Abstract
Purpose
Peritoneal metastasis (PM) in patients with colorectal cancer (CRC) is associated with poor prognosis. We conducted this study to assess whether palliative resection (PR) of the primary tumor improved the overall survival (OS) of patients with PM-CRC.
Methods
We analyzed retrospectively, data collected prospectively from patients with CRC. PM was categorized into three subgroups according to the Japanese classification of PM. A propensity‐score model was used to compare the outcomes of patients who underwent PR (PR group) and those who did not [non‐resection (NR) group].
Results
Among 1909 patients with metastatic CRC, 309 (16 %) had only peritoneal metastases and 255 of these patients who underwent palliative surgery (R2) were the subjects of our analysis: 161 in the PR group and 94 in the NR group. Median OS was significantly longer in the PR group than in the NR group (23 vs. 11 months, P < 0.001). Patients in the PR group had less extensive PM and a higher rate of receiving palliative chemotherapy than those in the NR group (P < 0.001). In a Cox multivariate analysis of 69 propensity‐score matched pairs, PR resulted in significantly longer OS than NR (hazard ratio 0.496, 95 % confidence interval 0.268–0.919, P = 0.025).
Conclusions
Our results show that PR resulted in better OS than NR for patients with PM-CRC, when their overall condition permitted a more aggressive approach.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Clinical manifestations, prognosis, and treatment of patients with metastatic colorectal cancer (mCRC) differ according to the metastatic sites. Peritoneal metastasis (PM) of CRC (PM-CRC), which is found in 5–13 % of patients with primary CRC, is associated with a very poor prognosis [1–3]. These patients have poorer survival than patients with other manifestations of mCRC [4]. In fact, PM and multiple metastases associated with CRC have been classified as stage IVB by the 7th edition of American Joint Committee on Cancer (AJCC) staging system [5].
Traditional treatment for PM-CRC consists of systemic chemotherapy with or without palliative surgery, generally resulting in a median survival of less than 6 months [3]. In the 1990s, studies on cytoreduction surgery (CRS) with perioperative intraperitoneal chemotherapy (PIC), including hyperthermic intraperitoneal chemotherapy (HIPEC), introduced a new treatment option for selected patients with PM-CRC [6–8]. However, this multimodality treatment can be performed only in specialized referral centers, where surgical oncologists are experienced in these procedures and special equipment is available for the HIPEC. Despite the recent developments in chemotherapeutic options and surgical procedures, improvement in the overall outcomes of patients with PM-CRC has been limited compared with that of patients with other types of mCRC [1].
Despite controversy about the survival benefit of palliative resection as the first-line treatment for unresectable mCRC, surgery remains the first-line treatment for symptomatic patients with mCRC. Previously, our group reported that patients with unresectable liver metastasis who underwent palliative resection (PR) had better survival than those who did not undergo resection [9]. Although PM is more aggressive than hepatic metastasis, we hypothesized that primary tumor resection improves the survival of patients with PM-CRC. The aim of this study was to assess the survival benefit of palliative resection of the primary tumor in patients with PM-CRC using a prospective cohort of more than 1900 patients with mCRC.
Materials and methods
Patients and parameters
We analyzed retrospectively, prospective data on patients with CRC, treated at our tertiary referral center over a 13-year period (2000–2012). Among 13,657 consecutive patients with primary CRC who underwent surgery, 1909 (14.0 %) were found to have stage IV CRC, 309 (16.2 %) of whom had only PM. The 54 patients who underwent surgery with curative intent (R0, R1) were excluded. Thus, 255 patients who underwent palliative surgery (R2) as the first-line treatment were the subjects of this study.
Clinicopathological factors analyzed included preoperative serum carcinoembryonic antigen (CEA) concentration, primary diagnosis, primary symptoms, comorbidities, site of the primary lesion, the presence of preoperative obstruction, tumor attachment to other structures, pathologic results, degree of PM, curability of surgery, postoperative complications, mortality, and postoperative palliative chemotherapy [10]. Clinical, radiographic, and computer records were retrospectively reviewed. During chart review, additional data were gathered regarding American Society of Anesthesiologist (ASA) score, Eastern Cooperative Oncology Group (ECOG) performance status, and survival status from the Korean National Registry of medical insurance. Major complications requiring reoperation or hospitalization were also recorded. Operative mortality was defined as death during the hospital stay or within 30 days after surgery. Symptomatic patients were limited to those who needed immediate intervention, such as surgery, stent insertion, transfusion, or medication to control pain. The study protocol was approved by the Institutional Review Board of our institution (IRB No. 2015-0398).
Grade of peritoneal metastases
The grade of PM was established by colorectal surgeons at the time of surgery. PM was classified according to the classification defined by the Japanese Society for Cancer of the Colon and Rectum (JSCCR) into three subgroups, based on extent; namely: P1, metastases only to adjacent peritoneum; P2, a few metastases to distant peritoneum; and P3, numerous metastases in the distant peritoneum [2, 11].
Operation
First-line treatment regimens were decided by both colorectal surgeons and medical oncologists. The type of surgery was decided by colorectal surgeons based on the severity of the disease, defined by the extent of PM, adjacent organ invasion, and obstruction; and the patient’s general condition, defined by age, performance status, and comorbidity. Most patients with extensive peritoneal metastases (P2 or P3), adjacent organ invasion, an older age (>70 years), or poor performance status with comorbidity underwent palliative surgery, which was classified as PR and NR. PR included resection of the primary tumor without removal of PM lesions, and NR was defined as exploratory laparotomy, stoma construction, and bypass surgery without removal of the primary tumor. PIC or HIPEC was not performed during the study period.
Chemotherapy
Medical oncologists were responsible for deciding on chemotherapy use and regimens. Patients were considered to have undergone palliative chemotherapy if they completed at least two cycles of a course of chemotherapy following surgery. Eligibility criteria included ECOG performance status of 0–2, and age ≤75 years. Chemotherapy regimens were administered in accordance with the NCCN Clinical Practice Guidelines in Oncology (http://www.nccn.org).
Statistical analysis
Continuous variables in the PR and NR groups are expressed as mean ± standard deviation and compared using the t test or Wilcoxon’s rank sum test; categorical variables are expressed as frequencies (percentages) and compared using the Chi-squared or Fisher’s exact test. Overall survival (OS) was calculated by the Kaplan–Meier method and compared by the log-rank test. Potential prognostic variables were assessed using a Cox’s proportional hazard model and backward elimination regression. To assess the correlation between PR and clinical outcomes, and to minimize the impact of treatment selection bias and potential confounding in this observational study, one-to-one propensity‐score matching (PSM) was performed, along with weighted Cox proportional‐hazards regression models, using the inverse‐probability‐of‐treatment weighting (IPTW), to adjust for significant differences in patient characteristics. Propensity scores in the PR and NR groups were estimated by multiple logistic‐regression analysis with all pre-specified covariates. The discrimination and calibration abilities of each propensity-score model were assessed by the C‐statistic and the Hosmer–Lemeshow statistic. All covariates included in the calculations of propensity scores in the two matched groups were compared. Categorical variables were compared by McNemar’s test. The risk of outcomes in the propensity‐score‐matched cohort was compared via a Cox regression model, with robust standard errors that accounted for the clustering of matched pairs. Using the IPTW technique, weights for patients in the PR group were the inverse of the 1‐propensity score, and weights for patients in the NR group were the inverse of the propensity score. All reported P values are two-sided, with P values <0.05 considered significant. All statistical analyses were performed using SAS software version 9.3 (SAS Institute, Inc., Cary, NC, USA).
Results
Patient and tumor characteristics
Table 1 shows the clinicopathological features of the 255 patients with PM-CRC. Among the 170 patients (66.7 %) who presented with symptoms, obstruction (n = 122) was the most frequent, followed by defecation difficulty (n = 63), abdominal pain (n = 53), and others (n = 13). Rates of adjacent organ invasion were significantly lower, PM was less extensive, and rates of palliative chemotherapy were significantly higher in the PR group than in the NR group (P < 0.001–0.02). Table 2 summarizes the operative procedures performed for the 255 patients with PM-CRC.
Chemotherapy regimens
Among the 75 patients who did not receive chemotherapy after palliative surgery, the most frequent reason was patient refusal (n = 44), followed by performance status deterioration (n = 12), no advantage determined by medical oncologists (n = 5), postoperative mortality (n = 3), adverse effects after the first cycle of chemotherapy (n = 1), and prolonged postoperative complications (n = 1). First-line chemotherapy after palliative surgery consisted of irinotecan-containing regimens in 42 patients (33.1 %) and oxaliplatin-containing regimens in 37 (29.1 %), with a median number of 7 (range 2–42) cycles per patient (Table 3). Treatment with anti-vascular endothelial growth factor and anti-epidermal growth factor receptor was more frequent in the PR (n = 8) group than in the NR (n = 1) group (P = 0.002).
Survival and prognostic factors
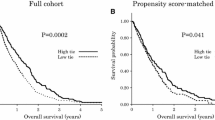
By the end of the study period, 219 patients (85.9 %) had died. The 1-, 3-, and 5-year OS rates in patients with PM-CRC were 62, 20, and 7 %, respectively. Overall median survival was 17 months, but survival was significantly higher in the PR group than in the NR group (23 vs. 11 months, respectively; P < 0.001, Fig. 1). Subgroup analysis showed that median survival was significantly longer for the PR group patients with disease classified as P1 and P3 (P < 0.001 each), but not for those with disease classified as P2 (P = 0.072), than for the NR group patients. Among the variables examined, adjacent organ invasion, more extensive PM (P3), non-resection, and the absence of chemotherapy were independent prognostic factors in the multivariate analysis (P < 0.001–0.006, Table 4).
Because the demographic data differed between the PR and NR groups, PSM was used to match 69 pairs of patients, thus reducing comparison bias. The discrimination and calibration abilities of the propensity-score model were 0.768 by the C-statistic and P = 0.419 by the Hosmer–Lemeshow statistic. The PR group patients had better survival than the NR group patients in Cox multivariate analyses, including PSM [hazard ratio (HR) 0.496, 95 % confidence interval (CI) 0.268–0.919, P = 0.025, Fig. 2] and IPTW (HR 0.344, 95 % CI 0.291–0.406, P < 0.001).
Discussion
Numerous studies of mCRC have compared PR with chemotherapy as the first‐line treatment. Although many symptomatic patients with mCRC require palliative surgery, their surgical outcomes have not been assessed systematically [9, 12]. In patients with unresectable liver metastases, PR showed better survival than NR, using a PSM method [9]. Because the route of metastasis for PM differs from that for hematogenous and lymphatic spread, the treatment and prognosis of patients with PM are different from those of patients with other types of systemic metastases [4, 8]. Compared with patients having unresectable hepatic metastasis in our previous study [9], the patients with PM-CRC in this study had a more aggressive clinical presentation, including frequent symptoms (67 vs. 43 %), obstruction (48 vs. 37 %), colon predilection (83 vs. 58 %), and organ invasion (27 vs. 14 %). Although poorer survival was expected for the patients with PM-CRC than for patients with other types of systemic metastasis, this study showed that palliative primary tumor resection can benefit patients with PM-CRC as well as those with unresectable hepatic mCRC.
The degree of PM in most studies on cytoreductive surgery (CRS) has been evaluated using the peritoneal cancer index (PCI) [8], which integrates peritoneal implant size and the distribution of nodules on the peritoneal surface. Surgeons should identify all seeded nodules throughout 12 abdominal regions and calculate the composite score. Compared with the complexity of PCI, the Japanese classification of PM-CRC is simple and easy to use, even for general surgeons in routine clinical practice. However, the definitions of P1–P3 according to this classification seem subjective and vague [13]. A new version of this system, which includes additional number and size criteria to enhance objectivity [14], is more difficult to use for general surgeons, with drawbacks similar to those for PCI. Although it is difficult to compare the Japanese classification system with the PCI, the P1, P2, and P3 of the former may be approximately equivalent to PCIs of 1–9, 4–18, and 7–39, respectively [15]. The JSCCR guidelines for treating PM indicate that complete resection is desirable for P1 and that complete resection should be considered for P2 when easily resectable; however, the efficacy of resection for P3 has not been determined [16]. Despite the relatively small number of cases in each subgroup, this study found that primary tumor resection had benefits, even in the P3 group, suggesting that an aggressive approach including PR may prolong the survival of selected PM-CRC patients with disease classified as P3. However, it is not easy for the surgeon to decide if palliative resection is appropriate for patients with extensive PM-CRC (P3) in clinical practice. Thus, PR for P3 of PM-CRC should be considered when patient’s overall condition permits an aggressive procedure.
Systemic chemotherapy has only limited efficacy in patients with PM-CRC, owing at least in part to the plasma-peritoneal barrier, which reduces intraperitoneal drug penetration [17]. In contrast to other systemic metastases, multimodality treatment, combining CRS with perioperative intraperitoneal chemotherapy (PIC), may promote the long-term survival of selected patients with PM [6, 7]. However, this aggressive treatment has not been universally adopted for several reasons [15]. First, selected patients with less extensive PM, of PCI ≤10–20 or with isolated and resectable PM, can benefit from this treatment [7, 18]. Second, this approach can be performed in specialized centers, where surgical oncologists are experienced in these procedures and special equipment is available for hyperthermic intraperitoneal chemotherapy (HIPEC). This equipment is available in only a limited number of tertiary centers in Korea, excluding ours; thus, most patients with PM-CRC receive palliative chemotherapy and/or surgery. Third, although recent advances in anesthesiologic and surgical techniques have reduced morbidity and mortality rates [19], more aggressive treatment has been associated with high mortality (0–12 %) and morbidity (21–62 %) rates [17]. In clinical practice, palliative surgery is more available than CRS and PIC.
This study showed that patients who underwent PR had a survival advantage of 12 months over patients in the NR group. Although PM was less extensive and chemotherapy rates were lower in the PR group, the survival difference between the two groups was not eliminated after propensity-score-matched analysis. Tumor debulking and control of symptoms may improve patient responses to chemotherapy, as seen in patients with advanced renal cell and ovarian cancer [20, 21]. Moreover, as CRS is the most aggressive type of debulking surgery, the prolonged survival of patients who underwent CRS may partly explain the survival benefit of primary tumor resection in patients with PM.
The degree of PM is the most important prognostic factor in patients with PM-CRC. Many studies have demonstrated that survival correlated with the degree of PM [2, 7, 22], in agreement with our findings. Surgical procedures for PM-CRC have been based on the degree of PM and have included CRS, debulking, palliative tumor resection, bypass, and stoma formation. Generally, patients with less extensive PM are eligible for a more aggressive surgical approach; a finding also observed in this study. The presence of other solid organ metastases is a poor risk factor and regarded as a contraindication to CRS and PIC [17]. However, a recent study reported that 8 % of patients with mCRC had both hepatic and peritoneal metastases, and that treatment with curative intent resulted in a median survival of up to 36 months in selected patients [23]. Other factors, including tumor differentiation, bowel obstruction, malignant ascites, lymph node dissemination, and small bowel involvement, have been identified as negative prognostic indicators [6, 17, 22, 24].
Our study had several limitations, including its retrospective design. Most notably, the allocations of P1/2/3 might have some elements of bias according to the operating surgeon. In addition, although a PSM method can reduce selection bias, resulting in a situation similar to a randomized controlled trial, our PSM and IPTW models could not eliminate all selection bias. Because ethical reasons make it difficult to prospectively evaluate the actual role of PR, the true benefit of primary tumor resection should be investigated in large prospective randomized trials.
In conclusion, the findings of this study demonstrated that PR appears to result in better OS than NR for patients with PM-CRC, when their overall condition permits an aggressive approach.
References
Kerscher AG, Chua TC, Gasser M, Maeder U, Kunzmann V, Isbert C, et al. Impact of peritoneal carcinomatosis in the disease history of colorectal cancer management: a longitudinal experience of 2406 patients over two decades. Br J Cancer. 2013;108:1432–9.
Kobayashi H, Kotake K, Funahashi K, Hase K, Hirata K, Iiai T, et al. Clinical benefit of surgery for stage IV colorectal cancer with synchronous peritoneal metastasis. J Gastroenterol. 2014;49:646–54.
Jayne DG, Fook S, Loi C, Seow-Choen F. Peritoneal carcinomatosis from colorectal cancer. Br J Surg. 2002;89:1545–50.
Franko J, Shi Q, Goldman CD, Pockaj BA, Nelson GD, Goldberg RM, et al. Treatment of colorectal peritoneal carcinomatosis with systemic chemotherapy: a pooled analysis of north central cancer treatment group phase III trials N9741 and N9841. J Clin Oncol. 2012;30:263–7.
Edge S, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A. AJCC cancer staging manual. 7th ed. New York: Springer; 2010.
Cao C, Yan TD, Black D, Morris DL. A systematic review and meta-analysis of cytoreductive surgery with perioperative intraperitoneal chemotherapy for peritoneal carcinomatosis of colorectal origin. Ann Surg Oncol. 2009;16:2152–65.
Elias D, Gilly F, Boutitie F, Quenet F, Bereder JM, Mansvelt B, et al. Peritoneal colorectal carcinomatosis treated with surgery and perioperative intraperitoneal chemotherapy: retrospective analysis of 523 patients from a multicentric French study. J Clin Oncol. 2010;28:63–8.
Sugarbaker PH. A curative approach to peritoneal carcinomatosis from colorectal cancer. Semin Oncol. 2005;32:S68–73.
Yoon YS, Kim CW, Lim SB, Yu CS, Kim SY, Kim TW, et al. Palliative surgery in patients with unresectable colorectal liver metastases: a propensity score matching analysis. J Surg Oncol. 2014;109:239–44.
Katayama H, Kurokawa Y, Nakamura K, Ito H, Kanemitsu Y, Masuda N, et al. Extended Clavien–Dindo classification of surgical complications: Japan Clinical Oncology Group postoperative complications criteria. Surg Today. 2016;46:668.
Japanese Society for Cancer of the Colon and Rectum. Japanese classification of colorectal carcinoma. 2nd ed. Tokyo: Kanehara; 2009.
Yun HR, Lee WY, Lee WS, Cho YB, Yun SH, Chun HK. The prognostic factors of stage IV colorectal cancer and assessment of proper treatment according to the patient’s status. Int J Colorectal Dis. 2007;22:1301–10.
Kobayashi H, Enomoto M, Higuchi T, Uetake H, Iida S, Ishikawa T, et al. Validation and clinical use of the Japanese classification of colorectal carcinomatosis: benefit of surgical cytoreduction even without hyperthermic intraperitoneal chemotherapy. Dig Surg. 2010;27:473–80.
Kobayashi H, Kotake K, Sugihara K. Enhancing the objectivity of the Japanese classification of peritoneal metastases from colorectal cancer. Jpn J Clin Oncol. 2014;44:898–902.
Adachi T, Hinoi T, Egi H, Shimomura M, Ohdan H. Oxaliplatin and molecular-targeted drug therapies improved the overall survival in colorectal cancer patients with synchronous peritoneal carcinomatosis undergoing incomplete cytoreductive surgery. Surg Today. 2015;45:986–92.
Watanabe T, Itabashi M, Shimada Y, Tanaka S, Ito Y, Ajioka Y, et al. Japanese Society for Cancer of the Colon and Rectum (JSCCR) Guidelines 2014 for treatment of colorectal cancer. Int J Clin Oncol. 2015;20:207–39.
Mirnezami R, Moran BJ, Harvey K, Cecil T, Chandrakumaran K, Carr N, et al. Cytoreductive surgery and intraperitoneal chemotherapy for colorectal peritoneal metastases. World J Gastroenterol. 2014;20:14018–32.
Goere D, Malka D, Tzanis D, Gava V, Boige V, Eveno C, et al. Is there a possibility of a cure in patients with colorectal peritoneal carcinomatosis amenable to complete cytoreductive surgery and intraperitoneal chemotherapy? Ann Surg. 2013;257:1065–71.
Stillwell AP, Buettner PG, Siu SK, Stitz RW, Stevenson AR, Ho YH. Predictors of postoperative mortality, morbidity, and long-term survival after palliative resection in patients with colorectal cancer. Dis Colon Rectum. 2011;54:535–44.
Galizia G, Lieto E, Orditura M, Castellano P, Imperatore V, Pinto M, et al. First-line chemotherapy vs bowel tumor resection plus chemotherapy for patients with unresectable synchronous colorectal hepatic metastases. Arch Surg. 2008;143:352–8 (discussion 8).
Stillwell AP, Buettner PG, Ho YH. Meta-analysis of survival of patients with stage IV colorectal cancer managed with surgical resection versus chemotherapy alone. World J Surg. 2010;34:797–807.
Glehen O, Kwiatkowski F, Sugarbaker PH, Elias D, Levine EA, De Simone M, et al. Cytoreductive surgery combined with perioperative intraperitoneal chemotherapy for the management of peritoneal carcinomatosis from colorectal cancer: a multi-institutional study. J Clin Oncol. 2004;22:3284–92.
Thomassen I, van Gestel YR, Lemmens VE, de Hingh IH. Incidence, prognosis, and treatment options for patients with synchronous peritoneal carcinomatosis and liver metastases from colorectal origin. Dis Colon Rectum. 2013;56:1373–80.
Ozawa H, Kotake K, Kobayashi H, Sugihara K. Prognostic factors for peritoneal carcinomatosis originating from colorectal cancer: an analysis of 921 patients from a multi-institutional database. Surg Today. 2014;44:1643–50.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
Seon Jeong Jeong and her coauthors have no conflicts of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Jeong, S.J., Yoon, Y.S., Lee, J.B. et al. Palliative surgery for colorectal cancer with peritoneal metastasis: a propensity-score matching analysis. Surg Today 47, 159–165 (2017). https://doi.org/10.1007/s00595-016-1402-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-016-1402-9