Abstract
Purpose
Cancer cachexia leads to poor outcomes, especially for patients with advanced stage disease. The cachexia index (CXI), a novel biomarker for cancer cachexia, has been identified as a prognostic indicator for several malignancies. The present study aimed to clarify the prognostic significance of the CXI for patients with recurrent pancreatic cancer.
Methods
This retrospective study enrolled 113 patients diagnosed with recurrence following pancreatectomy for pancreatic cancer, to analyze the association between the CXI and prognostic survival.
Results
The 2-year overall survival rate and median survival of all patients were 28.5% and 12.6 months, respectively. The 2-year overall survival curve in the high CXI group was significantly better than that in the low CXI group (p < 0.001). The rate of chemotherapy after recurrence was significantly lower in the low CXI group than in the high CXI group (p = 0.002). Multivariate analysis identified the CXI as an independent prognostic factor for patients with recurrent pancreatic cancer (p = 0.011).
Conclusions
The CXI proved useful for predicting the post-recurrence prognosis of patients with recurrent pancreatic cancer. Patients with a low CXI at the time of recurrence have poorer prognostic outcomes than those with a high CXI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
According to the latest report on cancer statistics, pancreatic cancer is the third-leading cause of cancer death, it has a 5-year relative survival rate of 12%, and it remains one of the most challenging malignancies to treat [1]. In Japan, the number of registered patients with newly developed pancreatic cancer is increasing every year [2]. The dismal prognosis of pancreatic cancer arises from its frequent postoperative recurrence, even when surgical resection with curative intent has been achieved. Despite the various therapeutic strategies developed for patients with recurrent pancreatic cancer, the median survival time (MST) after recurrence remains unsatisfactory at 3.0–19.0 months [3,4,5]. Therefore, it is crucial to identify accurate predictive factors for the prognosis of patients with recurrent pancreatic cancer to optimize quality of life in their remaining lifetime.
The prognosis of cancer patients is multifactorial and influenced by both tumor-related factors and individual patient characteristics. Cancer cachexia is a multifactorial syndrome characterized by ongoing loss of skeletal muscle mass, with or without loss of fat mass that cannot be fully reversed by conventional nutritional support and leads to progressive functional impairment [6]. Cachexia causes poor performance status (PS), resulting in high mortality for approximately 50% of cancer patients, and accounting for approximately 20% of cancer deaths [7]. The cachexia index (CXI), comprising the skeletal muscle index (SMI), serum albumin level, and neutrophil-to-lymphocyte ratio (NLR), is a novel biomarker that was established to comprehensively reflect the cachectic status [8]. The relationship between the CXI and the prognostic outcomes of cancer patients has been investigated, and a low CXI was found to independently reflect a poor prognosis in several malignancies [9,10,11,12]. However, no studies have examined the prognostic significance of the CXI in patients with recurrence after pancreatic cancer surgery.
Against this background, the present study was conducted to evaluate the utility of the CXI to predict prognosis after recurrence for patients with pancreatic cancer.
Methods
Patients
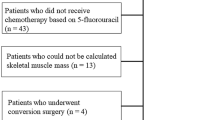
We reviewed the medical records of 181 patients with histologically confirmed pancreatic ductal adenocarcinoma, who underwent pancreatectomy at our institution between July, 2005 and December, 2022. As of April, 2023, 116 (64.1%) had postoperative recurrence. After the exclusion of three patients because of insufficient available data, 113 patients with recurrent pancreatic cancer were enrolled in this retrospective analysis. All patients in the study were of Japanese ethnicity. The study was approved by the Tottori University Hospital Ethics Committee (no. 21A125) and the requirement for informed consent was waived.
Postoperative recurrence after pancreatectomy was detected by periodic radiological examinations, such as computed tomography or magnetic resonance imaging, and if necessary, by positron emission tomography, and measurement of serum carbohydrate antigen 19–9 (CA19-9) levels. The following clinical characteristics at the time of recurrence were obtained from the patients’ medical records: age, sex, body mass index (BMI), Eastern Cooperative Oncology Group (ECOG) PS, initial site of recurrence, serum albumin level, NLR, CA19-9 level, and SMI. The following data were also collected: time to recurrence after pancreatectomy, chemotherapy after recurrence, and pathological data for the primary tumor, including localization, tumor size, lymph node involvement, blood vessel invasion, perineural invasion, and histological grade based on the Tumor-Node-Metastasis classification of the International Union Against Cancer (8th edition). The time to recurrence was divided into early recurrence, defined as recurrence identified within 12 months after the initial surgery; and late recurrence, defined as recurrence identified beyond 12 months after the initial surgery.
Cachexia index
The CXI was calculated using the following formula: CXI = SMI × serum albumin level (g/dL)/NLR [8]. The SMI was calculated by normalizing the cross-sectional areas of skeletal muscle mass at the level of the third lumbar vertebra to the patient height (cm2/m2). The cross-sectional areas of total skeletal muscle mass at the level of the third lumbar vertebra on computed tomography images at the time of recurrence were automatically measured by a SYNAPSE VINCENT (Fujifilm, Tokyo, Japan) for the study. The NLR, defined as the peripheral neutrophil count divided by the peripheral lymphocyte count, was obtained from laboratory data at the time of recurrence.
Statistical analysis
Differences between two groups were analyzed using the Chi-square or Fisher’s exact probability tests for categorical variables and the Mann–Whitney U test for continuous variables with a nonparametric distribution. Receiver operating characteristic (ROC) analysis was performed to calculate the cutoff value of CA19-9 and CXI. The 2-year post-recurrence survival curves were constructed by the Kaplan–Meier method and the differences between survival curves were estimated using the log-rank test. Cox proportional hazards models with a stepwise procedure were used to conduct univariate and multivariate analyses to identify prognostic factors for 2-year post-recurrence survival. Values of p < 0.05 were considered significant. All statistical analyses were performed using IBM SPSS Statistics for Windows (version 25; IBM, Armonk, NY, USA).
Results
The 2-year post-recurrence overall survival (OS) rate and MST of all the patients with recurrent pancreatic cancer were 28.5% and 12.6 months, respectively (Fig. 1). The median CXI values before surgery and at the time of recurrence were 79.5 for men and 68.9 for women, and 77.0 for men and 71.6 for women, respectively. The CXI at the time of recurrence was almost as same as the preoperative CXI. The cutoff values for the CXI at the time of recurrence in this study were set by ROC analysis at 51.2 for men and 69.5 for women. Based on these CXI cutoff values, the patients with recurrent pancreatic cancer were divided into a high CXI group (n = 73) and a low CXI group (n = 40).
Table 1 summarizes the clinicopathological characteristics of the two groups. The median (range) CXI was 122.8 in the high CXI group and 43.2 in the low CXI group, and this difference was significant. There were no significant differences in age, sex, primary tumor size, blood vessel invasion, perineural invasion, histological grade of the primary tumor, and site of recurrence between the two groups. BMI, the rate of chemotherapy after recurrence and preoperative CXI were significantly lower in the low CXI group than in the high CXI group. The rates of ECOG PS 1 or 2, the CA19-9 level at the time of recurrence, and lymph node involvement were significantly higher in the low CXI group than in the high CXI group. At the time of recurrence, the albumin level and SMI were significantly lower and the NLR was significantly higher in the low CXI group than in the high CXI group. The incidence of early recurrence was higher in the low CXI group than in the high CXI group. The 2-year post-recurrence OS rate and MST were 36.5% and 15.6 months in the high CXI group versus 13.2% and 6.4 months in the low CXI group, respectively. The 2-year post-recurrence OS curve of the high CXI group was significantly better than that of the low CXI group (p < 0.001; Fig. 2).
Among the total 113 patients enrolled in the study, 89 (78.8%) received systemic chemotherapy after recurrence. As first-line chemotherapy, 52 patients received gemcitabine-based combination regimens (30 gemcitabine plus nab-paclitaxel; 22 gemcitabine plus S-1), 8 received modified FOLFIRINOX, 1 received nanoliposomal irinotecan plus 5-fluorouracil/leucovorin, 15 received gemcitabine alone, 12 received S-1 alone, and 1 received uracil-tegafur. Second-line chemotherapy was given to 35 (39.3%) of the 89 patients with disease progression after the first-line chemotherapy. The remaining patients received best supportive care. Table 2 summarizes the systemic chemotherapy regimens following recurrence. No significant difference in first-line chemotherapy was observed between the high- and low-CXI groups; however, second-line chemotherapy was administered significantly more often in the high-CXI group than in the low-CXI group. In contrast, there were more patients without post-recurrent chemotherapy in the low-CXI group than in the high-CXI group. Figure 3 shows the 2-year post-recurrence OS survival curves stratified by chemotherapy in both the high-CXI group and the low-CXI group. The survival curves of patients who did not receive chemotherapy or received first-line chemotherapy were significantly better in the high-CXI group than in the low-CXI group (Fig. 3a, b). However, the survival curves of patients who received second-line chemotherapy in the two groups were similar, with no significant difference (Fig. 3c).
Multivariate analysis identified a low CXI at the time of recurrence as an independent predictive factor for poor prognosis (p = 0.018), along with lymph node metastasis at the initial surgery (p = 0.036), high CA19-9 levels at the time of recurrence (p < 0.001), early recurrence within 12 months (p = 0.009), and management without chemotherapy after recurrence (p = 0.001) (Table 3).
Discussion
The present study demonstrated that a low CXI is closely associated with poor survival after postoperative recurrence for patients with pancreatic cancer, and that it is also an independent prognostic risk factor for patients with recurrent pancreatic cancer. This is the first study to suggest the importance of assessing cancer cachexia at the time of recurrence in patients with pancreatic cancer. Cancer cachexia is considered to have a complex multifactorial pathogenesis caused by the interactions between the tumor and various host factors, and remains a challenging condition affecting cancer patients at advanced stages [6, 13]. The complex interactions between the tumor and host factors in advanced cancer patients are related mainly to systemic inflammation, which decreases oral intake and causes a wasting syndrome characterized by muscle loss, poor PS, and reduced tolerability of cancer treatment [14]. Therefore, systemic inflammation, malnutrition, and loss of skeletal muscle volume, as the clinical features of cancer cachexia, are observed in patients with various advanced cancers. The CXI, devised by Jafri et al. [8], consists of the SMI, serum albumin level, and NLR, and this new biomarker enables the comprehensive evaluation of sarcopenia, systemic inflammation, and nutritional status. These three clinical parameters are key components of cancer cachexia and each is closely associated with a poor prognosis independently in patients with various cancers, including pancreatic cancer [15,16,17,18]. Therefore, the CXI, comprising the SMI, serum albumin level, and NLR, is considered a reliable biomarker that can precisely evaluate the status of cancer cachexia and the prognosis of advanced cancer patients.
Cachexia has been reported to develop in 80–90% of patients with advanced stage pancreatic cancer, with massive loss of skeletal muscle mass, a low serum albumin level, and high NLR [19, 20]. In fact, the CXI was identified as a useful prognostic indicator after resection in patients with resectable pancreatic cancer. The high incidence of cachexia in these patients can be explained by the highly malignant behavior of pancreatic cancer. Because cancer recurrence after surgery generally indicates systemic tumor spread, it is recognized as an incurable pathogenesis. Moreover, the pathogenesis differs between resectable pancreatic cancer with the potential for curability and recurrent pancreatic cancer without the potential for curability. In fact, the median post-recurrence survival of patients with recurrent pancreatic cancer is markedly curtailed to approximately 1.5 years or less, even if the patients receive chemotherapy, other than a favorable survival outcome reported for patients with isolated pulmonary metastases [5, 21, 22]. CA19-9 is the most frequently used tumor marker in pancreatic cancer, and high levels of CA19-9 are well-known to be an independent prognostic risk factor. This study demonstrated that patients with a low CXI had significantly higher CA19-9 levels than those with a high CXI, which explained why the CXI was closely associated with the prognostic outcome of patients with pancreatic cancer, because CA19-9 is derived mainly from the cancer itself. The present findings confirmed our hypothesis that evaluation of the CXI at the time of recurrence is important for accurate prediction of the prognosis and for deciding on optimal treatments such as chemotherapy or supportive and palliative care to optimize quality of life for patients with recurrent pancreatic cancer whose prognosis is very poor.
The present study demonstrated that pancreatic cancer patients with a low CXI at the time of recurrence had a significantly worse prognosis than those with a high CXI at the time of recurrence. Although systemic chemotherapy can prolong the life of patients with advanced or recurrent cancer, the proportion of patients administered chemotherapy was significantly lower in the low CXI group than in the high CXI group. Cancer cachexia influences the tolerability of chemotherapy [23]. In previous studies, patients with a low CXI were less likely to receive chemotherapy for various cancers [8, 24, 25]. Both the SMI and albumin are recognized as nutritional biomarkers, which are components of the CXI, and are well-known to be correlated with tolerability of chemotherapy. Because patients with a low CXI have a poor nutritional status, they need more frequent dose reductions and a lower relative dose intensity of the drug. Therefore, a low CXI can not only reflect cancer cachexia accurately, but it can also indicate decreased tolerability of chemotherapy, and is associated with the dismal prognosis of patients with recurrent pancreatic cancer. Taken together, the findings confirmed our hypothesis that the CXI is a reliable biomarker, which can accurately predict the prognosis of patients with recurrent pancreatic cancer and severe cancer cachexia.
The present study has several limitations. First, it was a retrospective study conducted in a single institution, with a limited population of only Japanese individuals. These factors may limit the generalizability of the findings. Second, although the cutoff value of the CXI in this study was set by the ROC analysis, whether this cutoff value for the CXI is adequate to predict the post-recurrence prognosis of patients with recurrent pancreatic cancer remains unclear. Third, no unified systemic chemotherapy regimen was administered as first-line chemotherapy for the patients in the study, which may have led to bias. Therefore, a well-designed, large-scale, randomized controlled study is needed to verify the impact of the CXI as a predictive factor for the prognosis of patients with recurrent pancreatic cancer.
In conclusion, the CXI is useful for predicting the post-recurrence prognosis of patients with recurrent pancreatic cancer. Patients with a low CXI at the time of recurrence have a poorer prognosis than patients with a high CXI at the time of recurrence. Identifying the CXI at the time of recurrence may help with decision-making for treatment to optimize the quality of life of patients with recurrent pancreatic cancer. Furthermore, nutritional therapy and an exercise program as soon as possible after curative surgery may improve the prognosis of patients with recurrent pancreatic cancer.
References
Siegel RL, Miller KD, Wagle NS, Jemal A. Cancer statistics, 2023. CA Cancer J Clin. 2023;73:17–48.
Awaya A, Kuroiwa Y. The relationship between annual airborne pollen levels and occurrence of all cancers, and lung, stomach, colorectal, pancreatic and breast cancers: a retrospective study from the national registry database of cancer incidence in Japan, 1975–2015. Int J Environ Res Public Health. 2020;2020:17.
Sperti C, Pasquali C, Piccoli A, Pedrazzoli S. Recurrence after resection for ductal adenocarcinoma of the pancreas. World J Surg. 1997;21:195–200.
Van den Broeck A, Sergeant G, Ectors N, Van Steenbergen W, Aerts R, Topal B. Patterns of recurrence after curative resection of pancreatic ductal adenocarcinoma. Eur J Surg Oncol. 2009;35:600–4.
Kolbeinsson H, Hoppe A, Bayat A, Kogelschatz B, Mbanugo C, Chung M, et al. Recurrence patterns and postrecurrence survival after curative intent resection for pancreatic ductal adenocarcinoma. Surgery. 2021;169:649–54.
Fearon K, Strasser F, Anker SD, Bosaeus I, Bruera E, Fainsinger RL, et al. Definition and classification of cancer cachexia: an international consensus. Lancet Oncol. 2011;12:489–95.
Tisdale MJ. Cachexia in cancer patients. Nat Rev Cancer. 2002;2:862–71.
Jafri SH, Previgliano C, Khandelwal K, Shi R. Cachexia index in advanced non-small-cell lung cancer patients. Clin Med Insights Oncol. 2015;9:87–93.
Hamura R, Haruki K, Shirai Y, Tanji Y, Taniai T, Okui N, et al. Preoperative cachexia index can predict the prognosis of extrahepatic biliary tract cancer after resection. Surg Oncol. 2022;44:101825.
Kamada T, Haruki K, Nakashima K, Takahashi J, Nakaseko Y, Suzuki N, et al. Prognostic significance of the cachexia index in patients with stage I-III colorectal cancer who underwent laparoscopic surgery. Surg Today. 2023;53:1064–72.
Nakashima K, Haruki K, Kamada T, Takahashi J, Nakaseko Y, Ohdaira H, et al. Usefulness of the cachexia index as a prognostic indicator for patients with gastric cancer. Ann Gastroenterol Surg. 2023;7:733–40.
Shimagaki T, Sugimachi K, Mano Y, Onishi E, Iguchi T, Nakashima Y, et al. Cachexia index as a prognostic predictor after resection of pancreatic ductal adenocarcinoma. Ann Gastroenterol Surg. 2023;7:977–86.
Setiawan T, Sari IN, Wijaya YT, Julianto NM, Muhammad JA, Lee H, et al. Cancer cachexia: molecular mechanisms and treatment strategies. J Hematol Oncol. 2023;16:54.
Suzuki H, Asakawa A, Amitani H, Nakamura N, Inui A. Cancer cachexia–pathophysiology and management. J Gastroenterol. 2013;48:574–94.
Stotz M, Gerger A, Eisner F, Szkandera J, Loibner H, Ress AL, et al. Increased neutrophil-lymphocyte ratio is a poor prognostic factor in patients with primary operable and inoperable pancreatic cancer. Br J Cancer. 2013;109:416–21.
Ninomiya G, Fujii T, Yamada S, Yabusaki N, Suzuki K, Iwata N, et al. Clinical impact of sarcopenia on prognosis in pancreatic ductal adenocarcinoma: A retrospective cohort study. Int J Surg. 2017;39:45–51.
Nakano Y, Kitago M, Shinoda M, Yagi H, Abe Y, Takano K, et al. Prognostic significance of the postoperative level and recovery rate of serum albumin in patients with curatively resected pancreatic ductal adenocarcinoma. Mol Clin Oncol. 2019;11:270–8.
Blomstrand H, Green H, Fredrikson M, Gränsmark E, Björnsson B, Elander NO. Clinical characteristics and blood/serum bound prognostic biomarkers in advanced pancreatic cancer treated with gemcitabine and nab-paclitaxel. BMC Cancer. 2020;20:950.
Poulia KA, Sarantis P, Antoniadou D, Koustas E, Papadimitropoulou A, Papavassiliou AG, et al. Pancreatic cancer and cachexia-metabolic mechanisms and novel insights. Nutrients. 2020;2020:12.
Vasconcelos De Matos L, Coelho A, Cunha R, Fernandes L, Fontes ESM, Neves MT, et al. Association of weight change inflammation markers and disease staging with survival of patients undergoing chemotherapy for pancreatic adenocarcinoma. Nutr Cancer. 2022;74:546–54.
Konishi T, Takano S, Takayashiki T, Kuboki S, Suzuki D, Sakai N, et al. Clinical benefits of pulmonary resection for lung metastases from pancreatic cancer. Langenbecks Arch Surg. 2023;409:11.
Stuart CM, Kirsch MJ, Zhuang Y, Meguid CL, Sugawara T, Colborn KL, et al. Pulmonary metastasectomy is associated with survival after lung-only recurrence in pancreatic cancer. Surgery. 2023;174:654–9.
Mitsunaga S, Kasamatsu E, Machii K. Incidence and frequency of cancer cachexia during chemotherapy for advanced pancreatic ductal adenocarcinoma. Support Care Cancer. 2020;28:5271–9.
Go SI, Park MJ, Park S, Kang MH, Kim HG, Kang JH, et al. Cachexia index as a potential biomarker for cancer cachexia and a prognostic indicator in diffuse large B-cell lymphoma. J Cachexia Sarcopenia Muscle. 2021;12:2211–9.
Goh MJ, Kang W, Jeong WK, Sinn DH, Gwak GY, Paik YH, et al. Prognostic significance of cachexia index in patients with advanced hepatocellular carcinoma treated with systemic chemotherapy. Sci Rep. 2022;12:7647.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
Study conception and design: TS; data acquisition: MK and YM; data analysis and interpretation: KM, TH, YS, and TM; statistical analysis: TS, KK, and MY; manuscript preparation: TS; manuscript editing: NT; manuscript review: YF; final approval of the article: all authors.
Corresponding author
Ethics declarations
Conflict of interests
We have no competing interests to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sakamoto, T., Kishino, M., Murakami, Y. et al. The cachexia index is a prognostic factor for patients with recurrent pancreatic cancer. Surg Today (2024). https://doi.org/10.1007/s00595-024-02877-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00595-024-02877-z