
A number of complex metabolic alterations occur in liver disease that are unique to cirrhosis and affect skeletal muscle growth and atrophy responses. These include dysregulation of fatty acid oxidation and ketogenesis, gluconeogenesis from amino acids, glycogenolysis, and the use of BCAAs in skeletal muscle as a source of energy [21–23]. BCAAs also modulate signal transduction pathways as a messenger in skeletal muscle, preventing muscle atrophy. BCAAs, particularly leucine, have anabolic effects on protein metabolism by increasing the rate of protein synthesis and decreasing the rate of protein degradation in resting human muscle. These effects are likely to be mediated through changes in the signaling pathways controlling protein and glycogen synthesis. Therefore, BCAA deficiency can cause basic energy impairment in liver, skeletal muscle, and immune cells. On the other hand, as previously mentioned, decreased levels of BCAA were found in patients with septic OLT. Therefore, both sarcopenia and a high incidence of bacteremia may be due to low serum levels of BCAAs in posttransplant patients.
A more direct explanation of the relationship between sarcopenia and bacteremia could be provided by focusing on the profiles of other amino acids, such as glutamine. In plasma, the concentrations of threonine, glutamine, valine, cysteine, methionine, leucine, lysine, tryptophane, arginine, BCAAs, and the essential amino acids are correlated with age. These results indicate that there is an age dependency of the amino acid pattern in skeletal muscle and plasma. Stuerenburg et al. [39] showed that in myositis, which is a change seen in aged skeletal muscles, glutamate levels were significantly reduced. This study provides evidence that an alteration in glutamine levels is correlated with aging and might reflect increased proteolysis in aged and diseased human skeletal muscle. In chronic liver disease, skeletal muscle is able to seize ammonium during hyperammonemia, releasing glutamine [40]. In a recent experimental study, Jia et al. [41] administered carbon tetrachloride to rats repeatedly for 19 weeks as a decompensated cirrhosis model, and thereafter gave them a BCAA-enriched diet or normal diet for 5 weeks. Downregulation of fatty acid translocase/Cd36, glutamine synthetase, and pyruvate dehydrogenase kinase isoenzyme 4 is believed to promote lower uptake of fatty acids, lower ammonia incorporation, and higher uptake of glucose, and thus, to provide an energy source without using BCAAs. This study showed that, in patients with liver cirrhosis, serum BCAAs may be exhausted as a result of detoxication of ammonia in skeletal muscle. Glutamine would be produced in this process, and then disposed of via the liver.
Glutamine is the most abundant nonessential free amino acid in the healthy human body [40]. It is synthesized de novo, predominantly in skeletal muscle. Low glutamine levels, which have been detected in patients during critical illness, have been associated with poor outcomes [42]. Loss of muscle mass, with no evident upregulation of glutamine synthesis, has been inferred to contribute to insufficient glutamine production [43]. Thus, apparent glutamine deficiency, brought about by the increased glutamine requirements of immune cells, enterocytes, and hepatocytes, is thought to occur, and has led to the idea that glutamine is a “conditionally essential” amino acid in critically ill patients. It is widely accepted that immune system responses such as T-cell proliferation, B cell differentiation, macrophage phagocytosis, antigen presentation, cytokine production, and enterocyte barrier function target intestinal bacteria.
Under a stress condition, such as postliver transplantation and liver function deterioration, glutamine exhaustion may easily occur without BCAA supplementation. In these patients with glutamine exhaustion, bacteremia may occur owing to bacterial translocation from gut and/or impaired immunity (Fig. 15.2). Thus, especially in sarcopenic patients who have undergone liver transplantation, and who are supposed to have impaired glutamine production activity in their skeletal muscle, BCAA supplementation may be beneficial for maintaining glutamine metabolism.
Hypothesis for the development of posttransplant bacteremia in light of muscle-liver cross-talk. Decreased BCAA levels can cause glutamine deficiency and this may be a cause of enterocyte and immune system dysfunction. Alternative explanations of posttransplant bacteremia are possible, especially in patients with sarcopenia
By analyzing body composition, especially in the light of sarcopenia, custom-made nutritional support such as BCAA supplementation should be examined, and may be realized in the very near future.
Conclusions
Recently, the various effects of BCAAs on liver, skeletal muscle, and host immunity have been examined and demonstrated in patients with end-stage liver disease [44]. BCAA supplementation preliver and post-liver transplantation may provide essential nutritional support for preventing posttransplant bacteremia. This nutritional support may improve protein synthesis and naturally acquired immunity. Furthermore, in patients with sarcopenia, which is a commonly observed condition in candidates for liver transplantation, BCAA supplementation may improve the outcome after liver transplantation. Further large-scale clinical trials are necessary to test this hypothesis.
References
Singh N, Paterson DL, Gayowski T, Wagener MM, Marino IR. Predicting bacteremia and bacteremic mortality in liver transplant recipients. Liver Transpl. 2000;6:54–61.
Iida T, Kaido T, Yagi S, et al. Posttransplant bacteremia in adult living donor liver transplant recipients. Liver Transpl. 2010;16:1379–85.
Alexopoulos S, Matsuoka L, Cho Y, et al. Outcomes after liver transplantation in patients achieving a model for end-stage liver disease score of 40 or higher. Transplantation. 2013;95:507–12.
Figueiredo F, Dickson ER, Pasha T, et al. Impact of nutritional status on outcomes after liver transplantation. Transplantation. 2000;70:1347–52.
Reilly J, Mehta R, Teperman L, et al. Nutritional support after liver transplantation: a randomized prospective study. J Parenter Enteral Nutr. 1990;14:386–91.
Ikegami T, Shirabe K, Yoshiya S, et al. Bacterial sepsis after living donor liver transplantation: the impact of early enteral nutrition. J Am Coll Surg. 2012;214:288–95.
Kaido T, Mori A, Ogura Y, et al. Impact of enteral nutrition using a new immuno-modulating diet after liver transplantation. Hepatogastroenterology. 2010;57:1522–5.
Rayes N, Seehofer D, Hansen S, et al. Early enteral supply of lactobacillus and fiber versus selective bowel decontamination: a controlled trial in liver transplant recipients. Transplantation. 2002;74:123–7.
Rayes N, Seehofer D, Theruvath T, et al. Supply of pre- and probiotics reduces bacterial infection rates after liver transplantation – a randomized, double-blind trial. Am J Transplant. 2005;5(1):125–30.
Eguchi S, Takatsuki M, Hidaka M, et al. Perioperative synbiotic treatment to prevent infectious complications in patients after elective living donor liver transplantation: a prospective randomized study. Am J Surg. 2011;201:498–502.
Tietge UJ, Bahr MJ, Manns MP, Böker KH. Hepatic amino-acid metabolism in liver cirrhosis and in the long-term course after liver transplantation. Transpl Int. 2003;16:1–8.
Mager DR, Wykes LJ, Roberts EA, Ball RO, Pencharz PB. Effect of orthotopic liver transplantation (OLT) on branched-chain amino acid requirement. Pediatr Res. 2006;59:829–34.
Luzi L, Regalia E, Pulvirenti A, et al. Post-absorptive and insulin-mediated muscle protein metabolism in liver-transplanted patients. Acta Diabetol. 2002;39:203–8.
Munoz SJ, Jarrell BE, Westerberg S, Miller L, Moritz MJ, Maddrey WC. Serum amino acids following human orthotopic liver transplantation. Transplant Proc. 1993;25:1779–82.
Roth E, Muhlbacher F, Karner J, Steininger R, Schemper M, Funovics J. Liver amino acids in sepsis. Surgery. 1985;97:436–42.
Shirabe K, Yoshimatsu M, Motomura T, et al. Beneficial effects of supplementation with branched-chain amino acids on postoperative bacteremia in living donor liver transplant recipients. Liver Transpl. 2011;17:1073–80.
Kaido T, Mori A, Ogura Y, et al. Pre- and perioperative factors affecting infection after living donor liver transplantation. Nutrition. 2012;28:1104–8.
Kaido T, Ogura Y, Ogawa K, et al. Effects of post-transplant enteral nutrition with an immunomodulating diet containing hydrolyzed whey peptide after liver transplantation. World J Surg. 2012;36:1666–71.
Yoshida R, Yagi T, Sadamori H, et al. Branched-chain amino acid-enriched nutrients improve nutritional and metabolic abnormalities in the early post-transplant period after living donor liver transplantation. J Hepatobiliary Pancreat Sci. 2012;19:438–48.
Mattick JS, Kamisoglu K, Ierapetritou MG, Androulakis IP, Berthiaume F. Branched-chain amino acid supplementation: impact on signaling and relevance to critical illness. Wiley Interdiscip Rev Syst Biol Med. 2013;5(4):449–60.
Ijichi C, Matsumura T, Tsuji T, Eto Y. Branched-chain amino acids promote albumin synthesis in rat primary hepatocytes through the mTOR signal transduction system. Biochem Biophys Res Commun. 2003;303:59–64.
Matsumura T, Morinaga Y, Fujitani S, Takehana K, Nishitani S, Sonaka I. Oral administration of branched-chain amino acids activates the mTOR signal in cirrhotic rat liver. Hepatol Res. 2005;33:27–32.
Nishitani S, Ijichi C, Takehana K, Fujitani S, Sonaka I. Pharmacological activities of branched-chain amino acids: specificity of tissue and signal transduction. Biochem Biophys Res Commun. 2004;313:387–9.
Cerra FB, Mazuski JE, Chute E, et al. Branched chain metabolic support. A prospective, randomized, double-blind trial in surgical stress. Ann Surg. 1984;199:286–91.
Vente JP, Soeters PB, von Meyenfeldt MF, et al. Prospective randomized double-blind trial of branched chain amino acid enriched versus standard parenteral nutrition solutions in traumatized and septic patients. World J Surg. 1991;15:128–32.
Bassit RA, Sawada LA, Bacurau RF, et al. Branched-chain amino acid supplementation and the immune response of long-distance athletes. Nutrition. 2002;18:376–9.
Calder PC. Branched-chain amino acids and immunity. J Nutr. 2006;136:288S–93.
Chuang JC, Yu CL, Wang SR. Modulation of human lymphocyte proliferation by amino acids. Clin Exp Immunol. 1990;81:173–6.
Nakamura I, Ochiai K, Imawari M. Phagocytic function of neutrophils of patients with decompensated liver cirrhosis is restored by oral supplementation of branched-chain amino acids. Hepatol Res. 2004;29:207–11.
Nakamura I, Ochiai K, Imai Y, Moriyasu F, Imawari M. Restoration of innate host defense responses by oral supplementation of branched-chain amino acids in decompensated cirrhotic patients. Hepatol Res. 2007;37:1062–7.
Kakazu E, Kanno N, Ueno Y, Shimosegawa T. Extracellular branched-chain amino acids, especially valine, regulate maturation and function of monocyte-derived dendritic cells. J Immunol. 2007;179:7137–46.
Kakazu E, Ueno Y, Kondo Y, et al. Branched chain amino acids enhance the maturation and function of myeloid dendritic cells ex vivo in patients with advanced cirrhosis. Hepatology. 2009;50:1936–45.
Doherty TJ. Invited review: aging and sarcopenia. J Appl Physiol. 2003;95:1717–27.
Montano-Loza AJ, Meza-Junco J, Prado CM, et al. Muscle wasting is associated with mortality in patients with cirrhosis. Clin Gastroenterol Hepatol. 2012;10:166–73.
Piquet MA, Ollivier I, Gloro R, Castel H, Tiengou LE, Dao T. Nutritional indices in cirrhotic patients. Nutrition. 2006;22:216–7.
Tsuchiya M, Sakaida I, Okamoto M, Okita K. The effect of a late evening snack in patients with liver cirrhosis. Hepatol Res. 2005;31:95–103.
Englesbe MJ, Patel SP, He K, et al. Sarcopenia and mortality after liver transplantation. J Am Coll Surg. 2010;211:271–8.
Stuerenburg HJ, Stangneth B, Schoser BG. Age related profiles of free amino acids in human skeletal muscle. Neuro Endocrinol Lett. 2006;27:133–6.
Kaido T, Ogawa K, Fujimoto Y. Impact of sarcopenia on survival in patients undergoing living donor liver transplantation. Am J Transplant. 2013. doi:10.1111/ajt.12221.
Adeva MM, Souto G, Blanco N, Donapetry C. Ammonium metabolism in humans. Metabolism. 2012;61:1495–511.
Jia H, Takahashi S, Saito K, Kato H. DNA microarray analysis identified molecular pathways mediating the effects of supplementation of branched-chain amino acids on CCl4-induced cirrhosis in rats. Mol Nutr Food Res. 2013;57:291–306.
Karinch AM, Pan M, Lin CM, Strange R, Souba WW. Glutamine metabolism in sepsis and infection. J Nutr. 2001;131 Suppl 9:2535S–8. discussion 2550S–1S.
Biolo G, Zorat F, Antonione R, Ciocchi B. Muscle glutamine depletion in the intensive care unit. Int J Biochem Cell Biol. 2005;37:2169–79.
Masuda T, Shirabe K, Yoshiya S, et al. Nutrition support and infections associated with hepatic resection and liver transplantation in patients with chronic liver disease. J Parenter Enteral Nutr. 2013;37:318–26.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer Science+Business Media New York
About this chapter
Cite this chapter
Shirabe, K., Ikegami, T., Yoshizumi, T., Maehara, Y. (2015). Basic Aspects in Prevention of Posttransplant Bacteremia by Branched Chain Amino Acids. In: Rajendram, R., Preedy, V., Patel, V. (eds) Branched Chain Amino Acids in Clinical Nutrition. Nutrition and Health. Humana Press, New York, NY. https://doi.org/10.1007/978-1-4939-1914-7_15
Download citation
DOI: https://doi.org/10.1007/978-1-4939-1914-7_15
Published:
Publisher Name: Humana Press, New York, NY
Print ISBN: 978-1-4939-1913-0
Online ISBN: 978-1-4939-1914-7
eBook Packages: MedicineMedicine (R0)