Abstract
Purpose
Some patients have worse actual observed postoperative (apo) respiratory function values than predicted postoperative (ppo) values. The present study therefore clarified the predictive factors that hinder the recovery of the postoperative respiratory function.
Methods
This study enrolled 255 patients who underwent anatomical pulmonary resection for lung cancer. A pulmonary function test (PFT) was carried out before surgery and at one, three, and six months after surgery. In each surgical procedures, the forced expiratory volume in 1 s (FEV1) ratio was calculated as the apo value divided by the ppo value. In addition, we investigated the predictive factors that inhibited postoperative respiratory function improvement in patients with an FEV1 ratio < 1.0 at 6 months after surgery.
Results
The FEV1 ratio gradually improved over time in all surgical procedures. However, 49 of 196 patients who underwent a PFT at 6 months after surgery had an FEV1 ratio < 1.0. In a multivariate analysis, right side, upper lobe, segmentectomy and pleurodesis for prolonged air leakage were independent significant predictors of a decreased FEV1 ratio (p = 0.003, 0.006, 0.001, and 0.009, respectively).
Conclusion
Pleurodesis was the only controllable factor that might help preserve the postoperative respiratory function. Thus, the intraoperative management of air leakage is important.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Evaluating the pulmonary function is important for estimating the risk of postoperative complications in the field of general thoracic surgery. In patients with lung cancer, a pulmonary function test (PFT) is a preoperative evaluation test that can determine the indication for surgery. Furthermore, several reports have shown a close relationship between the pulmonary function, postoperative complications, and quality of life [1,2,3,4,5].
According to the guidelines of the European Respiratory Society and the European Society of Thoracic Surgery [6], the predicted postoperative (ppo) forced expiratory volume in 1 s (FEV1) is commonly used in the evaluation of lung resection candidates. However, the ppoFEV1 tends to be underestimated in patients with moderate to severe chronic obstructive pulmonary disease (COPD) because of the “lung volume reduction effect”, which states that resection of emphysematous lung parenchyma improves the postoperative pulmonary function [7, 8]. The diffusing capacity of the lung for carbon monoxide (DLCO), together with the FEV1, is used to evaluate of lung resection candidates, as the DLCO is associated with perioperative mortality and morbidity even in patients with a normal FEV1 or in those without COPD [6, 9, 10].
Thoracic surgeons calculate the ppoFEV1 and ppoDLCO according to the “anatomical method” and subsequently estimate the risk of postoperative mortality and morbidity. In fact, there is some variation in the actual observed postoperative (apo) pulmonary function depending on the extent of lung resection and the duration after surgery due to an imbalance in the air flow and blood flow distribution caused by the anatomical and physiological conditions. Yokoba reported that improvements in the postoperative pulmonary function and symptoms varied according to the resected lobe [11]. In clinical practice, some patients have a decreased quality of life and respiratory symptoms, such as shortness of breath, because of a worse postoperative respiratory function than had been predicted preoperatively.
The present study therefore clarified the factors that inhibit postoperative respiratory function improvement. We retrospectively compared the ppo values with the apo values on the PFT performed one, three, and six months after surgery according to the surgical procedures and analyzed the predictors of patients with apo values lower than their ppo values.
Patients and methods
Study population
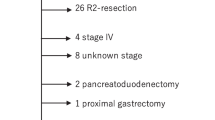
This was a retrospective single-institutional study. Between January 2017 and December 2017, a total of 454 patients underwent pulmonary resection for primary lung cancer at Juntendo University Hospital. Of those, 391 patients underwent anatomical pulmonary resection, such as segmentectomy, lobectomy, bilobectomy, and pneumonectomy. Among these 391 patients, 38 undergoing 36 lobectomies combined with wide wedge resection and 2 lobectomies with chest wall resection were excluded because their ppo values could not be accurately calculated. In addition, 98 patients with missing postoperative PFT data were also excluded. Therefore, the remaining 255 patients were the study subjects (Fig. 1). These patients underwent the following procedures: lobectomy (n = 192), pneumonectomy (n = 4), bilobectomies (n = 11), lobectomies with bronchoplasty (n = 5), and segmentectomy (n = 43). The medical records of each patient were retrospectively reviewed under a waiver of authorization with approval by the Institutional Review Board of the Juntendo University School of Medicine (No: 16–084).
Surgical technique
A total of 178 patients underwent pulmonary resection by posterolateral or anterolateral open thoracotomy (over 8-cm skin incision), 45 underwent video-assisted thoracic surgery, and 32 underwent robot-assisted thoracic surgery. In segmentectomy, dissection of the inter-segmental plane was performed via stapler and/or electrocautery. We controlled the air leakages detected in the intraoperative sealing test by suturing the lung parenchyma and covering it with sealing materials, such as a polyglycolic acid sheet and fibrin glue. Prolonged air leakage was defined in cases where postoperative air leakage persisted for more than five days. For patients with prolonged air leakage, chemical pleurodesis by intrathoracic administration of the sclerosing agent OK432, with or without 50 mL of autologous blood through the chest tube, was initially performed according to the clinical judgement of the attending doctor for each patient [12]. Failing that, re-operation was considered in order to control prolonged air leakage.
Evaluating the perioperative pulmonary function
The patients underwent a PFT, including assessments of the FEV1, vital capacity (VC), and DLCO before surgery and at one, three, and six months after surgery. A total of 255 patients enrolled in the present study underwent a PFT at least once at 1, 3, and 6 months after surgery. At our institute, preoperative PFT and thin-section computed tomography (CT) are usually performed within one month prior to surgery. We evaluated the number of functioning/obstructed segments on thin-section CT and calculated the ppo values using the following formula [6]: ppo values = preoperative value × (1 – a/b), where a is the number of functioning or unobstructed segments to be resected and b is the total number of functioning or unobstructed lung segments. The FEV1, VC, and DLCO ratios were calculated using the following formulae: FEV1 ratio = apoFEV1/ppoFEV1, VC ratio = apoVC/ppoVC, and DLCO ratio = apoDLCO/ppoDLCO.
Evaluating the predictors of a decreased FEV1 ratio
Data of patients with an FEV1 ratio < 1.0 at 6 months after surgery were extracted and evaluated for their clinical characteristics, and intraoperative and postoperative data were extracted to investigate predictive factors that impeded recovery of the postoperative respiratory function. The clinical characteristics analyzed were the age, sex, body mass index, pack-years of smoking, location of tumors, radiological findings on thin-section CT, FEV1, VC, and DLCO. All CT findings with respect to the radiological changes of interstitial pneumonia and emphysema were reviewed by one blinded independent radiologist, one pulmonary medicine physician, and at least two thoracic surgeons [13]. We retrospectively examined the intraoperative data, such as surgical procedure, operation time, amount of bleeding, use of sealant materials, length of wound, number of staplers used to cut the pulmonary parenchyma, presence of adhesion, and postoperative data, such as whether or not chemical pleurodesis for prolonged air leakage and adjuvant chemotherapy had been performed.
Statistical analyses
The FEV1, VC, and DLCO ratio at each point after surgery were compared using Wilcoxon’s signed-rank test. A logistic regression analysis was conducted to investigate the predictive factors causing apoFEV1 values to be lower than ppoFEV1 values.
Statistical analyses were performed using the JMP Pro 14 software program (SAS Institute Inc, Cary, NC, USA), and values of p < 0.05 were considered significant.
Results
Table 1 summarizes the patients’ characteristics. The number of right anatomical pulmonary resections was 162 (64%). Thirty-four (13%) patients were found to have interstitial changes on thin-section CT, while 57 (22%) were found to have emphysematous changes on thin-section CT. As shown in Table 1, of the 255 eligible patients who underwent anatomical lung resection for lung cancer, 192 underwent lobectomy, 4 underwent pneumonectomy, 11 underwent bilobectomy, 5 underwent lobectomy with bronchoplasty, and 43 underwent segmentectomy. Notably, there were 69 right upper lobectomies, 13 right middle lobectomies, 40 right lower lobectomies, 48 left upper lobectomies, and 22 left lower lobectomies. There were two patients each who underwent right or left pneumonectomy. There were five right upper-middle bilobectomies and six right middle-lower bilobectomies. Among the five lobectomies with bronchoplasty, three were right upper sleeve lobectomy, one was left upper sleeve lobectomy, and one was left lower sleeve lobectomy. Regarding segmentectomy, the resected segment was S1 + 2 in 1 patient, S1 in 3 patients, S2 in 2 patients, S3 in 2 patients, S6 in 11 patients, S8 in 2 patients, basal segment in 3 patients on the right side, S6 in 3 patients, S1 + 2 + 3 in 11 patients, and basal segment in 5 patients on the left side.
Table 2 shows the FEV1 ratio according to surgical procedure. Except for segmentectomy, the apoFEV1 exceeded the ppoFEV1 following all procedures until 3 months after surgery (FEV1 ratio for all procedures = 1.05, 95% CI 1.03–1.08). Furthermore, in all procedures, the apoFEV1 was higher than the ppoFEV1 at 6 months after surgery (FEV1 ratio = 1.10, 95% CI 1.08–1.13). The FEV1 ratio at 6 months after surgery was 1.04 in right upper and 1.07 in right middle lobectomy. In contrast, the ratio was increased to 1.14 in left upper, 1.20 in left lower, and 1.19 in right lower lobectomy. Patients after pneumonectomy showed a high FEV1 ratio (FEV1 ratio = 1.25 at 3 months), and those who underwent segmentectomy showed an FEV1 ratio of 1.02 at 6 months after surgery.
Supplemental Tables 1 and 2 show the VC and DLCO ratios by surgical procedure. Regarding the VC (Supplemental Table 1), the apoVC was less than the ppoVC in most cases at 3 months after surgery (VC ratio in all procedures = 0.99, 95% CI 0.97–1.01). Until 6 months after surgery, the apoVC exceeded the ppoVC (VC ratio in all procedures = 1.04, 95% CI 1.02–1.06). The VC ratio of right middle lobectomy and segmentectomy was < 1.0, even at 6 months after surgery (VC ratio = 0.99 and 0.97, respectively). The same tendency as with the FEV1 ratio was seen with the DLCO ratio (Supplemental Table 2); the apoDLCO at 3 months after surgery was approximately equivalent to the ppoDLCO (DLCO ratio in all procedures = 1.00, 95% CI 0.97–1.03), except for in cases of right upper lobectomy and segmentectomy (DLCO ratio = 0.92 and 0.93, respectively), and the ratio with right upper lobectomy and segmentectomy remained < 1.0 even at 6 months after surgery (DLCO ratio = 0.96 and 0.97, respectively).
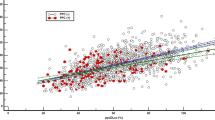
Regarding the change in the FEV1 ratio over time in all surgical procedures, the residual respiratory function after surgery gradually improved (median FEV1 ratio at 1, 3, and 6 months = 0.95, 1.05, and 1.10, respectively; Fig. 2). A total of 49 of 196 patients who underwent PFT had lower apoFEV1 values than ppoFEV1 values at 6 months after surgery (Fig. 3). Therefore, we investigated the predictive factors that inhibited the postoperative improvement of the pulmonary function.
Postoperative changes in the FEV1 ratio at one, three, and six months after surgery. Data are shown as the median with the interquartile range (IQR). a FEV1 ratio at 1 month after surgery (median = 0.95, IQR = 0.84–1.06); b FEV1 ratio at 3 months after surgery (median = 1.05, IQR = 0.94–1.18); c FEV1 ratio at 6 months after surgery (median = 1.10, IQR = 1.00–1.22); *, Wilcoxon’s signed-rank test
As shown in Table 3, the overall cohort consisted of 113 male and 83 female participants. The patients ranged in age from 27 to 90 years old, with a median age of 69 years old. Among them, 49 (25%) patients showed an FEV1 ratio < 1.0 at 6 months after surgery (decreased FEV1 ratio group). Of these 49 patients, 38 (77%) had a tumor in the right side (p = 0.017), and 34 (69%) had a tumor in the upper lobe (p = 0.042). Radiological changes on thin-section CT (interstitial change and emphysematous change, p = 0.085 and 0.61, respectively) and the preoperative pulmonary function (%VC, %FEV1, DLCO, p = 0.70, 0.24, 0.96, respectively) were not predictive factors for a decreased FEV1 ratio. Regarding intra- and postoperative factors, 15 (30%) patients in the decreased FEV1 ratio group had undergone segmentectomy (p = 0.014). Other intraoperative factors, such as the surgical technique, operation time, amount of bleeding, use of sealant, length of wound, number of staplers used, and presence of adhesion were not predictive factors for a decreased FEV1 ratio (p = 0.79, 0.18, 0.61, 0.77, 0.21, 0.86, and 0.63, respectively). In the early postoperative period, pleurodesis for prolonged air leakage was performed in 19 (9%) patients. Among these patients, lobectomy was performed in 15, segmentectomy in 3, and bilobectomy in 1. Although three patients underwent pleurodesis twice, none underwent re-operation to manage prolonged air leakage. Nine (18%) patients were in the decreased FEV1 ratio group and 10 (6%) patients were in the recovered FEV1 ratio group. Pleurodesis was one predictive factor of a low FEV1 ratio according to a univariate analysis (p = 0.025).
In multivariate analyses, right side, upper lobe, segmentectomy, and pleurodesis were independent significant predictive factors for a decreased FEV1 ratio (p = 0.003, 0.006, 0.001, and 0.009, respectively; Table 4).
Discussion
We compared ppo values to apo values for each lobe and each surgical procedure and analyzed factors that inhibited the postoperative respiratory function improvement. The apoFEV1 was found to equivalent to the ppoFEV1 in cases of right upper, middle lobectomy, and segmentectomy at 6 months after surgery (FEV1 ratio = 1.04, 1.07, and 1.02, respectively). In contrast, in cases of left upper, left lower, and right lower lobectomies, the apoFEV1 exceeded the ppoFEV1 (FEV1 ratio = 1.14, 1.20, and 1.19, respectively). In this study, the location of the tumor (right side and upper lobe), segmentectomy, and postoperative pleurodesis were revealed to be predictive factors for an inhibited postoperative pulmonary function improvement (p = 0.003, 0.006, 0.001, and 0.009, respectively).
Brunelli et al. evaluated the predicted versus observed FEV1 and DLCO values in 200 consecutive patients undergoing lobectomy or pneumonectomy [14]. They noted that the apoFEV1 was 3% higher than the ppoFEV1, and the apoDLCO was 6% higher than the ppoDLCO at 3 months after lobectomy. In our study, the apoFEV1 and apoDLCO were 8% and 2% higher, respectively, than the associated ppo values at 3 months after lobectomy. Our results were compatible with those previous findings, and any slight differences in these two studies may have been due to patients’ physique, the study population undergoing the surgical procedure, and patients’ postoperative physical condition.
Regarding the FEV1 ratio at 6 months after surgery (Table 2), the apoFEV1 values in right lower, left upper, and left lower lobectomies were 1.14–1.20 times higher than the ppoFEV1 values. In contrast, the apoFEV1 values in segmentectomy were approximately the same as the ppoFEV1 values (FEV1 ratio = 1.02). Although segmentectomy has an advantage over lobectomy in that it can preserve the pulmonary function [15, 16], the outcomes remain controversial; indeed, several reports have concluded that segmentectomy did not contribute to the preservation of the postoperative pulmonary function compared to lobectomy [17,18,19]. The reason was that the residual ipsilateral lung and the contralateral lung expanded in a compensatory manner after major pulmonary resection. Ueda et al. reported that the extent of loss between the segmentectomy and lobectomy groups was not significantly different because the expansion of the bilateral residual lung after lobectomy was greater than that after segmentectomy [17]. Yamagishi et al. recently reported that a greater expansion after anatomical pulmonary resection occurred in the lobe next to the diaphragm than in the other lobes [20]. Thus, in left upper and either-side lower lobectomy, the actual observed postoperative pulmonary function was expected to be higher than the predicted postoperative pulmonary function due to significant postoperative expansion of the residual lung.
For the right upper and middle lobectomy procedures, the FEV1 ratios at 6 months after surgery were 1.04 and 1.07, respectively. Why the apoFEV1 was not further improved in these procedures might be due to only slight compensatory lung expansion or deformity of the bronchus after surgery. The amount of resected lung parenchyma in these procedures was smaller than that in left upper and both-sides lower lobectomy procedures, so postoperative compensatory lung expansion was relatively small. Furthermore, excessive upward bending and deviation of the right middle bronchus can occur after right upper lobectomy, which reduces the right middle lobe volume [21]. Yoshimoto et al. suggested that right upper segmentectomy might increase the FEV1 of the remaining right middle lobe because deformation of the right middle lobe does not occur due to the presence of remnant right upper lung parenchyma [19]. Thus, the FEV1 ratio after right upper and middle lobectomy might be lower than that after other lobectomy procedures.
Four predictive factors inhibiting the improvement of the postoperative pulmonary function were identified based on a multivariate analysis: tumor side, location, surgical procedure (segmentectomy), and postoperative chemical pleurodesis. Among them, the tumor side and tumor location are unalterable factors, as they depend on the location of the tumor. The surgical procedure was determined by the tumor invasiveness and comorbidities of the patient and thus was similarly difficult to change. We usually determine the surgical procedure for patients with lung cancer based on radiological findings, such as a solid component and/or ground-glass opacity on CT, the degree of 18-F-fluorodeoxyglucose accumulation in the tumor or lymph nodes on positron emission tomography (PET), and the patient’s surgical tolerance, especially in patients with cardiopulmonary comorbidities. Postoperative chemical pleurodesis for prolonged air leakage was thus considered to be the only controllable factor for preventing the inhibition of postoperative pulmonary improvement.
Maeyashiki et al. described the loss of the pulmonary function in patients who underwent postoperative pleurodesis after segmentectomy as being comparable to that in patients who underwent lobectomy [22]. Furthermore, they mentioned that pleural visceral thickening and adhesion with residual lung after pleurodesis led to a significant loss of the postoperative pulmonary function. Preventing pleurodesis with air leakage is thus important for ensuring recovery of the postoperative pulmonary function.
Several limitations associated with the present study warrant mention. First, this was a retrospective single-institution study. Therefore, the number of patients enrolled in this study was small, and there was a selection bias among this cohort with regard to the decision on which surgical technique and surgical procedure to perform. Second, the PFT may contain measurement errors because of postoperative pain and the patient’s physical condition. Indeed, PFT results are not always reproducible, especially in elderly patients or patients with a low performance status.
Conclusion
The apoFEV1exceeded the ppoFEV1 in cases of left upper, left lower, and right lower lobectomy (FEV1 ratio = 1.14, 1.20, and 1.19, respectively). According to a multivariate analysis, the tumor location (right side and upper lobe), segmentectomy, and postoperative pleurodesis were predictive factors for inhibiting postoperative pulmonary function improvement. Pleurodesis was the only controllable factor among these predictive factors, so the intraoperative management of air leakage is important to avoid postoperative pleurodesis.
Data availability
The data underlying this article cannot be shared publicly due to the privacy of individuals that participated in the study.
Abbreviations
- PFT:
-
Pulmonary function test
- FEV1:
-
Forced expiratory volume in 1 s
- VC:
-
Vital capacity
- DLCO:
-
Diffusing capacity of the lung for carbon monoxide
- ppo:
-
Predicted postoperative
- apo:
-
Actual observed postoperative
References
Sarna L, Evangelista L, Tashkin D, Padilla G, Holmes C, Brecht ML, et al. Impact of respiratory symptoms and pulmonary function on quality of life of long-term survivors of non-small cell lung cancer. Chest. 2004;125(2):439–45.
Pierce RJ, Copland JM, Sharpe K, Barter CE. Preoperative risk evaluation for lung cancer resection: predicted postoperative product as a predictor of surgical mortality. Am J Respir Crit Care Med. 1994;150:947–55.
Miyazaki T, Callister MEJ, Franks K, Dinesh P, Nagayasu T, Brunelli A. Minute ventilation-to-carbon dioxide slope is associated with postoperative survival after anatomical lung resection. Lung Cancer. 2018;125:218–22.
Kearney DJ, Lee TH, Reilly JJ, DeCamp MM, Sugarbaker DJ. Assessment of operative risk in patients undergoing lung resection. Importance of predicted pulmonary function. Chest. 1994;105:753–9.
Wang JS. Relationship of carbon monoxide pulmonary diffusing capacity to postoperative cardiopulmonary complications in patients undergoing pneumonectomy. Kaohsiung J Med Sci. 2003;19:437–46.
Brunelli A, Charloux A, Bolliger CT, Rocco G, Sculier JP, Varela G, et al. ERS/ESTS clinical guidelines on fitness for radical therapy in lung cancer patients (surgery and chemo-radiotherapy). Eur Respir J. 2009;34:17–41.
Korst RJ, Ginsberg RJ, Ailawadi M, Bains MS, Downey RJ Jr, Rusch VW, et al. Lobectomy improves ventilatory function in selected patients with severe COPD. Ann Thorac Surg. 1998;66:898–902.
Ueda K, Murakami J, Sano F, Hayashi M, Kobayashi T, Kunihiro Y, et al. Assessment of volume reduction effect after lung lobectomy for cancer. J Surg Res. 2015;197:176–82.
Brunelli A, Refai MA, Salati M, Sabbatini A, Morgan-Hughes NJ, Rocco G. Carbon monoxide lung diffusion capacity improves risk stratification in patients without airflow limitation: evidence for systematic measurement before lung resection. Eur J Cardiothorac Surg. 2006;29:567–70.
Ferguson MK, Vigneswaran WT. Diffusing capacity predicts morbidity after lung resection in patients without obstructive lung disease. Ann Thorac Surg. 2008;85:1158–64.
Yokoba M, Ichikawa T, Harada S, Naito M, Sato Y, Katagiri M. Postoperative pulmonary function changes according to the resected lobe: a 1-year follow-up study of lobectomized patients. J Thorac Dis. 2018;10(12):6891–902.
Takamochi K, Imashimizu K, Fukui M, Maeyashiki T, Suzuki M, Ueda T, et al. Utility of objective chest tube management after pulmonary resection using a digital drainage system. Ann Thorac Surg. 2017;104:275–83.
Fukui M, Takamochi K, Suzuki K, Ando K, Matsunaga T, Hattori A, et al. Advantages and disadvantages of corticosteroid use for acute exacerbation of interstitial pneumonia after pulmonary resection. Gen Thorac Cardiovasc Surg. 2021;69:472–7.
Brunelli A, Refai M, Salati M, Xiume F, Sabbatini A. Predicted versus observed FEV1 and DLCO after major lung resection: a prospective evaluation at different postoperative periods. Ann Thorac Surg. 2007;83:1134–9.
Nomori H, Shiraishi A, Cong Y, Sugimura H, Mishima S. Differences in postoperative changes in pulmonary functions following segmentectomy compared with lobectomy. Eur J Cardiothorac Surg. 2018;53:640–7.
Okada M, Koike T, Higashiyama M, Yamato Y, Kodama K, Tsubota N. Radical sublobar resection for small-sized non-small cell lung cancer: a multicenter study. J Thorac Cardiovasc Surg. 2006;132:769–75.
Ueda K, Tanaka T, Hayashi M, Li TS, Tanaka N, Hamano K. Computed tomography-defined functional lung volume after segmentectomy versus lobectomy. Eur J Cardiothorac Surg. 2010;37:1433–7.
Deng B, Cassivi SD, de Andrade M, Nichols FC, Trastek VF, Wang Y, et al. Clinical outcomes and changes in lung function after segmentectomy versus lobectomy for lung cancer cases. J Thorac Cardiovasc Surg. 2014;148:1186–92.
Yoshimoto K, Nomori H, Mori T, Ohba Y, Shiraishi K, Tashiro K, et al. Postoperative change in pulmonary function of the ipsilateral preserved lung after segmentectomy versus lobectomy. Eur J Cardiothorac Surg. 2010;37:36–9.
Yamagishi H, Chen-Yoshikawa TF, Oguma T, Hirai T, Date H. Morphological and functional reserves of the right middle lobe: radiological analysis of changes after right lower lobectomy in healthy individuals. J Thorac Cardiovasc Surg. 2021;162:1417–23.
Irani B, Miller JE, Linberg E, Attar S. Use of radiopaque markings on middle lobe (or lingula) following upper resectional surgery. Ann Thorac Surg. 1968;5:1–7.
Maeyashiki T, Takamochi K, Matsunaga T, Oh S, Suzuki K. Negative impact of chemical pleurodesis on postoperative pulmonary function for managing prolonged air leakage after segmentectomy. Gen Thorac Cardiovasc Surg. 2021;69:707–15.
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.
Funding
This work was supported in part by a Grant-in-Aid for Cancer Research from the Ministry of Health, Labour, and Welfare of Japan, and the Smoking Research Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ueno, H., Takamochi, K., Hirayama, S. et al. Predictive factors inhibiting recovery of the respiratory function after anatomical pulmonary resection. Surg Today 53, 1081–1088 (2023). https://doi.org/10.1007/s00595-023-02666-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-023-02666-0