Abstract
Aim
To identify the potential metabolite markers in diabetic retinopathy (DR) by using gas chromatography coupled with time-of-flight mass spectrometry (GC-TOFMS).
Methods
GC-TOFMS spectra were acquired from vitreous and aqueous humor (AH) samples of patients with DR and non-diabetic participants. Comparative analysis was used to elucidate the distinct metabolites of DR. Metabolic pathway was employed to explicate the metabolic reprogramming pathways involved in DR. Logistic regression and receiver-operating characteristic analyses were carried out to select and validate the biomarker metabolites and establish a therapeutic model.
Results
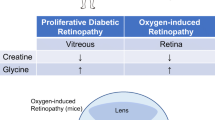
Comparative analysis showed a clear separation between disease and control groups. Eight differentiating metabolites from AH and 15 differentiating metabolites from vitreous were highlighted. Out of these 23 metabolites, 11 novel metabolites have not been detected previously. Pathway analysis identified nine pathways (three in AH and six in vitreous) as the major disturbed pathways associated with DR. The abnormal of gluconeogenesis, ascorbate–aldarate metabolism, valine–leucine–isoleucine biosynthesis, and arginine–proline metabolism might weigh the most in the development of DR. The AUC of the logistic regression model established by d-2,3-Dihydroxypropanoic acid, isocitric acid, fructose 6-phosphate, and l-Lactic acid in AH was 0.965. The AUC established by pyroglutamic acid and pyruvic acid in vitreous was 0.951.
Conclusions
These findings have expanded our understanding of identified metabolites and revealed for the first time some novel metabolites in DR. These results may provide useful information to explore the mechanism and may eventually allow the development of metabolic biomarkers for prognosis and novel therapeutic strategies for the management of DR.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Epidemiological survey showed that the estimated standardized prevalence of total diagnosed diabetes in China reached to 10.9% in 2013 [1]. The prevalence of diabetic retinopathy (DR) in Chinese type 2 diabetes mellitus increased to 25% according to a meta-analysis published in 2019 [2]. DR is considered to be the major cause of blindness among middle-aged adults and has caused increased health and economic burden [3]. Rigid control of hyperglycemia is thought to effectively prevent the development/progression of DR [4, 5]; however, the incidence of DR is increasing despite implementation of proper glycemic control [6, 7]. Early exposure to hyperglycemia predisposes diabetics to the development of DR. One possible reason for this is that transient exposure to hyperglycemia can induce the development of persistent epigenetic changes [8, 9], referred to as modifications of chromatin structure and gene expression to metabolic characteristics (metabolic memory theory) [10], which eventually results in the development of DR [11]. Thus, we require a better understanding of this pathway to enable better management of DR. For this pathway, the metabolites are the downstream products of gene transcription and translation. Given this, the use of metabolomics is considered to provide a more sensitive and dynamic approach for elucidating the pathophysiological mechanisms and identifying disease biomarkers that can eventually be applied for the development of clinical interventions [12,13,14].
In metabolomics, mass spectrometry (MS) is the most frequently employed technology. Of the gas chromatography (GC) separation techniques, gas chromatography time-of-flight mass spectrometry (GC-TOFMS) yields higher sensitivity, selectivity, separation capacity, and accuracy of metabolite detection and is well suited for the identification and quantitation of small molecular weight metabolites [15,16,17]. Therefore, in our study, a GC-TOFMS technology-based nontargeted metabolomics approach combined with multivariate statistical analysis was validated to profile patients diagnosed with DR, and non-diabetic patients to explore mechanisms underlying DR, to discover potential metabolite biomarkers for DR, and to develop pharmacologic approaches to combat pathological change in DR.
Serum metabolomics has been mainly used to explore metabolic signatures associated with diabetes [18,19,20]. We postulate that a distinct metabolic signature for DR exists, and this signature can be resolved from that of diabetes alone. Vitreous samples have been examined for DR, but there are only a few studies until now and the repeatability is low. Currently, there is also limited knowledge about aqueous humor (AH) metabolomics in the context of DR. AH serves as the main fluid that fills the anterior chamber and supplies nutrients. The breakdown of AH homeostasis might play a major role in the formation of iris neovascularization (INV) in DR. Metabolic analysis of AH may supply some valuable information. Therefore, we designed the metabolic profile analysis of human vitreous and AH taken from diabetes-free patients and diabetic patients with DR.
Methods
Research design
The study was prospectively approved by the Ethics Committee of Shanghai First People’s Hospital of Shanghai Jiaotong University, and research was conducted in accordance with the Declaration of Helsinki. Signed informed consent was obtained from all participants before the procedures. We conducted this prospective, observational, and registration study from February 2017 to February 2018 at Shanghai First People’s Hospital Ophthalmologic Center.
Diabetes was defined as self-report of a previous diagnosis, a fasting blood glucose of 7.0 mmol/L or higher, or HbA1c level of 6.5% (48 mmol/mol) or higher on two separate tests. Chronic kidney disease (CKD) was defined as self-report of the previous diagnosis. All participants were screened based on unified diagnostic standard guidelines or the consensus of Chinese Ocular Fundus Disease Society. The inclusion criteria for disease group were patients with confirmed diagnosis of type 2 diabetes and proliferative diabetic retinopathy (PDR). The inclusion criteria for control group included participants without type 2 diabetes. Participants were excluded if they had a history of intravitreal injection of any anti-VEGF drugs (vascular endothelial growth factor, VEGF), the previous ocular surgeries or other ocular diseases. Participants who had diffuse vitreous hemorrhage were also excluded. All participants’ data including sex, age, body mass index (BMI), vital signs, medical history, concomitant medications, and biochemical variables such as low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), and triacylglycerol (TAG) were recorded and filed in the electronic case report form.
Vitreous samples were collected from 28 patients with type 2 diabetes with PDR and 22 non-diabetic patients with macular hole (MH). For the AH samples, the disease subjects were 23 participants with type 2 diabetes with PDR. Control subjects were 25 non-diabetic patients with cataract.
Sample preparation and mass spectrometry analysis
For the vitreous sample collection, participants underwent standard pars plana vitrectomy with a 25-gauge 3-port system. We mainly cut the vitreous where there was no diffuse hemorrhage. We also set the cut rates to 2500 cuts per min (cpm) and the aspiration flow to maximum 350 mmHg in order to avoid the aspiration of hemorrhage. For the aqueous humor sample collection, participants underwent paracentesis of anterior chamber. Sample aliquots of 0.15 mL were transferred into cryovial tubes and immediately stored at − 80 °C. An Agilent 6890N gas chromatography coupled with a Pegasus HT TOF MS (LECO Corp., St. Joseph, MI, USA) was used as the GC-TOFMS platform. The sample preparation procedures and instrumental analysis are referred in the previously published methods [21] with minor modifications and are summarized in the Supplementary Materials.
Statistical and data analysis
The raw data generated by GC-TOFMS were processed using XploreMET for automated baseline denoising and smoothing, peak picking and deconvolution, creating reference database from the pooled QC samples, metabolite signal alignment, missing value correction and imputation, and QC correction. Metabolites in the study samples were annotated with self-built mammalian metabolite database JiaLib™ using both retention times and fragmentation patterns in the mass spectrum.
Results are expressed as the mean ± SD for continuous variables. Principal component analysis (PCA) and orthogonal projection to latent structure-discriminant analysis (OPLS-DA) were performed in our study using SIMCA-P version 14.0 (Umetrics AB, Umea, Sweden). In addition to the multivariate statistical method, the Mann–Whitney U test and fold change were also applied to measure the significance of each metabolite. The resultant p values for each metabolite in all cross-comparisons were corrected by Bonferroni correction. The p values across all metabolites within each comparison were adjusted to account for multiple testing by a false discovery rate method. Pathway analysis and spearman rank correlation analysis were conducted using MetaboAnalyst 4.0 (http://www.metaboanalyst.ca/) [22]. Eight differential metabolites in AH and 15 differential metabolites in vitreous were evaluated for pathway analysis using the “Homo sapiens (KEGG)” library with the default parameters (“Hypergeometric test” and “Relative-betweenness Centrality”) specified as the algorithms for pathway enrichment and topological analysis, respectively. Spearman rank correlation analysis was implemented among those significantly changed metabolites and clinical data of diabetes retinopathy patients. A forward stepwise logistic regression analysis and receiver-operating characteristic (ROC) analysis were performed using SPSS software version 18.0 (IBM Corp., Armonk, New York) for diagnosis of different diabetes retinopathy from controls.
Results
Sample characteristics
The clinical characteristics of participants selected for discovery metabolomic profiling are shown in Tables 1 and 2. Patient characteristics were well matched between control and DR groups.
Global metabolomics profiles between control and DR groups
The metabolic profiles were evaluated between control and DR groups using unsupervised statistics. As shown in Fig. 1, the PCA score plot with the first two and three principal components showed a suggestion separation between the control and DR groups, means that DR caused gradual alterations in metabolism.
Global metabolomics profile analysis. a, b Principal component analysis scatter plots showing the first two and three principal components with control and ADR groups; c, d principal component analysis scatter plots showing the first two and three principal components with control and VDR groups. Aqueous humor DR, ADR; vitreous DR, VDR
Significant disturbed metabolites between control and DR groups
Metabolite profiling demonstrated a suggestion difference between control and DR groups. To further investigate the potential biomarkers that account for DR, supervised OPLS-DA was performed. In the OPLS-DA model, clear differences were obtained for the following: aqueous humor DR (ADR) versus control group, cumulative R2Y at 0.677 and Q2Y at 0.482 (Fig. 2a); vitreous DR (VDR) versus control group, cumulative R2Y at 0.713 and Q2Y at 0.529 (Fig. 2b). A cluster of 200 permutated models was visualized using validation plots. The validation plots (Fig. 2c, d) from permutation test strongly supported the validity of the established OPLS-DA model as all permuted R2 and Q2 values on the left were lower than the original point on the right, and that the Q2 regression line in blue had a negative intercept [23]. Figure 2e, f shows the S-plot of OPLS-DA. The potential biomarkers from S-plot in our study were selected according to the parameter of VIP. In the S-plot, 25 and 29 features (red highlighted) were found to have VIP values higher than 1 in AH and vitreous, respectively. Then, the variables were further confirmed by Mann–Whitney U test, and metabolites listed in Table 3 were selected as potential biomarkers (p < 0.05).
Significant disturbed metabolites analysis. The orthogonal projection to latent structure discriminant analysis (OPLS-DA) between control and ADR groups (a, c, and e), between control and VDR groups (b, d, and f). OPLS-DA score plots a, b showed clustering, validation plot using a 200 times permutation test c, d showed the performance of OPLS-DA model, while an S-plot e, f identified the different metabolites. Aqueous humor DR, ADR; vitreous DR, VDR
Metabolic pathway analysis associated with DR
As metabolites and enzymes involved in the same biological processes are often dysregulated together [24], higher-order quantitative representations of metabolomics features, such as pathway-based metabolomics features, are coherent surrogates of metabolomics biomarkers that provide more information on biological functions. In order to identify biologically meaningful patterns that are significantly enriched in metabolomic data [25], pathway analysis was performed using Metaboanalyst software. The relevant pathways on the basis of the eight differential metabolites in AH are shown in Fig. 3a, and those related to the 15 differential metabolites in vitreous are shown in Fig. 3b. Glycolysis or gluconeogenesis, galactose metabolism, and ascorbate–aldarate metabolism were three significantly perturbed pathways in ADR (p < 0.01). Similarly, valine–leucine–isoleucine biosynthesis, taurine–hypotaurine metabolism, arginine–proline metabolism, alanine–aspartate–glutamate, aminoacyl-tRNA biosynthesis, and nitrogen metabolism are highlighted as the notably disturbed pathways in VDR group (p < 0.01), which are indicated with the high pathway importance.
Pathway analysis. a Pathway analysis of eight different metabolites associated with ADR, and the x-axis represents the pathway impact, and the y-axis represents the log(p); b pathway analysis of 15 different metabolites associated with VDR, and the x-axis represents the pathway impact, and the y-axis represents the log(p). Aqueous humor DR, ADR; vitreous DR, VDR
Potential biomarkers analysis for discrimination
We assessed the impact of multiple metabolites and selected the best combination of potential biomarkers for discrimination, using a forward stepwise regression selection procedure. The ROC presentation on the basis of the logistic regression of each biomarker panel is shown in Fig. 4. ROC curve shows improving effects of adding demographic characteristics. The model containing panel metabolites corrected for the effect of gender, age, and BMI showed the best characteristics and allows very good discrimination between control and DR groups. The AUC, sensitivity, and specificity of the logistic regression model established by d-2,3-Dihydroxypropanoic acid, isocitric acid, fructose 6-phosphate, and l-Lactic acid from ADR were 0.965, 88%, and 95.7% (Fig. 4a). The AUC, sensitivity, and specificity of the logistic regression model established by pyroglutamic acid and pyruvic acid from VDR were 0.951, 95.5%, and 85.7% (Fig. 4b). Spearman rank correlation analysis was performed among different metabolites with individual phenotypes. d-2,3-Dihydroxypropanoic acid, isocitric acid, and l-Lactic acid in AH showed significantly negative correlation with FBG and HbA1c (Figure S1A). Meanwhile, the two potential vitreous biomarkers, pyruvic acid, and pyroglutamic acid exhibited strong positive correlation with HbAlc (Figure S1B).
Potential biomarkers analysis for discrimination. a The diagnostic outcomes of potential biomarkers are shown via the ROC curves for comparison between ADR versus control; b the diagnostic outcomes of potential biomarkers are shown via the ROC curves for comparison between VDR versus control. Aqueous humor DR, ADR; vitreous DR, VDR
Discussion
Metabolomics is a prospective approach to explore the pathogenesis of the disease. The metabolomic information of vitreous and AH can provide a direct indication of the physiological status of the eyes [26]. In our study, we discovered eight metabolites in AH sample (d-2,3-Dihydroxypropanoic acid, isocitric acid, threonic acid, d-glucose, myoinositol, l-Lactic acid, fructose 6-phosphate, and citrulline) and 15 metabolites in vitreous sample (pyruvic acid, uric acid, ornithine, l-lysine, l-leucine, pyroglutamic acid, l-alanine, l-threonine, hydroxylamine, l-valine, l-alloisoleucine, l-phenylalanine, creatinine, myoinositol, and l-glutamine). Our results supported the identification of eight vitreous metabolites as reported in the previous vitreous studies (uric acid [27], l-lysine [28], l-leucine [28], l-alloisoleucine [28], hydroxylamine [29], l-valine [30], l-phenylalanine [31], and creatinine [32]). Three AH metabolites from our study were found in the vitreous from other studies (d-glucose [33], myoinositol [34], and citrulline [35]). There were 11 novel metabolites that have not been detected previously (d-2,3-Dihydroxypropanoic acid, isocitric acid, threonic acid, l-threonine, l-glutamine, l-Lactic acid, fructose 6-phosphate, pyruvic acid, ornithine, pyroglutamic acid, and l-alanine). These metabolites detected in our research may merit further investigation as key molecules in DR pathogenesis. In order to fully understand biologically meaningful patterns of these identified metabolites, we carried out entire metabolic pathways analysis to explore pathway-based metabolomics features.
In our research, the ascorbate–aldarate pathway and markedly disturbed threonic acid were detected in ADR group. Ascorbic acid and threonic acid are central signaling hubs in ascorbate–aldarate pathway. Threonic acid is considered to be a major breakdown product of ascorbic acid. Ascorbic acid is a cofactor for several hydroxylases including proline hydroxylase and dopamine hydroxylase [36], which play important roles in neuropeptide synthesis. Hence, the lack of ascorbic acid may have an important effect on the early neurodegeneration observed in DR. Studies also indicate that ascorbic acid probably inhibits angiogenesis, a central event in DR, as suggested by experiments with corneal neovascularization in rodent models [37]. Ascorbic acid metabolism impairment was discovered in patients with diabetes who developed DR [38]. We conceived that regulation of ascorbic acid might provide a valuable approach to combat angiogenesis change in DR, especially for the patients who are inclined to develop INV.
d-glucose was notably disturbed, and glycolysis pathway was highlighted as an important pathway in ADR sample. Glucose flux is known to inhibit the glycolytic enzyme GAPDH and divert upstream metabolites from glycolysis into pathways of glucose overutilization, which can result in increased flux of dihydroxyacetone phosphate (DHAP) to de novo synthesis of diacylglycerol (DAG) and downstream protein kinase C (PKC) [39,40,41]. PKC is a family of ten enzymes, in which the β isoform appears to be closely associated with the development of DR [42, 43]. Hyperglycemia-induced activation of PKC β increases vascular permeability as well as expression of VEGF and neovascularization in animal models [44]. Two-phase three trials suggest that an orally administered PKC inhibitor has a magnitude of effect on reducing vision loss in patients with DR [45]. Although the sustained moderate visual loss in PKC inhibitor group was 2.3% and not considered statistically significant compared to 4.4% of the placebo group (P = 0.069). PKC β pathway alone may not be sufficient to completely inhibit the development of DR. But based on our discoveries, we believe PKC is still a prospective intervention target. We hypothesize that blocking the PKC β-related metabolic pathway or second-generation PKC inhibitor might offer a valuable opportunity for slowing the progression of DR.
In our vitreous sample, the arginine–proline metabolism pathway was highlighted. Meanwhile, the associated ornithine significantly augmented. In retina, arginine is metabolized through two distinct pathways: the arginase pathway through which ornithine and urea are generated by enzyme arginase II (Arg-II), and the nitric oxide synthase (NOS) pathway, which produces citrulline and NO [46]. The increased ornithine in diabetic status indicated the overactivity of the enzyme Arg-II, which is known as proinflammatory factor for macrophages-mediated chronic inflammation in type 2 diabetes mellitus. Meanwhile, overactivity of Arg-II can consequently cause a shortage of arginine for the NOS pathway, leading to a deficiency of NO. This can result in consequential endothelial cell dysfunction and impaired vasodilation, which are characteristics of DR. It can also lead to NOS uncoupling which generates increased level of oxygen and nitrogen reactive species that can accelerate DR [47]. Based on our discoveries, we conjectured that blocking Arg-II might serve as a potential therapeutic strategy to delay the progression of DR.
l-leucine and l-valine were found increased in VDR group. The linked branched-chain amino acids (BCAAs) (valine–leucine–isoleucine biosynthesis) pathway was also revealed. Elevated circulating BCAAs level and related metabolites have been significantly associated with insulin resistance [48,49,50] and diabetes-related disease [51, 52]. Higher BCAAs level has been considered to track with increased neurotoxic level of glutamate in retina, which might play a major role in the DR neurodegeneration [53]. Primarily, BCAAs exert its function by activation of mammalian target of rapamycin (mTOR) pathway, which regulates cell growth, proliferation, and survival [54]. It has been reported that mTOR can activate IKK and NF-κB along with downstream inflammatory cytokines [55], chemokines, and adhesion molecules, the early components accelerating the progression of DR. mTOR is also known to play a pivotal role in upregulating VEGF pathway, which leads to augmented Caspase-3 expression and causes consequent retinal damages in DR animal model [56, 57]. mTOR can also cause leakage and breakdown of the blood–retinal barrier. Experimental findings suggest that inhibition of mTOR pathway could prohibit the proliferation and migration of endothelial cells which are requirements for neovascularization in DR [58]. Thus, it can be surmised that targeting BCAAs–mTOR pathway could have beneficial therapeutic effects on preventing the neuropathy and vasculopathy observed in DR. A recent clinical trial showed empagliflozin, a sodium–glucose cotransporter-2 inhibitor, could particularly regulate BCAAs catabolism in patients with type 2 diabetes-related cardiovascular disease [51, 59]. We speculated that empagliflozin could potentially provide a novel therapeutic opportunity for the management of DR.
Besides pathway analysis, we also assessed the impact of multiple metabolites. The ROC results indicated that the combination of d-2,3-Dihydroxypropanoic acid, isocitric acid, and l-Lactic acid from ADR and pyroglutamic acid and pyruvic acid from VDR could serve as potential biomarkers for good discrimination between control and DR groups. The previous metabolomics study of diabetic kidney disease (DKD) revealed reduced level of isocitric acid which showed better diagnosis values for DKD [60]. Lactic acid was considered as new risk marker for diabetes mellitus like diabetic ketoacidosis and diabetic nephropathy [61, 62]. Changes in pyroglutamic acid and pyruvic acid in diabetes provided useful information regarding diagnostic or prognostic biomarkers [63, 64]. These studies showed really positive support for our outcomes. Our spearman rank correlation analysis also indicated these five metabolites differentially expressed in DR patients and showed significant correlation with FBG or HbA1c. But obtaining AH or vitreous sample for the diagnosis of PDR is not practical. Instead, this discovery could be used as a prediction of PDR and allow us to perform active intervention for this kind of patients.
In conclusion, these discoveries expanded our understanding about identified metabolites and revealed for the first time some central metabolites that are disturbed in the progression of DR. These results may allow the development of metabolic biomarkers for prognosis and novel therapeutic strategies to prevent or delay the development of DR. However, further investigation is necessary to confirm these metabolic reprogramming pathways. We recognize there are limitations to our study. The patient sample size is small. Subsequent studies will enroll more participants and also combine the serum sample assay to reinforce the result.
References
Wang L et al (2017) Prevalence and ethnic pattern of diabetes and prediabetes in China in 2013. JAMA 317(24):2515–2523
Yang QH et al (2019) Prevalence of diabetic retinopathy, proliferative diabetic retinopathy and non-proliferative diabetic retinopathy in Asian T2DM patients: a systematic review and meta-analysis. Int J Ophthalmol 12(2):302–311
Klein BE (2007) Overview of epidemiologic studies of diabetic retinopathy. Ophthalmic Epidemiol 14(4):179–183
Ciulla TA, Amador AG, Zinman B (2003) Diabetic retinopathy and diabetic macular edema: pathophysiology, screening, and novel therapies. Diabetes Care 26(9):2653–2664
Li X et al (2011) Metabolomics study of diabetic retinopathy using gas chromatography-mass spectrometry: a comparison of stages and subtypes diagnosed by Western and Chinese medicine. Mol BioSyst 7(7):2228–2237
Albers JW et al (2010) Effect of prior intensive insulin treatment during the Diabetes Control and Complications Trial (DCCT) on peripheral neuropathy in type 1 diabetes during the Epidemiology of Diabetes Interventions and Complications (EDIC) Study. Diabetes Care 33(5):1090–1096
Group AC et al (2008) Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 358(24):2560–2572
Brasacchio D et al (2009) Hyperglycemia induces a dynamic cooperativity of histone methylase and demethylase enzymes associated with gene-activating epigenetic marks that coexist on the lysine tail. Diabetes 58(5):1229–1236
El-Osta A et al (2008) Transient high glucose causes persistent epigenetic changes and altered gene expression during subsequent normoglycemia. J Exp Med 205(10):2409–2417
Chalmers J, Cooper ME (2008) UKPDS and the legacy effect. N Engl J Med 359(15):1618–1620
Pirola L et al (2010) Epigenetic phenomena linked to diabetic complications. Nat Rev Endocrinol 6(12):665–675
Fang J et al (2017) Metabolomics combined with pattern recognition and bioinformatics analysis methods for the development of pharmacodynamic biomarkers on liver fibrosis. Mol BioSyst 13(8):1575–1583
Baharum SN, Azizan KA (2018) Metabolomics in systems biology. Adv Exp Med Biol 1102:51–68
Tomasova P et al (2019) Metabolomics based on MS in mice with diet-induced obesity and type 2 diabetes mellitus: the effect of vildagliptin, metformin, and their combination. Appl Biochem Biotechnol 188(1):165–184
Jaeger C et al (2017) Compound annotation in liquid chromatography/high-resolution mass spectrometry based metabolomics: robust adduct ion determination as a prerequisite to structure prediction in electrospray ionization mass spectra. Rapid Commun Mass Spectrom 31(15):1261–1266
Phua LC et al (2013) Global gas chromatography/time-of-flight mass spectrometry (GC/TOFMS)-based metabonomic profiling of lyophilized human feces. J Chromatogr B Analyt Technol Biomed Life Sci 937:103–113
Yin S et al (2017) Optimization of GC/TOF MS analysis conditions for assessing host-gut microbiota metabolic interactions: Chinese rhubarb alters fecal aromatic amino acids and phenol metabolism. Anal Chim Acta 995:21–33
Gao J et al (2016) Association between serum bile acid profiles and gestational diabetes mellitus: a targeted metabolomics study. Clin Chim Acta 459:63–72
Wang S et al (2018) Association of serum metabolites with impaired fasting glucose/diabetes and traditional risk factors for metabolic disease in Chinese adults. Clin Chim Acta 487:60–65
Floegel A et al (2013) Identification of serum metabolites associated with risk of type 2 diabetes using a targeted metabolomic approach. Diabetes 62(2):639–648
Qiu Y et al (2014) A distinct metabolic signature of human colorectal cancer with prognostic potential. Clin Cancer Res 20(8):2136–2146
Xia J, Wishart DS (2016) Using metaboanalyst 3.0 for comprehensive metabolomics data analysis. Curr Protoc Bioinform 55:14101–141091
Ke C et al (2016) Metabolic phenotyping for monitoring ovarian cancer patients. Sci Rep 6:23334
Zhang F, Du G (2012) Dysregulated lipid metabolism in cancer. World J Biol Chem 3(8):167–174
Wang X et al (2013) Metabolomics and proteomics annotate therapeutic properties of geniposide: targeting and regulating multiple perturbed pathways. PLoS ONE 8(8):e71403
Haines NR et al (2018) Metabolomics Analysis of Human Vitreous in Diabetic Retinopathy and Rhegmatogenous Retinal Detachment. J Proteome Res 17(7):2421–2427
Zhu DD et al (2018) The role of uric acid in the pathogenesis of diabetic retinopathy based on Notch pathway. Biochem Biophys Res Commun 503(2):921–929
Vidhya S et al (2018) Free amino acids hydroxyproline, lysine, and glycine promote differentiation of retinal pericytes to adipocytes: a protective role against proliferative diabetic retinopathy. Exp Eye Res 173:179–187
Sanchez-Chavez G et al (2016) Potential role of endoplasmic reticulum stress in pathogenesis of diabetic retinopathy. Neurochem Res 41(5):1098–1106
Ola MS et al (2013) Neurodegeneration and neuroprotection in diabetic retinopathy. Int J Mol Sci 14(2):2559–2572
Gong MT et al (2018) Comprehensive analysis of gene expression profiles associated with proliferative diabetic retinopathy. Exp Ther Med 16(4):3539–3545
Romero-Aroca P et al (2018) Glomerular filtration rate and/or ratio of urine albumin to creatinine as markers for diabetic retinopathy: a ten-year follow-up study. J Diabetes Res 2018:5637130
Lauritzen T et al (1983) Effect of 1 year of near-normal blood glucose levels on retinopathy in insulin-dependent diabetics. Lancet 1(8318):200–204
MacGregor LC et al (1986) Altered retinal metabolism in diabetes. I. Microanalysis of lipid, glucose, sorbitol, and myo-inositol in the choroid and in the individual layers of the rabbit retina. J Biol Chem 261(9):4046–4051
Kumaramanickavel G et al (2002) Inducible nitric oxide synthase gene and diabetic retinopathy in Asian Indian patients. Clin Genet 61(5):344–348
Komeima K et al (2006) Antioxidants reduce cone cell death in a model of retinitis pigmentosa. Proc Natl Acad Sci USA 103(30):11300–11305
Ashino H et al (2003) Novel function of ascorbic acid as an angiostatic factor. Angiogenesis 6(4):259–269
Sinclair AJ et al (1991) Disturbed handling of ascorbic acid in diabetic patients with and without microangiopathy during high dose ascorbate supplementation. Diabetologia 34(3):171–175
Brownlee M (2001) Biochemistry and molecular cell biology of diabetic complications. Nature 414(6865):813–820
Wang QJ (2006) PKD at the crossroads of DAG and PKC signaling. Trends Pharmacol Sci 27(6):317–323
Xia P et al (1994) Characterization of the mechanism for the chronic activation of diacylglycerol-protein kinase C pathway in diabetes and hypergalactosemia. Diabetes 43(9):1122–1129
Koya D, King GL (1998) Protein kinase C activation and the development of diabetic complications. Diabetes 47(6):859–866
Galvez MI (2011) Protein kinase C inhibitors in the treatment of diabetic retinopathy. Review Curr Pharm Biotechnol 12(3):386–391
Sheetz MJ et al (2011) Effect of ruboxistaurin (RBX) on visual acuity decline over a 6-year period with cessation and reinstitution of therapy: results of an open-label extension of the Protein Kinase C Diabetic Retinopathy Study 2 (PKC-DRS2). Retina 31(6):1053–1059
Sheetz MJ et al (2013) The effect of the oral PKC beta inhibitor ruboxistaurin on vision loss in two phase 3 studies. Invest Ophthalmol Vis Sci 54(3):1750–1757
Narayanan SP et al (2014) Arginase 2 deficiency reduces hyperoxia-mediated retinal neurodegeneration through the regulation of polyamine metabolism. Cell Death Dis 5:e1075
Narayanan SP et al (2013) Arginase in retinopathy. Prog Retin Eye Res 36:260–280
Lynch CJ, Adams SH (2014) Branched-chain amino acids in metabolic signalling and insulin resistance. Nat Rev Endocrinol 10(12):723–736
Zhao X et al (2016) The Relationship between branched-chain amino acid related metabolomic signature and insulin resistance: a systematic review. J Diabetes Res 2016:2794591
Yoon MS (2016) The emerging role of branched-chain amino acids in insulin resistance and metabolism. Nutrients 8(7):405–417
Kappel BA et al (2017) Effect of empagliflozin on the metabolic signature of patients with type 2 diabetes mellitus and cardiovascular disease. Circulation 136(10):969–972
Bhattacharya S et al (2014) Validation of the association between a branched chain amino acid metabolite profile and extremes of coronary artery disease in patients referred for cardiac catheterization. Atherosclerosis 232(1):191–196
Ola MS, Alhomida AS, LaNoue KF (2019) Gabapentin attenuates oxidative stress and apoptosis in the diabetic rat retina. Neurotox Res. https://doi.org/10.1007/s12640-019-00018-w
Hung CM et al (2012) mTOR-dependent cell survival mechanisms. Cold Spring Harb Perspect Biol. https://doi.org/10.1101/cshperspect.a008771
Dan HC et al (2008) Akt-dependent regulation of NF-κB is controlled by mTOR and Raptor in association with IKK. Genes Dev 22(11):1490–1500
Wei J et al (2016) Blocking mammalian target of rapamycin (mTOR) attenuates HIF-1α pathways engaged-vascular endothelial growth factor (VEGF) in diabetic retinopathy. Cell Physiol Biochem 40(6):1570–1577
Jacot JL, Sherris D (2011) Potential therapeutic roles for inhibition of the PI3K/Akt/mTOR pathway in the pathophysiology of diabetic retinopathy. J Ophthalmol 2011:589813
Adini I et al (2003) RhoB controls Akt trafficking and stage-specific survival of endothelial cells during vascular development. Genes Dev 17(21):2721–2732
Herat LY et al (2018) Focusing on sodium glucose cotransporter-2 and the sympathetic nervous system: potential impact in diabetic retinopathy. Int J Endocrinol 2018:9254126
Li L et al (2017) Metabolomics reveal mitochondrial and fatty acid metabolism disorders that contribute to the development of DKD in T2DM patients. Mol BioSyst 13(11):2392–2400
Lu J et al (2011) Closing the anion gap: contribution of D-lactate to diabetic ketoacidosis. Clin Chim Acta 412(3–4):286–291
Chou CK et al (2015) Elevated urinary D-lactate levels in patients with diabetes and microalbuminuria. J Pharm Biomed Anal 116:65–70
Chou J et al (2018) Fasting serum alphahydroxybutyrate and pyroglutamic acid as important metabolites for detecting isolated post-challenge diabetes based on organic acid profiles. J Chromatogr B Analyt Technol Biomed Life Sci 1100–1101:6–16
Makahleh A, Ben-Hander GM, Saad B (2015) Determination of alpha-ketoglutaric and pyruvic acids in urine as potential biomarkers for diabetic II and liver cancer. Bioanalysis 7(6):713–723
Acknowledgements
We acknowledge Dr Xun Xu (MD) from our department for providing medical writing assistant.
Funding
This work was supported in part by grants from National Key R&D Program of China (No. 2016YFC0904800) and National Natural Science Foundation of China (No. 81870666).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors have declared that there are no conflicts of interest.
Statement of human and animal rights
The study was prospectively approved by the Ethics Committee of Shanghai First People’s Hospital of Shanghai Jiaotong University, and research was conducted in accordance to the Declaration of Helsinki.
Informed consent
Signed informed consent was obtained from all participants enrolled in the study.
Additional information
Managed by Massimo Porta.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wang, H., Fang, J., Chen, F. et al. Metabolomic profile of diabetic retinopathy: a GC-TOFMS-based approach using vitreous and aqueous humor. Acta Diabetol 57, 41–51 (2020). https://doi.org/10.1007/s00592-019-01363-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-019-01363-0