Abstract
Purpose
An accurate diagnosis of thymic malignancies is important, but challenging due to the broad range of differential diagnoses. This study aims to evaluate the efficacy of PET/CT and tumor markers for diagnosing thymic malignancies.
Methods
Patients admitted to our department between January 2012 and December 2021 with primary anterior mediastinal tumors were retrospectively evaluated. We evaluated the relationship between the maximum standardized uptake value (SUVmax), tumor markers, and pathological diagnosis in four groups: thymic carcinoma, thymoma, lymphoma, and others.
Results
In total, 139 patients were included in this study. The SUVmax was significantly higher in lymphoma, thymic carcinoma, and thymoma, in that order. The cytokeratin 19 fragment (CYFRA 21-1) was significantly higher in thymic carcinoma than in the other groups. An ROC curve analysis indicated that the optimal cut-off values of SUVmax for thymic carcinoma plus lymphoma and CYFRA 21-1 for thymic carcinoma were 7.97 (AUC = 0.934) and 2.95 (AUC = 0.768), respectively. Using a combination of cut-off values (SUVmax = 8, CYFRA 21-1 = 3), the accuracy rate for diagnosing thymic carcinoma was 91.4%.
Conclusions
The SUVmax and CYFRA 21-1 levels are significant indicators for the diagnosis of thymic carcinoma. Combining these indicators resulted in a more accurate diagnosis of thymic malignancies, which could facilitate the decision-making process for determining the optimal treatment strategies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
An accurate diagnosis of anterior mediastinal tumors plays an important role in determining the treatment strategy; however, the broad differential diagnosis makes this challenging. The most common histological type is thymic epithelial tumor (accounting for 35%), followed by malignant lymphoma (approximately 25%) [1]. There are other histological types such as germ cell tumors, neuroendocrine tumors (NET), cystic lesions, and other atypical lesions, in addition to major tumors. For resectable lesions, the treatment strategy (i.e., initial surgery or preoperative biopsy) was determined based on the findings of a differential diagnosis.
Thymic epithelial tumors include thymomas, thymic carcinomas, and NET [2, 3]. The standard procedure for resectable thymic epithelial tumor is complete thymectomy under median sternotomy [4]. Thymic carcinoma and NET have more malignant potential with frequent lymph-node involvement and invasion of tissues other than thymoma, resulting in a poor prognosis [5]. However, for thymoma without myasthenia gravis, there are some reports that the prognosis after limited resection or minimally invasive surgery is similar to that after complete thymectomy [6,7,8]. Nevertheless, preoperative differentiation between thymoma, thymic carcinoma, and NET remains challenging.
In contrast, chemotherapy is generally indicated for malignant lymphoma [except for limited mucosa-associated lymphoid tissue (MALT) lymphoma] after making a definitive diagnosis; therefore, if the anterior mediastinal tumor is suspected to be malignant lymphoma, then a biopsy should be performed [9]. Some markers such as soluble interleukin-2 receptor antibody (sIL-2R Ab) and lactate dehydrogenase (LDH) can help narrow down the differential diagnosis; however, there are some lymphoma cases in which an elevation of these markers is not observed [10, 11]. In fact, 3.7% of patients who underwent diagnostic surgery for suspected thymic epithelial tumor were diagnosed with malignant lymphoma after surgery [12]. To avoid unnecessary surgery, the preoperative differential diagnosis should therefore be more accurate.
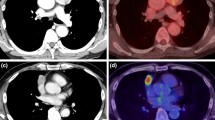
Magnetic resonance imaging and computed tomography are generally used as preoperative imaging examinations, although their contribution to preoperative diagnosis is limited [13]. Recently, positron-emission tomography/computed tomography (PET/CT) has been reported as a practical differential diagnostic tool for anterior mediastinal tumors, especially for distinguishing between thymoma and lymphoma, thymoma and thymic carcinoma, and even for predicting the histological type of thymoma [14,15,16]. Additionally, some tumor markers such as cytokeratin 19 fragment (CYFRA 21-1) and neuron-specific enolase (NSE) for thymic carcinoma, as well as sIL-2R Ab and LDH for lymphoma, have been reported to be efficient auxiliary diagnostic tools [17, 18]. However, these imaging examinations and tumor markers have been evaluated only in isolation. Therefore, we hypothesized that the combination of PET/CT and tumor markers could facilitate narrowing of the differential diagnosis. This study aimed to evaluate the efficacy of combined prediction using PET/CT and tumor markers for the differential diagnosis while focusing on thymic carcinoma, thymoma, and malignant lymphoma, which are clinically important and frequently occurring tumors.
Methods
Patients
The patients admitted to our department between January 2012 and December 2021 with anterior mediastinal tumors were retrospectively evaluated. Data, including patient characteristics, blood test results, PET/CT imaging, and pathological diagnosis, were collected from the medical records. Patients who received a definitive diagnosis of anterior mediastinal tumor through either biopsy or surgery were included. The exclusion criteria were as follows: (i) metastatic tumor, (ii) assessment performed after treatment, (iii) PET/CT not performed, and (iv) borderline tumor with indeterminate pathological diagnosis. The data for patients with no radiological reports of PET/CT or without the numeric data for the maximum standardized uptake value (SUVmax) at 60 min after the intravenous administration of 18-fludeoxyglucose were excluded and treated as missing data. This study was approved by the Institutional Review Board of University of Tsukuba Hospital (August 10, 2022, R04-103). The requirement for informed consent was waived due to the retrospective design of the study.
Evaluation
The patients were divided into four groups according to the pathological diagnosis as follows: thymic carcinoma, including NET, thymoma, lymphoma, and others. We compared the following clinical data between the pathological groups: age; SUVmax; tumor markers such as LDH, sIL-2R Ab, carcinoembryonic antigen (CEA), α-fetoprotein (AFP), CYFRA 21-1, squamous cell carcinoma antigen (SCCA), pro-gastrin-releasing peptide (proGRP), and NSE. For thymic carcinoma, including NET and lymphoma groups, the relationships with their histological subtypes and significant values obtained in the previous evaluations were also assessed.
Positron emission tomography protocol
PET/CT was conducted in most of the patients at the advanced imaging center affiliated with our institution and was performed as an auxiliary tool for the differential diagnosis at the discretion of the attending physician according to the following regulations: (i) patients had to avoid oral intake and exercise for 6 h and 24 h prior to the examinations, respectively; (ii) blood glucose levels had to be below 180 mg/dl before the examination. PET/CT was performed 60 min after the intravenous injection of 18-fludeoxyglucose at a dose calculated based on the patient’s body weight.
Statistical analysis
Each value is expressed as the mean ± standard deviation. The amount of variation in SUVmax and tumor markers was evaluated using a one-way analysis of variance between the groups, followed by Bonferroni correction in the groups with significant differences as a multiple-comparison correction. Sensitivity, specificity, and area under the curve (AUC) were calculated using receiver-operating characteristic (ROC) curves. The optimal cut-off values were determined with an emphasis on specificity to avoid any overdiagnosis. Data were analyzed using the SPSS version 27.0 software program (IBM Corporation, NY, USA). Statistical significance was set at P < 0.05.
Results
Patients
Of the 207 patients with anterior mediastinal tumors, 68 were excluded for the following reasons: (i) metastatic tumor (n = 8), (ii) assessment carried out after treatment (n = 2), (iii) PET/CT not performed (n = 57), and (iv) borderline tumor with an indeterminate pathological diagnosis (n = 1). In total, 139 patients were enrolled in this study. Four patients underwent PET/CT at other institutions.
Comparison between the pathologic groups
The characteristics of the clinical data are shown in Table 1, thus allowing for comparisons between the pathological groups. The number of cases (number of resected cases) of thymic carcinoma, including NET, thymoma, and lymphoma, was 16 (11), 78 (77), and 15 (1), respectively. Significant differences between the groups were found in age, SUVmax, LDH, sIL-2RAb, CYFRA 21-1, and NSE levels. Figure 1 shows detailed comparisons between the pathological groups for clinical data showing significant differences. SUVmax was significantly higher in lymphoma, thymic carcinoma including NET, and thymoma, in that order (Fig. 1b). CYFRA 21-1 was significantly higher in thymic carcinomas, including NET, than in all other groups (Fig. 1c). sIL-2R Ab and LDH levels were also significantly higher in lymphoma than in all other groups (except for LDH values in thymic carcinoma, including NET) (Fig. 1d, e).
Detailed comparison of the clinical data between the pathological groups (A: Age, B: SUVmax, C: CYFRA 21-1, D: LDH, E: sIL-2R Ab, F: NSE). B SUVmax was significantly higher in Lymphoma, Thymic carcinoma including NET, and Thymoma, in that order. C CYFRA 21-1 was significantly higher in Thymic carcinoma including NET compared to all other groups. D, E sIL-2R Ab and LDH were significantly higher in Lymphoma compared to all other groups (except for LDH values in thymic carcinoma including NET). F NSE was significantly higher in Lymphoma than in Thymoma and Others. The upper and lower borders of the boxes represent upper and lower quartiles. The horizontal line indicates the median value. The crosses represent the mean values. The whiskers show the minimum and maximum values, excluding outliers. *P < 0.05 and **P < 0.01 represent significant differences between the pathological groups. CYFRA 21-1: Cytokeratin 19 fragments. NET, neuroendocrine tumor; NSE, neuron-specific enolase; LDH: Lactate dehydrogenase; sIL-2R, soluble interleukin-2 receptor antibody; SUVmax: maximum standard uptake value
ROC curves
Tumor markers that were significantly higher than those in any other group were further evaluated using ROC curves. The ROC curves for SUVmax for the diagnosis of thymic carcinoma, including NET and lymphoma, and thymic carcinoma, including NET and lymphoma, are shown in Fig. 2a–c. The cut-off values for SUVmax for the diagnosis of lymphoma, thymic carcinoma including NET, and thymic carcinoma including NET and lymphoma were 12.32 (AUC = 0.934, specificity = 0.916, sensitivity = 0.867), 7.97 (AUC = 0.798, specificity = 0.768, sensitivity = 0.800), and 7.97 (AUC = 0.934, specificity = 0.900, sensitivity = 0.867), respectively.
ROC curves for the SUVmax for the diagnosis of A thymic carcinoma including NET (AUC = 0.798), B lymphoma (AUC = 0.934), and C thymic carcinoma including NET and lymphoma (AUC = 0.934). D ROC curve for CYFRA 21-1 for the diagnosis of thymic carcinoma including NET (AUC = 0.768). E ROC curve for sIL-2R Ab for the diagnosis of lymphoma (AUC = 0.958). CYFRA 21-1: Cytokeratin 19 fragment, NET: Neuroendocrine tumor, sIL-2R Ab: Soluble interleukin-2 receptor antibody, SUVmax: Maximum standard uptake value
The ROC curve for CYFRA 21-1 in the diagnosis of thymic carcinoma, including NET, is shown in Fig. 2d. The optimal cut-off value was 2.95 (AUC = 0.768, specificity = 0.961, sensitivity = 0.385). The ROC curve for sIL-2R Ab in the diagnosis of lymphoma is shown in Fig. 2e. The optimal cut-off value was 806 (AUC = 0.958, specificity = 0.982, sensitivity = 0.800).
Combination of SUVmax and tumor markers
Figure 3a shows the relationship between SUVmax, CYFRA 21-1 and pathological diagnosis (n = 93). The cut-off values were set at 8.0 for SUVmax and 3.0 for CYFRA 21-1 considering the results of the ROC curves, as shown in Fig. 3. Thymic carcinomas, including NET, tend to be located in the right upper area (high SUVmax and high CYFRA 21-1), whereas lymphoma tends to be located in the left upper area (high SUVmax and low CYFRA 21-1). The thymomas tend to be located in the lower area (low SUVmax). The accuracy rate for the diagnosis of thymic carcinoma including NET was 91.4% (specificity = 98.7, sensitivity = 41.6) using cut-off values (SUVmax = 8.0, CYFRA 21-1 = 3.0). Figure 3b shows the relationship between SUVmax, sIL-2R Ab, and pathological diagnosis (n = 105). The cut-off values were set at 12 for SUVmax and 800 for sIL-2R Ab, considering the results of the ROC curves, as shown in Fig. 3b. With respect to the diagnosis of lymphoma, the accuracy rate was 94.2% (specificity = 97.78%, sensitivity = 73.33%) using cut-off values (SUVmax = 12, sIL-2R Ab = 800).
A Relationship between the SUVmax, CYFRA 21-1 and the pathological diagnosis (n = 93). Thymic carcinoma tends to be located in the right upper area (high SUVmax and high CYFRA 21-1), and lymphoma tends to be located in the left upper area (high SUVmax and low CYFRA 21-1). Focusing on the diagnosis for thymic carcinoma including NET, the accuracy rate was 91.4% (specificity = 98.7%, sensitivity = 41.6%) using the cut-off values (SUVmax = 8.0, CYFRA 21-1 = 3.0). The red dotted line shows the cut-off values set at 8.0 for SUVmax and 3.0 for CYFRA 21-1. B Relationship between the SUVmax, sIL-2R Ab, and the pathological diagnosis (n = 105). Focusing on the diagnosis for lymphoma, the accuracy rate was 94.2% (specificity = 97.78%, sensitivity = 73.33%) using the cut-off values (SUVmax = 12, sIL-2R Ab = 800). The blue dotted line shows the cut-off values set at 12 for SUVmax and 800 for sIL-2R Ab. CYFRA 21-1: Cytokeratin 19 fragment, NET: Neuroendocrine tumor, sIL-2R Ab: Soluble interleukin-2 receptor antibody, SUVmax: Maximum standard uptake value
Histological subtypes
For thymic carcinomas, including NET, the histological subtypes were classified into five categories: squamous cell carcinoma, poorly differentiated squamous cell carcinoma, poorly differentiated carcinoma, typical carcinoid, and atypical carcinoid (Fig. 4a). CYFRA 21-1 tended to be high in poorly differentiated carcinomas. The histological subtypes of lymphoma were classified into four categories: MALT, B-cell, T-cell, and Hodgkin lymphomas (Fig. 4b). SUVmax tended to be low in patients with MALT lymphoma.
A Histological subtypes in thymic carcinoma including NET. CYFRA 21-1 tended to be high in poorly differentiated carcinoma. B Histological subtypes in lymphoma. SUVmax tended to be low in MALT lymphoma. CYFRA 21-1: cytokeratin 19 fragment, MALT: mucosa-associated lymphoid tissue, NET: neuroendocrine tumor, SUVmax: maximum standard uptake value
Discussion
The treatment strategy for anterior mediastinal tumors, including the surgical indications, preoperative biopsy, or initial surgery, changes depending on the preoperative diagnosis, particularly for resectable lesions. In this study, we evaluated the efficacy of the combination of PET/CT and tumor markers for the differential diagnosis of clinically important and frequently occurring tumors, including thymic carcinoma, thymoma, and malignant lymphoma, in keeping with clinically relevant situations.
A tumor marker analysis showed that sIL-2R Ab and LDH levels were significantly higher in lymphomas. In limited-stage malignant lymphoma, elevations in LDH and sIL-2R Ab have been observed in 50–80% and 55% of patients, respectively [10, 11]. Additionally, B symptoms are present in less than 20% of patients [11]. As these rates could differ depending on the histological subtypes, the preoperative accuracy, which can be achieved using these values in addition to imaging examinations, such as computed tomography and magnetic resonance imaging, would not be sufficiently high to determine the treatment strategy. As a matter of fact, this study includes a patient who was first diagnosed with malignant lymphoma through surgery.
In this study, CYFRA 21-1 was also significantly higher in thymic carcinomas, including NET, than in other groups, such as thymoma and malignant lymphoma. Additionally, CYFRA 21-1 tends to be higher in poorly differentiated (squamous cell) carcinoma than in other types of tumors, but there was no significant difference between the histological subtypes of thymic carcinoma. CYFRA 21-1 was reported by Shiiya et al. to be an efficient marker for the diagnosis of thymic carcinoma [17]. In their report, the cut-off value for the differential diagnosis between thymic carcinoma and thymoma was set at 2.7 (AUC = 0.86, specificity = 95.2, sensitivity = 68.8). The AUC was higher than that in our study, which could be due to the larger number of thymic carcinoma cases (n = 32) and exclusion of carcinoids in their study. However, there were also no significant differences in CYFRA 21-1 between the histological subtypes of thymic carcinoma, which was similar to our findings.
Despite its low frequency, thymic carcinoma has a variety of histological subtypes. Although thymic carcinoids are classified as thymic neuroendocrine neoplasms rather than thymic carcinomas, the characteristics of thymic carcinoids (such as low frequency, high invasiveness into surrounding tissues and lymph nodes, and the surgical indications for resectable lesions) are similar to those of thymic carcinomas; therefore, these tumors were classified as thymic carcinomas including NET in this study [2].
The SUVmax was significantly higher in lymphoma, thymic carcinoma including NET, and thymoma, in that order. There were significant differences between the groups, suggesting that SUVmax is an efficient indicator. These differences have been reported between thymoma and lymphoma or between thymoma and thymic carcinoma, and even for the prediction of histological types of thymoma [14,15,16]. Although a significant difference was observed between lymphoma and thymic carcinoma, there was some overlap, as shown in Fig. 1b. This differential diagnosis divides the options for the next strategy into initial surgery or biopsy; however, it would be difficult to distinguish them preoperatively based on the SUVmax alone.
The accuracy rate for the diagnosis of thymic carcinoma, including NET, was as high as 91.4% (specificity = 98.7, sensitivity = 41.6) using optimal cut-off values (SUVmax = 8, CYFRA 21-1 = 3). Although an elevation of CYFRA 21-1 in thymic carcinoma is not frequent, its accuracy can be enhanced when combined with SUVmax. The same can be said for lymphoma using cut-off values (SUVmax = 12, sIL-2R Ab = 800) to achieve an accuracy rate of 94.2% (specificity = 97.78%, sensitivity = 73.33%). Consequently, the combination of PET/CT and tumor markers can contribute to a more precise differential diagnosis of anterior mediastinal tumors.
Kanou et al. reported an SUVmax cut-off value of 5 (specificity = 0.75, sensitivity = 0.90) for distinguishing between thymic carcinoma and thymoma, which was lower than that in our report [16]. This may be because our cut-off value of 8 (specificity = 0.768, sensitivity = 0.800) was set with an emphasis on specificity to minimize the number of false-positive patients considering the additional risks of biopsy, as resectable thymic epithelial tumors should be treated with initial surgery according to the guidelines [19, 20]. The other candidate cut-off value was 6.36 (Fig. 2a), which was closer to that of Kanou et al. Byrd et al. also reported that a cut-off value of SUVmax less than 7.5 was highly suggestive of resectable thymoma, while a value greater than 12.85 was highly suggestive of lymphoma, which was similar to our findings [14].
While a limited resection is gaining acceptance for thymoma, sternotomy should be indicated for thymic carcinoma to achieve complete resection, which is one of the most significant prognostic factors [19, 21, 22]. Additionally, some reports suggested that systematic lymph-node dissection should be performed in cases of thymic carcinoma or NET because of the high rate of lymph-node involvement [3, 22, 23]. This method can also be beneficial for determining the surgical approach or range of resection preoperatively, which may contribute to better surgical outcomes.
A preoperative biopsy is considered in cases of unresectable lesions or in cases where malignant lymphoma or malignant germ cell tumors are suspected. In cases of thymic epithelial tumor, a biopsy could result in tumor implantation along the puncture route or pleural dissemination; therefore, initial surgery is recommended [24]. According to the European Society for Medical Oncology clinical practice guidelines, postoperative adjuvant radiation is considered for TNM stage I or higher in thymic carcinoma and TNM stage III or higher in thymoma [20]. Because thymic carcinoma tends to be found at an advanced stage, most cases of thymic carcinoma are treated with postoperative radiation therapy. The implantation risk due to preoperative biopsy could be offset to some degree by postoperative radiation in thymic carcinoma, therefore; a preoperative biopsy might be acceptable in such cases [19, 20]. In other words, the differential diagnosis not between lymphoma and others, but between thymic carcinoma in addition to lymphoma and others, could be an efficient method to decide the optimal treatment strategy for cases with high SUVmax (SUVmax > 8.0) that do not fit the criteria (CYFRA 21-1 > 3.0 or sIL-2RAb > 800) described above.
This study is associated with three limitations. First, it was a retrospective, single-site study. The analyzed data included missing data owing to the retrospective design of the study. PET/CT was conducted at the discretion of the attending physician. Therefore, PET/CT tended to be omitted in patients with suspected benign or small tumors. Moreover, if indicated, such tumors tended to present with a low uptake, which was displayed as non-numeric data labeled as “slight uptake” in our institution (minimum SUVmax = 1.49). These cases were categorized as having ‘missing data’. Second, we enrolled patients with anterior mediastinal tumors, regardless of whether or not the tumor was resectable. The degree of tumor progression could influence the PET/CT results and tumor markers. Moreover, in unresectable cases, the accuracy of the pathological diagnosis could be limited, because only small specimens were obtained through needle biopsy. Third, we categorized thymic carcinoid as “thymic carcinoma including NET”, even though thymic carcinoid has been classified as thymic NET rather than thymic carcinoma, in light of their similar treatment strategy. These histological subtypes have different features that can affect the results.
In conclusion, SUVmax and CYFRA 21-1 are significant indicators for the diagnosis of thymic carcinoma and lymphoma. An SUVmax higher than 8 could be an efficient indicator for the diagnosis of thymic carcinoma, including NET, in addition to lymphoma. Both an SUVmax higher than 8 and CYFRA 21-1 higher than 3.0 can be predictors of thymic carcinoma. The combination of these values demonstrated a more accurate preoperative diagnosis of anterior mediastinal tumors, which could contribute to the decision-making regarding the treatment strategies.
References
Carter BW, Marom EM, Detterbeck FC. Approaching the patient with an anterior mediastinal mass: a guide for clinicians. J Thorac Oncol. 2014;9:102–9.
Marx A, Chan JKC, Chalabreysse L, Dacic S, Detterbeck F, French CA, et al. The 2021 WHO classification of tumors of the thymus and mediastinum: what is new in thymic epithelial, germ cell, and mesenchymal tumors? J Thorac Oncol. 2022;17:200–13.
Carter BW, Benveniste MF, Madan R, Godoy MC, Groot PM, Truong MT, et al. IASLC/ITMIG staging system and lymph-node map for thymic epithelial neoplasms. Radiographics. 2017;37:758–76.
Guerrera F, Falcoz PE, Moser B, van Raemdonck D, Bille A, Toker A, et al. Thymomectomy plus total thymectomy versus simple thymomectomy for early-stage thymoma without myasthenia gravis: a European society of thoracic surgeons thymic working group study. Eur J Cardiothorac Surg. 2021;60:881–7.
Litvak AM, Woo K, Hayes S, Huang J, Rimner A, Sima CS, et al. Clinical characteristics and outcomes for patients with thymic carcinoma: evaluation of Masaoka staging. J Thorac Oncol. 2014;9:1810.
Voulaz E, Perroni G, Russo A, Patirelis A, Mangiameli G, Alloisio M, et al. Thymomectomy versus complete thymectomy in early-stage non-myasthenic thymomas: a multicentric propensity score-matched study. Interact Cardiovasc Thorac Surg. 2022;35:167.
Yang CJ, Hurd J, Shah SA, Liou D, Wang H, Backhus LM, et al. A national analysis of open versus minimally invasive thymectomy for stage I to III thymoma. J Thorac Cardiovasc Surg. 2020;160:555–67.
Nakagawa K, Yokoi K, Nakajima J, Tanaka F, Maniwa Y, Suzuki M, et al. Is thymomectomy alone appropriate for stage I (T1N0M0) thymoma? Results of a propensity-score analysis. Ann Thorac Surg. 2016;101:520–6.
Zhou MX, Chen YY, Zhang JQ, Bai WL, Huang C, Guo C, et al. A systematic review and meta-analysis of thymic mucosa-associated lymphoid tissue lymphoma. J Thorac Dis. 2022;14(7):2894–907.
Yamashita H, Izutsu K, Nakamura N, Shiraishi K, Chiba S, Kurokawa M, et al. Treatment results of chemoradiation therapy for localized aggressive lymphomas: a retrospective 20-year study. Ann Hematol. 2006;85:523–9.
Martelli M, Ferreri A, Di Rocco A, Ansuinelli M, Johnson PWM. Primary mediastinal large B-cell lymphoma. Crit Rev Oncol Hematol. 2017;113:318–27.
Kent MS, Wang T, Gangadharan SP, Whyte RI. What is the prevalence of a “nontherapeutic” thymectomy? Ann Thorac Surg. 2014;97:276–82.
Ackman JB, Verzosa S, Kovach AE, Louissaint A Jr, Lanuti M, Wright CD, et al. High rate of unnecessary thymectomy and its cause. Can computed tomography distinguish thymoma, lymphoma, thymic hyperplasia, and thymic cysts? Eur J Radiol. 2015;84:524–33.
Byrd CT, Trope WL, Bhandari P, Konsker HB, Moradi F, Lui NS, et al. Positron emission tomography/computed tomography differentiates resectable thymoma from anterior mediastinal lymphoma. J Thorac Cardiovasc Surg. 2023;165:371–81.
Watanabe T, Shimomura H, Mutoh T, Saito R, Goto R, Yamada T, et al. Positron emission tomography/computed tomography as a clinical diagnostic tool for anterior mediastinal tumors. Surg Today. 2019;49:143–9.
Kanou T, Funaki S, Minami M, Ose N, Kimura T, Fukui E, et al. Usefulness of positron-emission tomography for predicting the World Health Organization grade of thymic epithelial tumors. Thoracic Cancer. 2022;13:1651–6.
Shiiya H, Ujiie H, Hida Y, Kato T, Kaga K, Wakasa S, et al. Elevated serum CYFRA 21-1 level as a diagnostic marker for thymic carcinoma. Thoracic Cancer. 2021;12:2933–42.
Mimori T, Shukuya T, Ko R, Okuma Y, Koizumi T, Imai H, et al. Clinical significance of tumor markers for advanced thymic carcinoma: a retrospective analysis from the NEJ023 Study. Cancers (Basel). 2022;14:331.
Falkson CB, Vella ET, Ellis PM, Maziak DE, Ung YC, Yu E. Surgical, radiation, and systemic treatments of patients with thymic epithelial tumours: a clinical practice guideline. J Thorac Oncol. 2022;17:1258–75.
Girard N, Ruffini E, Marx A, Faivre-Finn C, Peters S. Thymic epithelial tumours: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2015;26(Suppl 5):v40-55.
Kim S, Bull DA, Hsu CH, Hsu CC. The role of adjuvant therapy in advanced thymic carcinoma: a national cancer database analysis. Ann Thorac Surg. 2020;109:1095–103.
Cheufou DH, Valdivia D, Puhlvers S, Fels B, Weinreich G, Taube C, et al. Lymph node involvement and the surgical treatment of thymic epithelial and neuroendocrine carcinoma. Ann Thorac Surg. 2019;107:1632–8.
Brascia D, De Palma A, Schiavone M, De Iaco G, Signore F, Panza T, et al. Lymph nodes involvement and lymphadenectomy in thymic tumors: tentative answers for unsolved questions. Cancers (Basel). 2021;13:5085.
Kattach H, Hasan S, Clelland C, Pillai R. Seeding of stage I thymoma into the chest wall 12 years after needle biopsy. Ann Thorac Surg. 2005;79:323–4.
Acknowledgements
The authors appreciate Cosmin Florescu (Medical English Communications Center, University of Tsukuba) for grammatical revision of this manuscript.
Funding
There was no funding support for this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest in association with this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yanagihara, T., Kawamura, T., Maki, N. et al. Practical methods to differentiate thymic malignancies by positron-emission tomography and tumor markers. Surg Today 54, 899–906 (2024). https://doi.org/10.1007/s00595-024-02801-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-024-02801-5