Abstract
Aims
Retinopathy is a leading cause of vision impairment in diabetes. Its pathogenesis involves inflammation, pathological angiogenesis, neuronal and glial dysfunction. The purinergic P2X7 receptor (P2X7R) has a leading role in inflammation and angiogenesis. Potent and selective P2X7R blockers have been synthesized and tested in Phase I/II clinical studies. We hypothesize that P2X7R blockade will ameliorate diabetes-related pathological retinal changes.
Methods
Streptozotocin (STZ)-treated rats were intraperitoneally inoculated with either of two small molecule P2X7R receptor inhibitors, A740003 and AZ10606120, and after blood glucose levels increased to above 400 mg/dL, retinae were analyzed for P2X7R expression, vascular permeability, VEGF, and IL-6 expression.
Results
STZ administration caused a near fourfold increase in blood glucose, a large increase in retinal microvasculature permeability, as well as in retinal P2X7R, VEGF, and IL-6 expression. P2X7R blockade fully reversed retinal vascular permeability increase, VEGF accumulation, and IL-6 expression, with no effect on blood glucose.
Conclusion
P2X7R blockade might be promising strategy for the treatment of microvascular changes observed in the early phases of diabetic retinopathy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetic retinopathy (DR) is a global health burden [1, 2]. Hyperglycemia is the main cause of retinal neuron damage and microangiopathy, likely as a trigger of retinal inflammation [3]. Microaneurysms, small hemorrhages, and dilatation of capillaries and small veins occur in the microcirculation of the retina from the inception of diabetes, till the advanced stages characterized by neo-angiogenesis and fibrosis [4]. Vascular endothelial growth factor (VEGF) is a key pathogenic factor in DR, and in fact local administration of anti-VEGF monoclonal antibodies is a key therapy for DR [4, 5].
Low-grade inflammation has a main role in the complex pathogenesis of type 2 diabetes [6]. Extracellular ATP (eATP), acting at P2 receptors, synergizes with chemokines and cytokines, to drive several inflammatory responses, and at the same time is the precursor of adenosine, a powerful anti-inflammatory agent, which in principle accumulates at inflammatory sites to down-modulate inflammation, in the typical negative feed-back circuit of all homeostatic systems [7]. The P2X7 receptor (P2X7R) is a main player in the pathophysiological changes driven by eATP as it causes maturation and release of interleukin-1β (IL-1β), as well as of other cytokines (e.g., IL-6), reactive oxygen species [ROS], and matrix metalloproteases [8, 9]. P2X7R stimulation also promotes VEGF release in several pathological settings such as tumors where P2X7R overexpression leads to increased VEGF accumulation and enhanced angiogenesis [10, 11].
A role for the P2X7R, and more in general for purinergic signaling, in retinal damage has been hypothesized in previous studies [12], but few papers provided direct in vivo evidence in support [13]. Most pharmaceutical companies have developed highly selective small molecule P2X7R blockers, some of which were taken to clinical Phases I and II for the treatment of chronic inflammatory diseases [9]. Thus, a large number of potential drugs, some of which are permeant across the blood retinal barrier (BRB), might be available for the treatment of DR.
In this study, we tested the hypothesis that P2X7R blockade might reverse retinal damage in a rat model of type 1 diabetes.
Materials and methods
Animals
Fifty-seven male Wistar rats of 150–180 g b.w. were used. Rats were randomized after overnight fasting to induce diabetes by intraperitoneal (i.p.) streptozotocin (STZ) administration (60 mg/kg in 10 mM citrate buffer, pH 4.5, Sigma-Aldrich, St Louis, MO, USA), or to receive vehicle, and were double-blind tested. Blood glucose levels were measured with a glucometer in non-fasted rats; a blood glucose concentration ≥ 250 mg/dL 48 h after STZ treatment defined the diabetic condition. Fifteen days after STZ, rats were i.p. injected with P2X7R blockers (AZ10606120 or A740063 in the morning, at a dose of 100 μg/kg) or vehicle, every 2 days for additional 15 days, for a total of seven injections. The day following the last injection, rats were anesthetized with 70% ketamine and 30% xylazine (1 μl/g body weight, i.p.), and permeability of the BRB was examined with the Evans blue method [14]. At this time, retinae were withdrawn for biochemical analysis in other similarly treated-groups. Stock solutions of AZ10606120 or A740063 were made in sterile PBS or DMSO, respectively, and were both diluted in sterile PBS for administration.
Quantitative PCR
Total RNA was isolated from frozen retinas using TRIzol reagent (Life Technologies, Carlsbad, CA, USA), and cDNA was synthesized with the High-Capacity cDNA Reverse Transcription Kit (Applied Biosystems, Warrington, UK). PCR products were quantified with Maxima SYBR Green/ROX qPCR Master Mix (Thermo Scientific, Auburn, AL, USA) in a 10-μl final reaction volume containing template and 0.5 mM of each of the following primer pairs: P2X7R (sense 5′-CTTCGGCGTGCGTTTTG-3′, antisense 5′-AGGACAGGGTGGATCCAATG-3′), VEGF-A (sense 5′-TGCCAAGTGGTCCCAG-3′, antisense 5′-GTGAGGTTTGATCCGC-3′), and IL-6 (5′-TCCAACTCATCTTGAAAGCA-3′, antisense 5′-TTCATATTGCCAGTTCTTCG-3′).
Western blot
Each retina was homogenized in lysis buffer (0.1 M Tris–HCl, pH 7.5, 0.2 M EGTA, 0.2 M EDTA, 0.1 M sodium orthovanadate, 50 mM sodium fluoride, 100 mM sodium acid pyrophosphate, 250 mM sucrose) supplemented with a protease inhibitor cocktail (complete, mini, EDTA-free; Roche Diagnostics, Mannheim, Germany) and the homogenate centrifuged as described [14]. The homogenate (25 μg of protein) was boiled and run on a 7% SDS-PAGE acrylamide gel. Proteins were then blotted onto nitrocellulose membranes, incubated with a 1:500 dilution of anti-P2X7 receptor polyclonal antibody (Alomone Laboratories, Jerusalem, Israel) and stained with an alkaline phosphatase coupled secondary antibody (Bio-Rad, Hercules, CA, USA) or 1:1000 anti-βtubulin (ab6046; Abcam, Cambridge, MA, USA). Western blots were analyzed with Scanner Perfection V500 (EPSON, Long Beach, CA, USA). Optical density values were determined with Quantity One image analysis software (Bio-Rad, Richmond, CA, USA).
Evans blue method
Briefly, anesthetized rats were intrajugularly injected in the morning (8–9 am) with the Evans blue tracer (45 mg/kg, Sigma-Aldrich). Two hours later, 1 ml of heart-drawn blood was used to measure plasma Evans blue concentration, and rats were perfused for 2 min via the left ventricle with PBS (pH 3.5 at 37 °C). The retina was dissected and vacuum-dried (SPD 1010 SpeedVac System, ThermoSavant, Wilmington, USA) for 4 h, and after weighing the Evans blue tracer was extracted with 250 μl formamide (Mallinckrodt Baker, Phillipsburg, NJ, USA) for 18 h at 72 °C under agitation at 350 rpm. Absorbance was measured in 100 μl of the extract at 620 nm using a Varioskan Flash spectrophotometer (Thermo Fisher Scientific, Wilmington, DE, USA). Tracer concentration in the extracts was normalized to the retina and body weight and to plasma Evans blue concentration [14].
ELISA for VEGF
Retinae were homogenized and centrifuged as described in the Western blot section. We used one hundred μg of supernatant protein for VEGF measurements (Quantikine ELISA Kit, R&D Systems Inc., Minneapolis, MN, USA). The assay recognizes both natural and recombinant rat VEGF with intra- and inter-assay coefficients of variance of 5.75 and 7.5%, respectively, and a sensitivity of 8.4 pg/ml. Absorbance was measured with the Varioskan Flash spectrophotometer (Thermo Fisher Scientific).
Statistical analysis
Data are reported as mean ± SEM. Statistical differences between groups were determined by the unpaired two-tailed Student’s t test or by one-way ANOVA followed by Bonferroni test setting. Threshold for significance was p < 0.05. Analyses were performed using the Sigma Stat 7.0 software (Systat Software, San Jose, CA, USA).
Results
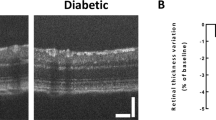
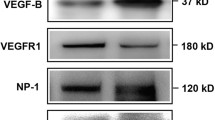
Pathological increase in microvessel permeability is one of the most serious changes occurring during the early phases of DR. Increased permeability allows accumulation of plasma proteins into the retina, and diapedesis of inflammatory cells, thus setting the stage for full blown inflammation [15]. As early as 2 weeks after STZ administration, retinae showed an about twofold increase in the expression of P2X7R mRNA and protein (Fig. 1a–c), as well as a large increase in microvasculature permeability, as measured by leakage of Evans blue-stained plasma proteins (Fig. 1d, e). At this time point, blood glucose was 482 ± 36 mg/dL (n = 8), with a basal blood glucose level in untreated animals of 114 ± 6 mg/dL (n = 9). Permeability increase was fully reversed in rats i.p. injected every other day starting at 2 weeks after STZ injection with either of the potent P2X7R blockers A740003 (Fig. 1d) or AZ10606120 (Fig. 1e). At the time microvasculature permeability was examined (4 weeks after STZ injection), blood glucose level was 524 ± 35 mg/dL (n = 4) in STZ-treated and 141 ± 36 mg/dL (n = 4) in control rats. Administration of P2XR blockers had no effect on blood glucose irrespective of STZ treatment. Of note, P2X7R inhibition with either blockers did not affect plasma protein leakage in the absence of STZ treatment (control cohort), suggesting that basal physiological microvasculature permeability was unaffected. A key causative agent of the microvasculature changes in diabetes is VEGF, whose release is promoted by P2X7R stimulation [10, 11], and thus we verified whether P2X7R blockade could antagonize VEGF accumulation. Figure 2a, b shows that STZ treatment triggered a large increase in retinal VEGF mRNA and protein levels, which was fully obliterated by P2X7R blockade. In the control cohort, AZ10606120 induced a small, but statistically significant increase in VEGF protein that was not observed with A740003 (Fig. 2b). One of the main cytokines involved in the pathogenesis of DR is IL-6. Figure 2c shows that IL-6 accumulated in the retinae of STZ-treated rats to a level about 25-fold higher than in control rats. Administration of AZ10606120 or A740003 re-established normal IL-6 levels.
P2X7R blockade reverses the increase in microvasculature permeability in the retinae of diabetic (DB) STZ-treated rats. Retinae from control non-diabetic (C) and DB STZ-treated rats were removed, and P2X7R expression and microvasculature permeability were measured as described in Materials and methods. P2X7R expression (mRNA or protein) was measured 4 weeks after STZ injection. Panel a, mRNA from 5 or 6 retinae from C or DB rats, respectively. Panel b shows representative Western blot of P2X7R expression from 2 control and 2 DB rat retinae. Panel c shows P2X7 densitometry values of retinae from DB rats expressed as fold change over those of control rat retinae processed in different Western blots (n = 4). Protein leakage in the absence or presence of P2X7R antagonists (panels d and e) was measured at 2 and 4 weeks after STZ injection. Symbols correspond to the values of each retina in each given condition. Panel d, two weeks: 6 control and 4 DB STZ-treated rat retinae were used. Panel d, four weeks: 15 control and 8 DB STZ-treated rat retinae; 10 control retinae of rats treated with A740063, and 13 retinae of DB STZ rat treated with A740063. Panel e, two weeks: 6 control and 5 DB STZ-treated rat retinae. Panel e, four weeks: 10 control rat retinae, and 11 DB STZ-treated rat retinae; 7 control retinae from rats treated with AZ10606120, and 11 retinae of DB STZ rat treated with AZ10606120
P2X7R blockade reverses increased VEGF and IL-6 expression in the retinae of STZ-treated rats. Retinae from control non-diabetic (C) and diabetic (DB) STZ-treated rats were removed, and VEGF mRNA (panel a) and protein (panel b) and IL-6 mRNA (panel c) measured as described in Materials and methods. Control and DB STZ-treated rats were injected with either PBS, AZ10606120, or A740003. Symbols correspond to the values of each retina in each given condition. Number of retinae analyzed: controls, 4 in all panels; DB STZ-treated, 5 in all panels; Controls treated with AZ10606120, 4 in panel a and c, 5 in panel b; DB STZ-treated with AZ10606120, 4 in panels a and c, 5 in panels b; controls treated with A740003, 4 in panels a and c, 5 in panel b; STZ- and A740003-treated, 4 in panels a and c, 5 in panels b
Discussion
Retinopathy is a disabling complication of both type 1 and type 2 diabetes and the leading cause of working age blindness in the western world [16]. Its main pathological changes include retinal inflammation, increased vascular permeability, and abnormal angiogenesis on the surface of the retina. Hyperglycemia directly injures retinal neurons and activates Muller glia and microglia to trigger release of pro-inflammatory factors, thus driving increased vascular permeability and recruitment of inflammatory cells; local inflammation further aggravates neuronal damage and accelerates progression toward proliferative DR [3]. Macular edema is treated with intravitreal injection of VEGF-blocking reagents [17]. This therapy is highly effective, but rather invasive and unpractical, since patients must receive monthly intravitreal injections. Thus, a small molecule-based therapy, likely administrable via a less invasive route (e.g., oral or eye drops), might be highly desirable.
The P2X7R might be an appealing target in DR. The inflammatory microenvironment contains high eATP concentrations [18], sufficient to gate even the low affinity P2X7R and thus trigger cytokine release (mainly IL-1β and IL-6), plasma membrane metalloprotease shedding, and ROS generation [9]. Accordingly, P2X7R genetic deletion or its pharmacological inhibition protect from CD40-induced TNFα, IL-1β, ICAM1, and NOS2 overexpression in Müller cells of diabetic mice [13], and P2X7R stimulation is a potent trigger for VEGF release [10]. Moreover, the NLRP3 inflammasome, whose activation can be triggered by P2X7R stimulation, is overexpressed in vitreal fibrovascular membranes of patients with DR, and a dysregulated NLRP3 activation in transgenic (Ins2Akita xVEGF+/−) Akimba hyperglycemic mice leads to vascular leakage and retinal neovascularization [19].’
The P2X7R has been described in ganglion cells, photoreceptors, amacrine cell, pigment epithelial cells, and Muller cells [20,21,22,23], but a recent re-evaluation using a genetically engineered mouse carrying a functional EGFP-tagged P2X7R suggested that the only retinal cell expressing this receptor is Muller glia [24]. Reason for this discrepancy is not clear, especially because functional responses in neuronal and non-neuronal retinal cells that could be assigned to the P2X7R have been reported by several authors [21, 23, 25]. However, it is not surprising that early retinal damage due to hyperglycemia may cause overexpression of the P2X7R since upregulation of this receptor has been associated with inflammatory changes in retinopathies such as age-related macular degeneration (AMD) [26] or in kidneys from type 2 diabetes patients [27]. Whether P2X7R upregulation occurs in microglia as well as in other cells in the retina is at present unknown.
We show here in an animal model of type 1 diabetes that hyperglycemia induces retinal overexpression of P2X7R and that P2X7R blockade fully reverses diabetes-induced microvasculature permeability increases. The P2X7R is a plasma membrane ion channel gated by eATP [9]. It is now widely acknowledged that eATP accumulates in the extracellular environment at inflammatory and tumor sites [28]. As an extracellular messenger, eATP drives a multiplicity of responses, mainly acting as a pro-inflammatory agent. The P2X7R is the main receptor mediating the pro-inflammatory effect of eATP since this receptor is coupled to NLRP3 inflammasome activation and to release of several cytokines, chiefly IL-1β, TNFα, and IL-6. Furthermore, P2X7R activation is also coupled to VEGF release. Previous evidence has implicated the P2X7R in the pathogenesis of type 2 diabetes or in its vascular complications, as well as retinal diseases such as age-related macular degeneration (AMD) [13, 27, 29]. We hypothesized that P2X7R antagonism could revert some of the inflammatory changes observed in diabetic retina. In diabetic rats, retinal permeability ranges from two- to fivefold above basal. Both P2X7R antagonists effectively normalize it. This protective effect is paralleled by a strong inhibition of the VEGF release, thus supporting a key role for P2X7R in advanced DR.
The direct role of IL-6 in the pathogenesis of DR is less known, but with no doubt it contributes to retinal neuron injury and microvasculature damage [30, 31]. Normalization of retinal IL-6 expression after P2X7R blockade reinforces the role of this receptor as a trigger of retinal inflammation and oxidative stress in diabetes, pointing to its targeting as a novel therapeutic option.
Our findings strongly support previous evidence on the protective role of P2X7R blockade in retinopathies of different origin (i.e., DR or AMD). The efficacy of P2X7R blockade is very likely due to two main reasons: a) inhibition of inflammatory cytokine release and b) inhibition of VEGF release. Both these events lead to local inflammatory changes (increase in vascular permeability, recruitment of inflammatory cells, neo-angiogenesis) that are at the basis of retinal degeneration. P2X7R small molecule drugs are safe and easy to administer, and thus treatment of degenerative retinal disease might be a viable future indication.
References
Barrett EJ, Liu Z, Khamaisi M et al (2017) Diabetic microvascular disease: an endocrine society scientific statement. J Clin Endocrinol Metab 102:4343–4410
Klein BE (2007) Overview of epidemiologic studies of diabetic retinopathy. Ophthalmic Epidemiol 14:179–183
Altmann C, Schmidt MHH (2018) The role of microglia in diabetic retinopathy: inflammation. Microvasc Defects Neurodegener Int J Mol Sci 19:e110
Wang W, Lo ACY (2018) Diabetic retinopathy: pathophysiology and treatments. Int J Mol Sci 19:e1816
Mehta H, Hennings C, Gillies MC, Nguyen V, Campain A, Fraser-Bell S (2018) Anti-vascular endothelial growth factor combined with intravitreal steroids for diabetic macular oedema. Cochrane Database Syst Rev 4:CD011599
Coope A, Torsoni AS, Velloso LA (2016) Mechanisms in endocrinology: metabolic and inflammatory pathways on the pathogenesis of type 2 diabetes. Eur J Endocrinol 174:R175–R187
Burnstock G (2006) Pathophysiology and therapeutic potential of purinergic signaling. Pharmacol Rev 58:58–86
Novak I, Solini A (2018) P2X receptor-ion channels in the inflammatory response in adipose tissue and pancreas-potential triggers in onset of type 2 diabetes? Curr Opin Immunol 52:1–7
Di Virgilio F, Dal Ben D, Sarti AC, Giuliani AL, Falzoni S (2017) The P2X7 receptor in infection and inflammation. Immunity 47:15–31
Adinolfi E, Raffaghello L, Giuliani AL et al (2012) Expression of P2X7 receptor increases in vivo tumor growth. Cancer Res 72:2957–2969
Amoroso F, Capece M, Rotondo A et al (2015) The P2X7 receptor is a key modulator of the PI3 K/GSK3beta/VEGF signaling network: evidence in experimental neuroblastoma. Oncogene 34:5240–5251
Bringmann A, Pannicke T, Uhlmann S, Kohen L, Wiedemann P, Reichenbach A (2002) Membrane conductance of Muller glial cells in proliferative diabetic retinopathy. Can J Ophthalmol 37:221–227
Portillo JC, Lopez CY, Miao Y et al (2017) CD40 in retinal muller cells induces P2X7-dependent cytokine expression in macrophages/microglia in diabetic mice and development of early experimental diabetic retinopathy. Diabetes 66:483–493
Diaz-Lezama N, Wu Z, Adan-Castro E et al (2016) Diabetes enhances the efficacy of AAV2 vectors in the retina: therapeutic effect of AAV2 encoding vasoinhibin and soluble VEGF receptor 1. Lab Invest 96:283–295
Fong DS, Aiello LP, Ferris FL III, Klein R (2004) Diabetic retinopathy. Diabetes Care 27:2540–2553
Lim LS, Liew G, Cheung N, Mitchell P, Wong TY (2010) Mixed messages on systemic therapies for diabetic retinopathy. Lancet 376:1461
Cai S, Bressler NM (2017) Aflibercept, bevacizumab or ranibizumab for diabetic macular oedema: recent clinically relevant findings from DRCR.net Protocol T. Curr Opin Ophthalmol 28:636–643
Morciano G, Sarti AC, Marchi S et al (2017) Use of luciferase probes to measure ATP in living cells and animals. Nat Protoc 12:1542–1562
Chaurasia SS, Lim RR, Parikh BH et al (2018) The NLRP3 inflammasome may contribute to pathologic neovascularization in the advanced stages of diabetic retinopathy. Sci Rep 8:2847
Brandle U, Kohler K, Wheeler-Schilling TH (1998) Expression of the P2X7-receptor subunit in neurons of the rat retina. Brain Res Mol Brain Res 62:106–109
Hu H, Lu W, Zhang M et al (2010) Stimulation of the P2X7 receptor kills rat retinal ganglion cells in vivo. Exp Eye Res 91:425–432
Pannicke T, Fischer W, Biedermann B et al (2000) P2X7 receptors in Muller glial cells from the human retina. J Neurosci 20:5965–5972
Sanderson J, Dartt DA, Trinkaus-Randall V et al (2014) Purines in the eye: recent evidence for the physiological and pathological role of purines in the RPE, retinal neurons, astrocytes, Muller cells, lens, trabecular meshwork, cornea and lacrimal gland. Exp Eye Res 127:270–279
Kaczmarek-Hajek K, Zhang J, Kopp R et al (2018) Re-evaluation of neuronal P2X7 expression using novel mouse models and a P2X7-specific nanobody. Elife 7:e36217
Resta V, Novelli E, Vozzi G et al (2007) Acute retinal ganglion cell injury caused by intraocular pressure spikes is mediated by endogenous extracellular ATP. Eur J Neurosci 25:2741–2754
Hu SJ, Calippe B, Lavalette S et al (2015) Upregulation of P2RX7 in Cx3cr1-deficient mononuclear phagocytes leads to increased interleukin-1beta secretion and photoreceptor neurodegeneration. J Neurosci 35:6987–6996
Solini A, Menini S, Rossi C et al (2013) The purinergic 2X7 receptor participates in renal inflammation and injury induced by high-fat diet: possible role of NLRP3 inflammasome activation. J Pathol 231:342–353
Di Virgilio F, Sarti AC, Falzoni S, De Marchi E, Adinolfi E (2018) Extracellular ATP and P2 purinergic signalling in the tumour microenvironment. Nat Rev Cancer 18:601–618
Vessey KA, Gu BJ, Jobling AI et al (2017) Loss of function of P2X7 receptor scavenger activity in aging mice: a novel model for investigating the early pathogenesis of age-related macular degeneration. Am J Pathol 187:1670–1685
Joussen AM, Poulaki V, Le ML et al (2004) A central role for inflammation in the pathogenesis of diabetic retinopathy. FASEB J 18:1450–1452
Tang J, Kern TS (2011) Inflammation in diabetic retinopathy. Prog Retin Eye Res 30:343–358
Acknowledgements
CC is supported by the National Council of Science and Technology of Mexico [CONACYT, n. 247164]. FDV is supported by Grants from the Italian Association for Cancer Research [n. IG 13025 and IG 18581], the Ministry of Health of Italy [n. RF-2011-02348435], and institutional funds from the University of Ferrara.
Author information
Authors and Affiliations
Contributions
CC conceived and designed the experiments and reviewed the MS; NDL, EAC, GRH, and BMC performed the experiments and analyzed the data; ACS, SF, and AS conceived the study and helped in the analysis of the data; FDV conceived the study and wrote the MS. All authors critically reviewed and/or revised the manuscript for important intellectual content. CC and FDV are the guarantors of this work and, as such, had full access to all the data in the study and took responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Conflict of interest
FDV is a member of the Scientific Advisory Board of Biosceptre Ltd, a UK-based Biotech Company involved in the development of P2X7-targeting antibodies. Other authors declare no conflict of interest.
Ethical approval
Rats were cared for in accordance with the US National Research Council’s Guide for the Care and Use of Laboratory Animals (8th edn, National Academy Press, Washington, DC, USA). The Bioethics Committee of the Institute of Neurobiology of the National University of Mexico (UNAM) approved all animal experiments.
Informed consent
For this type of study, formal consent is not required.
Additional information
Managed by Antonio Secchi.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Clapp, C., Diaz-Lezama, N., Adan-Castro, E. et al. Pharmacological blockade of the P2X7 receptor reverses retinal damage in a rat model of type 1 diabetes. Acta Diabetol 56, 1031–1036 (2019). https://doi.org/10.1007/s00592-019-01343-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-019-01343-4