Abstract
Purpose
Laparoscopic sleeve gastrectomy (SG) and gastric banding (GB) are popular bariatric procedures for treating morbid obesity. This study aimed to investigate changes in the hypothalamic feeding center after these surgeries in a diet-induced obese rat model.
Methods
Obesity was induced in 60 Sprague–Dawley rats using a high-energy diet for 6 weeks. These rats were divided into four groups: the sham-operated (SO) control, pair-fed (PF) control, SG and GB groups. Six weeks after the surgery, metabolic parameters, the plasma levels of leptin, ghrelin, peptide YY (PYY) and glucagon-like peptide-1 (GLP-1) and the hypothalamic mRNA expressions of neuropeptide Y (NPY) and pro-opiomelanocortin (POMC) were measured.
Results
Compared with those observed in the SO group, the body and fat tissue weights were significantly decreased and the metabolic parameters were significantly improved in the PF, SG and GB groups 6 weeks after surgery. The plasma ghrelin levels were significantly lower and the PYY and GLP-1 levels were significantly higher in the SG group than in the PF, GB and SO groups. Compared with that seen in the PF and GB groups, the hypothalamic mRNA expression of NPY was significantly lower and the expression of POMC was significantly higher in the SG group.
Conclusions
SG may affect the neurological pathway associated with appetite in the hypothalamus and thereby control ingestive behavior.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bariatric surgery is the most effective long-term treatment for morbid obesity and leads to both durable weight loss and significant improvements in comorbidities. Laparoscopic sleeve gastrectomy (SG) is a typical restrictive bariatric procedure that has been proven to be effective in treating morbid obesity in the clinical setting [1, 2]. This procedure causes rapid and extensive weight loss by decreasing the gastric volume and ghrelin level, shortening the gastrointestinal transit time and improving glucose metabolism [3]. Recently, we reported a high gastric emptying rate and improved glucose metabolism following SG in an obese diabetic rat model [4]. In addition, we also reported that SG improves lipid metabolism in this model [5].
Neuropeptide Y (NPY) is a peptide neurotransmitter that is ubiquitously synthesized in several areas of the brain. However, within the arcuate nucleus (ARC) of the hypothalamus, one group of NPY neurons containing leptin receptors is under the control of the local leptin levels. These NPY neurons project to the paraventricular nucleus (PVN) of the hypothalamus where NPY is released. Reduced leptin signaling activates these ARC neurons to synthesize and release NPY into the PVN, and increased NPY in the PVN promotes increased food intake, body weight gain and reduced energy expenditures [6]. Melanocortins constitute a family of peptides that include the adrenocorticotropic hormone and alpha-melanocyte-stimulating hormone (alpha-MSH). Melanocortins are peptides cleaved from the pro-opiomelanocortin (POMC) precursor molecule and exert their effects by binding to members of the melanocortin receptor family. Within the hypothalamus, some melanocortins, including alpha-MSH, have effects on energy homeostasis that are opposite to those of NPY [6]. POMC neurons are stimulated by leptin and reduce food intake.
Ghrelin is a hormone produced primarily by the gastric fundus and is related to appetite stimulation [7]. The intracerebroventricular injection of ghrelin strongly stimulates feeding in rats and increases body weight gain in these animals [8]. Ghrelin signals from the stomach transmit to the nucleus of the solitary tract at the medulla oblongata, finally leading to the increased secretion of NPY/agouti-related protein (AGRP) from the hypothalamus and inhibition of POMC [9]. Peptide YY (PYY) and glucagon-like peptide-1 (GLP-1) are postprandial hormones released by distal gut enteroendocrine L cells. Mechanistic studies have proposed that PYY may exert its anorectic effect by targeting neuropeptide Y2 receptors in the ARC of the hypothalamus, thereby decreasing the expression of NPY mRNA in NPY/AGNR neurons and increasing the expression of POMC mRNA [10]. GLP-1 is also a neurotransmitter involved in the brain stem hypothalamus pathway signaling satiety. GLP-1 stimulates POMC neurons directly and is suggested to indirectly inhibit ARC-NPY neurons [11].
Romanova et al. evaluated the neurobiological changes in the rat hypothalamus associated with weight loss after Roux-en Y gastric bypass (RYGB) using immunohistochemical quantification [12]. Diet-induced obese rats after RYGB demonstrate changes in the hypothalamic downregulation of NPY and upregulation of alpha-MSH. However, the authors did not investigate metabolic or hormonal changes in the blood. Therefore, it is unclear whether SG and gastric banding (GB) surgeries have an effect on the levels of gastrointestinal hormones or expression of NPY and POMC. The aim of the present study was to evaluate the changes in gastrointestinal hormones and hypothalamic expression of NPY and POMC after these procedures.
Materials and methods
Animals
Sixty male Sprague–Dawley rats (3 weeks of age, weight: 55–60 g) were obtained from Charles River Japan, Inc. (Saga, Japan) and housed in individual cages. After acclimation, all rats were fed a high-fat diet containing 60 % calories as fat (Research Diet D12492; Research Diets Inc. New Brunswick, NJ, USA) and tap water (24 ± 2 °C) and were maintained at 50 ± 10 % humidity with a 12-h light cycle (7:00 am to 7:00 pm) for 6 weeks. This study was approved by the Animal Committee of Oita University (Oita, Japan) and conformed to the Guidelines for Animal Experimentation of Oita University.
Surgical procedure
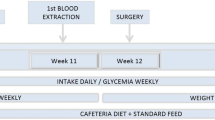
Rats weighing 325–375 g were divided into four groups (n = 15/group): the sham-operated (SO) control group, pair-fed (PF) control group, SG group and GB group. The rats were fasted for 24 h before surgery, and the surgical procedures were performed under anesthesia (4 % sevoflurane; Maruishi Pharmaceutical Co., Osaka, Japan). SG was performed as previously described [4, 13]. In brief, the greater curvature from the antrum to the fundus across the forestomach and glandular stomach was incised and approximately 90 % of the forestomach and 70 % of the glandular stomach were removed. The incision line in the stomach was then closed using polydioxanone sutures (5–0 PDS®; Ethicon, Tokyo, Japan) in three layers. The method for performing GB has been described previously [14, 15]. In brief, a 5-mm incision was made on the midline between the upper and lower portions of the stomach, and the incision lines were closed using 5-0 PDS®. Then, a gastric band made of nylon (Insulok; Hellermann Tyton, Tokyo, Japan) was tied around the suture line. The SO control rats underwent laparotomy, and their stomachs were elevated and returned to the abdominal cavity. The PF control rats consumed a high-fat diet after laparotomy. Body weight and food intake were measured (Animal Scale; Clare, Tokyo, Japan) weekly in all groups (at 10:00 am). The amount of food in the PF group was yoked ad lib to the weekly intake observed in the SG and GB groups, as previously described [16]. Indeed, the mean amount of food intake among the surgery groups was given to the PF group.
Measurement of fat tissue weight from the retroperitoneum
Fat tissue samples of the retroperitoneum around the kidneys were collected 6 weeks after surgery, as previously described [17], and their weights were measured in each of the four groups.
Biochemical tests
Blood samples were collected 6 weeks after surgery. The blood glucose data were evaluated using a commercial test kit (Accu-Chek; Sanko Junyaku Co. Ltd., Tokyo, Japan). The total cholesterol, triglyceride (TG) and free fatty acid (FFA) levels were estimated using an H7180 automatic biochemical analyzer (Hitachi, Tokyo, Japan). Enzyme-linked immunosorbent assay (ELISA) kits were used to evaluate the plasma levels of insulin (rat insulin ELISA kit; Shibayagi, Gunma, Japan), leptin (rat leptin ELISA kit; Wako Pure Chemical Industries, Osaka, Japan), active ghrelin (active ghrelin ELISA kit; Mitsubishi Chemical Medience, Tokyo, Japan), PYY (mouse/rat PYY ELISA kit; Wako Pure Chemical Industries, Osaka, Japan) and GLP-1 (rat GLP-1 ELISA kit; Shibayagi, Gunma, Japan). To evaluate insulin resistance, the homeostasis model assessment ratio (HOMA-R) was calculated based on the following formula: HOMA-R = fasting glucose (mmol/l) × fasting insulin (μU/ml)/22.5 [18].
Quantitative real-time polymerase chain reaction (PCR) for the mRNA expression of NPY and POMC in the hypothalamus
Each rat was decapitated, and sections containing the hypothalamus were then cut according to the rat brain atlas of Paxinos and Watson [19, 20] and immediately frozen in liquid nitrogen. Total RNA isolation was performed as previously described [21]. Quantitative real-time PCR was performed as previously described [21] with a LightCycler system (Roche Diagnostics, Lewes, East Sussex, UK). The following primers were used: NPY: 5′-CCGCTCTGCGACACTACAT-3′ (forward) and 5′-TGTCTCAGGGCTGGATCTCT-3′ (reverse) (Nihon Gene Research Laboratories, Sendai, Japan), and POMC: 5′-AGGACCTCACCACGGAAAG-3′ (forward) and 5′-CCGAGAGGTCGAGTCTGC-3′ (reverse) (Nihon Gene Research Laboratories). The data were analyzed using the LightCycler analysis software program (Roche), and a standard curve that correlated the cycle number with the amount of formed products was plotted for each sequence of interest. The mRNA expression levels of NPY and POMC were then normalized to those of rat glyceraldehyde-3-phosphate dehydrogenase (GAPDH).
Statistical analysis
All data are expressed as the mean ± standard deviation and were evaluated using a one-way analysis of variance with Bonferroni correction for multiple comparisons. A P value of <0.05 was considered to be statistically significant. The statistical analyses were performed using the Statistical Package for Social Sciences (SPSS) Ver. 21 software package (IBM Corp. Armonk, NY, USA).
Results
Changes in body weight, food intake and fat tissue weight
The body weights were significantly lower after surgery in the PF, SG and GB groups than in the SO group; however, there were no significant differences in weight between the PF, SG and GB groups (Fig. 1a). The weekly food intake in the PF, SG and GB groups was significantly decreased compared with that observed in the SO group after surgery (Fig. 1b). The weight of fat tissue from the retroperitoneum 6 weeks after surgery was significantly lower in the PF, SG and GB groups than in the SO group, and there were no significant differences in this parameter between the PF, SG and GB groups (Fig. 1c).
Changes in body weight, food intake and fat tissue weight. a Changes in body weight after surgery in the sham-operated (SO), pair-fed (PF), sleeve gastrectomy (SG) and gastric banding (GB) groups. Each group consisted of 15 rats. *P < 0.01 versus the SO group. b Weekly food intake after surgery in the SO, PF, SG and GB groups. Each group consisted of 15 rats. *P < 0.01 versus the SO group. c Weight of fat tissue from the retroperitoneum in the SO, PF, SG and GB groups. Each group consisted of 15 rats. *P < 0.01
Changes in metabolic parameters and hormones
The mean plasma levels of glucose, TC, TG, FFA and insulin and HOMA-R 6 weeks after surgery are shown in Table 1. The levels of glucose, TC, TG, FFA and insulin and HOMA-R were significantly lower in the PF, SG and GB groups than in the SO group, although there were no significant differences between the PF, SG and GB groups.
The plasma leptin levels were significantly lower in the PF, SG and GB groups than in the SO group, similar to the results for the other metabolic parameters (Table 1). However, the plasma ghrelin levels were significantly lower in the SG group than in the PF, GB and SO groups. In addition, the plasma PYY and GLP-1 levels were significantly higher in the SG group than in the other three groups.
mRNA expression levels of NPY and POMC in the hypothalamus
The mRNA expression levels of NPY in the hypothalamus were significantly lower in the SG group than in the PF and GB groups (Fig. 2), while the mRNA expression levels of POMC were significantly higher in the SG group than in the PF and GB groups (Fig. 3).
The mRNA expression of neuropeptide Y (NPY) in the hypothalamus was quantified using real-time polymerase chain reaction (PCR) and expressed as the ratio to that of glyceraldehyde-3-phosphate dehydrogenase (GAPDH). SO sham operated, PF pair fed, SG sleeve gastrectomy, GB gastric banding. *P < 0.01, **P < 0.05
The mRNA expression of pro-opiomelanocortin (POMC) in the hypothalamus was quantified using real-time polymerase chain reaction (PCR) and expressed as the ratio to that of glyceraldehyde-3-phosphate dehydrogenase (GAPDH). SO sham operated, PF pair fed, SG sleeve gastrectomy, GB gastric banding. Each group consisted of 10 rats. *P < 0.01
Discussion
A significant number of patients have been recognized as being morbidly obese in national epidemiologic studies. These patients have comorbidities, such as type 2 diabetes and heart disease, which can lead to premature death. Some surgical procedures, including SG and GB, may reduce these comorbidities and risk factors. The use of laparoscopic SG has rapidly increased worldwide, and several studies have reported its long-term effects. For example, Himpens et al. reported a percent excess weight loss (%EWL) 6 years after laparoscopic SG of 57.3 % [22], and Bohdjalian et al. reported a %EWL 5 years after laparoscopic SG of 55.0 % [23]. The morbidity of laparoscopic SG has been reported to be 3.2–7.3 %, with a mortality rate of 0–0.7 % [24–26]. The SG procedure reduces the size of the gastric reservoir and decreases lipid absorption, thus contributing to weight loss. Surgical intervention using the banding system has also been shown to be an effective method for sustaining significant weight loss for the majority of severely obese subjects [1]. However, the effects of SG and GB on the CNS and their roles in weight loss have not been previously described.
Body fat is regulated by a complex neuroendocrine system, making it difficult to maintain weight loss achieved through caloric restriction. A key component of this regulatory system is the adipocyte hormone leptin [27]. In the present study, the plasma leptin levels were significantly lower in the PF, SG and GB groups than in the SO group. In most obese patients, the leptin levels are elevated in direct proportion to the amount of body fat; similar findings were observed in our study, in which the fat tissue weight corresponded to the leptin level. Exogenous leptin treatment produces little or no weight loss [28]. The failure of leptin to produce the same effect in obese individuals as in lean individuals is believed to be due to leptin resistance [27]. In our previous studies, we used Zucker diabetic fatty rats that contained a mutation in the leptin receptor and demonstrated tolerance to leptin. It is likely not adequate to investigate the expression in the hypothalamic feeding center to avoid the low sensitivity of leptin, and we therefore used a high-fat diet-induced obese rat model in the current study. In this study, the SG and GB procedures reduced the fat mass and consequently decreased the plasma leptin levels.
The ghrelin levels were significantly lower in the SG group than in the other three groups in this study. A marked reduction in the ghrelin levels has been reported after SG in both clinical and experimental studies [29, 30]. In the present study, the plasma PYY and GLP-1 levels were significantly higher in the SG group than in the PF, GB and SO groups. In a previous clinical study, SG increased the plasma levels of PYY and GLP-1. Similarly, Peterli et al. described that the blood GLP-1 and PYY levels are increased after SG in humans [31]. In our previous animal studies, we demonstrated higher gastric emptying and greater small bowel transit in the SG group than in the GB and SO groups [4, 5]. In another clinical study, Shah et al. reported that the small bowel transit time and gastric emptying half-time were shortened after SG [3]. SG may activate PYY and GLP-1 secretion as a result of the shorter small bowel transit time of food.
Satiety hormones influence a feedback mechanism that controls energy intake via the receptors in the ARC of the hypothalamus. These receptors are situated on anabolic NPY/AGRP and catabolic POMC neurons; the anabolic neurons are stimulated by ghrelin and suppressed by leptin and insulin [32]. These phenomena explain the appetite-stimulant effect of ghrelin and the satiety-inducing properties of leptin [9]. In addition, putative direct PYY and indirect ghrelin target POMC neurons in the ARC. PYY, which may induce an overall negative energy balance, has been shown to have high affinity for Y2 receptors, which are expressed on both NPY/AGRP and POMC neurons and induce a reduced food intake [10]. GLP-1 directly stimulates POMC/cocaine- and amphetamine-regulated transcript neurons and indirectly inhibits neurotransmissions in neurons expressing NPY via GABA-dependent signaling [11].
In the present study, the mRNA expression of NPY in the hypothalamus was significantly lower in the SG group than in the PF and GB groups, whereas there were no differences between the SG and SO groups. In addition, the mRNA expression of POMC in the hypothalamus was significantly higher in the SG group than in the PF and GB groups, and there were no differences between the SG and SO groups. These differences in the mRNA expression between the SG, GB and PF groups are likely associated with the differences in the ghrelin, PYY and GLP-1 levels. Furthermore, the decrease in the NPY levels and increase in the POMC levels in the SO group may have been influenced by the elevated leptin levels. Furthermore, in the SG group, the decreased ghrelin levels may have directly suppressed the NPY activity and indirectly stimulated the POMC activity (Fig. 4). In addition, the increased PYY and GLP-1 levels may have directly activated POMC.
Ferreira et al. reported that the overexpression of NPY in the ARC induces sustained body weight gain and severe fat accumulation, whereas the downregulation of NPY does not affect body weight gain [33]. NPY-overexpression rats show a marked increase in the insulin and leptin levels. Moreover, Zhan et al. examined the behavioral functions of POMC neurons in the ARC using pharmacogenetic approaches [34]. In that study, the chronic activation of POMC neurons reduced food intake, and ablating these neurons resulted in hyperphasia, obesity and metabolism disorders. Additionally, ablating POMC neurons significantly reduced the plasma corticosterone levels, demonstrating the possibility of a feedback mechanism.
The current study had two control groups: the SO and PF groups. A comparison of the surgery and two control groups clearly demonstrated different effects of the surgeries on the gastrointestinal hormones and hypothalamic feeding center. A preliminarily examination of the expression of NPY and POMC just before surgery indicated that the expression levels were the same as those observed in the SO group. Therefore, we consider that SO rats may show normal expression levels of NPY and POMC, based on our findings. Many experimental studies have demonstrated that food intake in animals is decreased just after surgery and that appetite loss is temporary. The central mechanisms involved in the acute stress-induced inhibition of energy intake have not been fully investigated; however, certain peptides and neurotransmitters are believed to be involved in the response. It is generally accepted that the corticotropin-releasing factor (CRF) is responsible for initiating and coordinating the responses to stress [35], and an elevated CRF level in response to stress in the CNS decreases food intake [36]. In addition, the overexpression CRF may reduce the expression of NPY in the hypothalamus [37]. Therefore, the decreased food intake noted 1 week after surgery in the SG and GB groups in this study may be related to temporary changes in the feeding center.
Previously, in a clinical crossover study, Dixon et al. reported that laparoscopic adjustable GB prolonged satiety under conditions of optimal restriction [38]. They also evaluated changes in the blood glucose, insulin, ghrelin and leptin levels, although they found no relationships between the changes and the satiating effect. In the present study, upregulation of NPY and downregulation of POMC were observed in the GB group; however, the prolonged satiety detected after GB could not be explained. Considering that there were no differences in weight loss, food intake or the fat tissue weight between the SG and GB groups, the mechanisms inducing increased satiety may be related to different neurological pathways for appetite.
This manuscript first demonstrated changes in the hypothalamic feeding center after SG and GB. In addition, this study is the first to show the relationships between changes in the hypothalamic feeding center and the levels of gastrointestinal hormones after SG (Fig. 4). Therefore, bariatric surgeries, such as SG, may influence the hypothalamic feeding center and change ingestive behavior. However, this study used a rodent model, which differs from humans. Therefore, our results have limitations when applying the findings to the human neuron system, and further clinical studies are needed to investigate the relationship between these bariatric procedures and the neurological pathways in the hypothalamus.
In conclusion, SG may affect the neurological pathway of appetite in the hypothalamus and control ingestive behavior.
References
Gagner M, Deitel M, Kalberer TL, Erickson AL, Crosby RD. The Second International Consensus Summit for Sleeve Gastrectomy, March 19-21, 2009. Surg Obes Relat Dis. 2009;5:476–85.
Gill RS, Birch DW, Shi X, Sharma AM, Karmali S. Sleeve gastrectomy and type 2 diabetes mellitus: a systematic review. Surg Obes Relat Dis. 2010;6:707–13.
Shah S, Shah P, Todkar J, Gagner M, Sonar S, Solav S. Prospective controlled study of effect of laparoscopic sleeve gastrectomy on small bowel transit time and gastric emptying half-time in morbidly obese patients with type 2 diabetes mellitus. Surg Obes Relat Dis. 2010;6:152–7.
Masuda T, Ohta M, Hirashita T, Kawano Y, Eguchi H, Yada K, et al. A comparative study of gastric banding and sleeve gastrectomy in an obese diabetic rat model. Obes Surg. 2011;21:1774–80.
Kawano Y, Ohta M, Hirashita T, Masuda T, Inomata M, Kitano S. Effects of sleeve gastrectomy on lipid metabolism in an obese diabetic rat model. Obes Surg. 2013;23:1947–56.
Woods SC, Schwartz MW, Baskin DG, Seeley RJ. Food intake and the regulation of body weight. Annu Rev Psychol. 2000;51:255–77.
Takiguchi S, Murakami K, Yanagimoto Y, Tanaka A, Miyazaki Y, Mori M, et al. Clinical application of ghrelin in the field of surgery. Surg Today. 2014. doi:10.1007/s00595-014-1040-z.
Nakazato M, Murakami M, Date Y, Kojima M, Matsuo H, Kangawa K, et al. A role for ghrelin in the center regulation of feeding. Nature. 2001;409:194–8.
Frezza EE. Hormonal control of diabetes type 2 after surgery: clinical and experimental evaluation. Asian J Endosc Surg. 2009;2:1–7.
Pfluger PT, Castaneda TR, Heppner KM, Strassburg S, Kruthaupt T, Chaudhary N, et al. Ghrelin, peptide YY and their hypothalamic targets differentially regulate spontaneous physical activity. Physiol Behav. 2011;105:52–61.
Secher A, Jelsing J, Baquero A, Hecksher-Sorensen J, Cowley M, Daiboge L, et al. The arcuate nucleus mediates GLP-1 receptor agonist liraglutide-dependent weight loss. J Clin Invest. 2014;124:4473–88.
Romanova IV, Ramos EJ, Xu Y, Quinn R, Chen C, George ZM, et al. Neurobiologic changes in the hypothalamus associated with weight loss after gastric bypass. J Am Coll Surg. 2004;199:887–95.
Lopez PP, Nicholson SE, Burkhardt GE, Johnson RA, Johnson FK. Development of a sleeve gastrectomy weight loss model in obese Zucker rats. J Surg Res. 2009;157:243–50.
Endo Y, Ohta M, Kai S, Kitano S. An obese rat model of bariatric surgery with gastric banding. Obes Surg. 2007;17:815–9.
Hirashita T, Ohta M, Endo Y, Masuda T, Iwashita Y, Kitano S. Effects of visceral fat resection and gastric banding in an obese diabetic rat model. Surgery. 2012;151:6–12.
Chambers A, Jesen L, Ryan K, Sisley S, Wilson-Perez H, Stefater M, et al. Weight-independent changes in blood glucose homeostasis after gastric bypass or vertical sleeve gastrectomy in rats. Gastroenterology. 2011;141:950–8.
Masaki T, Chiba S, Yasuda T, Tsubone T, Kakuma T, Shimomura I, et al. Peripheral, but not central, administration of adiponectin reduces visceral adiposity and upregulates the expression of uncoupling protein in agouti yellow (Ay/a) obese mice. Diabetes. 2003;52:2266–73.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9.
Gotoh K, Masaki T, Chiba S, Ando H, Shimasaki T, Mitsutomi K, et al. Nesfatin-1, corticotropin-releasing hormone, thyrotropin-releasing hormone, and neuronal histamine interact in the hypothalamus to regulate feeding behavior. J Neurochem. 2013;124:90–9.
Paxinos G, Watson C. The Rat Brain in Stereotaxic Coordinates. 7th ed. New York: Academic Press; 2013.
Tominaga M, Ohta M, Kai S, Iwaki K, Shibata K, Kitano S. Increased heat-shock protein 90 expression contributes to impaired adaptive cytoprotection in the gastric mucosa of portal hypertensive rats. J Gastroenterol Hepatol. 2009;24:1136–41.
Himpens J, Dobbeleir J, Peeters G. Long-term results of laparoscopic sleeve gastrectomy for obesity. Ann Surg. 2010;252:319–24.
Bohdjalian A, Langer FB, Shakeri-Leidenmuhler S, Gfrerer L, Ludvik B, Zacherl J, et al. Sleeve gastrectomy as sole and definitive bariatric procedure: 5-year results for weight loss and ghrelin. Obes Surg. 2010;20:535–40.
Bellanger DE, Greenway FL. Laparoscopic sleeve gastrectomy, 529 cases without a leak: short-term results and technical considerations. Obes Surg. 2011;21:146–50.
Menenakos E, Stamou KM, Albanopoulos K, Papailiou J, Theodorou D, Leandros E. Laparoscopic sleeve gastrectomy performed with intent to treat morbid obesity: a prospective single-center study of 261 patients with a median follow-up of 1 year. Obes Surg. 2010;20:276–82.
Mittermair R, Sucher R, Perathoner A. Results and complication after laparoscopic sleeve gastrectomy. Surg Today. 2014;44:1307–12.
Stefater MA, Perez-Tilve D, Chambers AP, Wilson-Perez HE, Sandoval DA, Berger J, et al. Sleeve gastrectomy induces loss of weight and fat mass in obese rats, but does not affect leptin sensitivity. Gastroenterology. 2010;138:2426–36.
Scarpace PJ, Matheny M, Tumer N. Hypothalamic leptin resistance is associated with impaired leptin signal transduction in aged obese rats. Neuroscience. 2001;104:1111–7.
Karamanakos SN, Vagenas K, Kalfarentzos F, Alexandrides TK. Weight loss, appetite suppression, and changes in fasting and postprandial ghrelin and peptide-YY levels after Roux-en-Y gastric bypass and sleeve gastrectomy: a prospective, double blind study. Ann Surg. 2008;247:401–7.
Wang Y, Liu J. Plasma ghrelin modulation in gastric band operation and sleeve gastrectomy. Obes Surg. 2009;19:357–62.
Peterli R, Wolnerhanssen B, Peters T, Devaux N, Kern B, Christoffel-Courtin C, et al. Improvement in glucose metabolism after bariatric surgery: comparison of laparoscopic Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy: a prospective randomized trial. Ann Surg. 2009;250:234–41.
Nijhuis J, van Dielen FM, Buurman WA, Greve JW. Ghrelin, leptin and insulin levels after restrictive surgery: a 2-year follow-up study. Obes Surg. 2004;14:783–7.
Ferreira L, Garrido M, Ferreira I, Nobrega C, Carvalho A, Alvaro A, et al. Moderate long-term modulation of neuropeptide Y in hypothalamic arcuate nucleus induces energy balance alterations in adult rats. PLoS One. 2011;6:e22333.
Zhan C, Zhou J, Feng Q, Zhang J, Lin S, Bao J, et al. Acute long-term suppression of feeding behavior by POMC neurons in the brainstem and hypothalamus, respectively. J Neurosci. 2013;33:3624–32.
Koob G, Heinrichs S, Pich E, Menzaghi F, Baldwin H, Miczek K, et al. The role of corticotropin-releasing factor in behavioural responses to stress. Ciba Found Symp. 1993;172:277–89.
Makino S, Smith MA, Gold PW. Increased expression of corticotropin-releasing hormone and vasopressin messenger ribonucleic acid (mRNA) in the hypothalamic paraventricular nucleus during repeated stress: association with reduction in glucocorticoid receptor mRNA levels. Endocrinology. 1995;136:3299–309.
Heinrichs SC, Menzaghi F, Pich EM, Hauger RL, Kob GF. Corticotropin-releasing factor in the paraventricular nucleus modulates feeding induced by neuropeptide Y. Brain Res. 1993;611:18–24.
Dixon AF, Dixon JB, O’Brien PE. Laparoscopic adjustable gastric banding induces prolonged satiety: a randomized blind crossover study. J Clin Endocrinol Metab. 2005;90:813–9.
Acknowledgments
We thank Ms. Yuiko Aso for her expert technical assistance.
Conflict of interest
The authors declare that they have no conflicts of interest and that no sources of funding or material support were provided for this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kawasaki, T., Ohta, M., Kawano, Y. et al. Effects of sleeve gastrectomy and gastric banding on the hypothalamic feeding center in an obese rat model. Surg Today 45, 1560–1566 (2015). https://doi.org/10.1007/s00595-015-1135-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-015-1135-1