Abstract
Aims
Type 2 diabetes (T2D) accelerates the decline in glomerular function; however, some individuals do not develop chronic kidney disease despite advanced age and long-lasting T2D. We aimed to phenotype patients with T2D aged 80 years or older who presented with a fully preserved kidney function.
Methods
From an Italian population of 281,217 T2D outpatients, we collected data on demographics, anthropometrics, diabetes duration, HbA1c, fasting plasma glucose, lipids, liver enzymes, estimated glomerular filtration rate (eGFR), albumin excretion rate (AER), chronic complications, and medication use. We primarily compared patients with a fully preserved kidney function (eGFR > 90 ml/min/1.73 m2 and AER < 30 mg/24 h, or G1A1) with those with mild kidney impairment (eGFR 60–90 ml/min/1.73 m2 and AER < 30 mg/24 h, or G2A1).
Results
N = 113,860 had available data for eGFR and AER, 21,648 of whom were aged ≥ 80. G1A1 (n = 278) and G2A1 (n = 6647) patients represented 1.3 and 30.7% of aged T2D patients, respectively, with an average diabetes duration of 16 years. Differences between the G1A1 and G2A1 groups were entered in a multiple logistic regression analysis with and without imputation of missing data. After adjustment and in both imputed and non-imputed datasets, younger age, lower BMI and lower triglycerides were associated with fully preserved versus mildly impaired kidney function. The comparison between G1A1 and G1A2/3 yielded different results.
Conclusions
In a rare population of patients with a fully preserved kidney function despite old age and long-lasting diabetes, lower BMI and triglycerides suggest that protection from lipotoxicity may preserve kidney function over time.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Italy is one of the western countries with the highest prevalence of aging citizens [1, 2]. Due to its aging population, Italy faces a huge public spending on pensions and age-related health problems, including type 2 diabetes (T2D) [3]. Chronic kidney disease (CKD) is also a major health burden in aged people, and particularly in those with T2D [4]. According to population-based studies, the prevalence of CKD in individuals aged 65 years or older ranges from 35 to 44%, with the highest representation observed in those aged 80 years and older [5]. While the progressive decline in glomerular filtration rate (GFR) is a feature of normal aging, T2D accelerates GFR decline, making diabetic individuals prone to develop CKD [6, 7]. A recent observation across Europe has documented a prevalence of CKD stage III–V of 28.5% in France and 27.6% in Germany in people with diabetes aged 65–74 years [8]. In the RIACE study, a prospective observational study evaluating about 16,000 individuals with T2D in Italy [9], the prevalence of CKD stage III–V in the highest age quartile was 34.1% in males and 39.8% in females (AS, unpublished observations). Due to the worldwide epidemic of T2D [10], end-stage renal disease (ESRD) will inevitably become a primary health problem, which will also lead to a progressive increase of the mean age of people undergoing dialysis, a challenging issue in a frail population [11, 12]. The size of this problem urgently calls for strategies to better identify, target, and treat people at risk to progress towards ESRD and, even more, to die for cardiovascular disease [13, 14].
On the other hand, likely thanks to a favorable genetic predisposition, a number of individuals do not develop renal impairment with age and keep fully preserved renal function despite diabetes. A detailed characterization of the phenotype of this subset of individuals would instruct strategies to prevent renal dysfunction in large strata of the general and diabetic population.
Herein, we provide for the first time an extensive comparative phenotyping of T2D subjects aged 80 years or older that exhibit a fully preserved renal function, taking advantage of a large clinical database on the Italian T2D population. To this end, we approached a population of elderly patients with an estimated glomerular filtration rate (eGFR) > 60 ml/min/1.73 m2, and with a normal albumin excretion rate (AER < 30 mg/24 h or mg/g of creatinine). We then compared the rare population of patients with fully preserved kidney function (eGFR > 90 ml/min/1.73 m2,) with those with mild renal impairment (eGFR 60–90 ml/min/1.73 m2). In parallel, we also compared patients with versus those without micro-/macro-albuminuria and eGFR > 90 ml/min/1.73 m2, to evaluate whether determinants of isolated eGFR decline and of isolated AER increase in this elderly T2D population coincide.
Materials and methods
Study design
This study reports a sub-analysis of the background population of the DARWIN-T2D (DApagliflozin Real World evIdeNce in Type 2 Diabetes) project. DARWIN-T2D was a multicentre nationwide retrospective study conducted on 46 diabetic outpatient clinics in Italy, supported by the Italian Diabetes Society. The study collected routinely accumulated clinical data stored in electronic charts and was primarily designed to compare the baseline clinical characteristics and the change in metabolic parameters in patients who were newly initiated on dapagliflozin, dipeptidyl-peptidase 4 inhibitors, sulphonylurea, or GLP-1 receptor agonists. The retrospective analysis was performed by an automated software that interrogated the same electronic chart system at all centers (MyStar Connect [MSC], Me.te.da). Data collection spanned the period from 13th March 2015 to 31st December 2016. The study design and primary results have already been published [15, 16].
Source of data
In addition to the subsets of patients who were newly initiated on glucose lowering medications and formed the primary study cohort, we collected clinical data of the background population of all patients with a diagnosis of T2D attending the participating centers, at the last available visit, irrespectively of medications and with no exclusion criteria. This total population was comprised of 281,217 patients.
The software automatically extracted the following data for each patient: age, sex, diabetes duration, height, weight, body mass index (BMI), waist circumference, smoking status, systolic and diastolic blood pressure, fasting plasma glucose, HbA1c, total cholesterol, high-density lipoprotein (HDL) cholesterol, triglycerides concentrations, low-density lipoprotein (LDL) cholesterol (calculated using the Friedewald formula [17]), liver enzymes, estimated glomerular filtration rate (eGFR) calculated from serum creatinine according to the CKD-EPI formula [18], albumin excretion rate (AER). Only one value of eGFR and AER was used to categorize patients. In the database, AER was coded using different units of measure (65.5% mg/l or mg/min; 34.5% mg/24 h or mg/g creatinine). To derive AER values in the same range of the mg/24 h or mg/g creatinine (normal value < 30), AER reported as mg/l or mg/min (normal value < 20) were multiplied by 1.5, assuming a standard fixed daily urinary volume of 1500 ml. Detailed information on chronic diabetic complications (retinopathy, neuropathy, peripheral arterial disease, foot problems, cerebrovascular disease, and heart disorders) were recorded from the electronic chart, were they are coded according to the ICD-9 system. Finally, we collected data on ongoing glucose lowering medications and medications for the treatment of concomitant conditions, including hypertension, dyslipidemia, and cardiovascular disease.
Cohort selection
Out of the total population of 281,217 patients, we retained for further analysis only those for whom eGFR and AER were both available at the same visit. We then selected patients aged 80 years or older and the resulting population was divided into two groups according to the National Kidney Foundation (NKF) classification [19]: G1A1 (eGFR > 90 ml/min/1.73 m2 and AER < 30 mg/g or mg/24 h); G2A1 (eGFR 60–90 ml/min/1.73 m2 and AER < 30 mg/g or mg/24 h). Comparisons were performed between these two final groups. For an exploratory additional analysis, we compared patients with G1A1 versus those with G1A2/3 to evaluate whether the presence of micro-/macroalbuminuria in individuals with normal eGFR, was associated with a similar phenotype as the presence of a mild eGFR impairment with normoalbuminuria.
Statistical analysis
Continuous data are presented as mean ± standard deviation, whereas categorical data are presented as percentage. Continuous data that significantly departed from the normal distribution upon a Kolmogorov–Smirnov test were log transformed before analysis. Comparisons of continuous variables between the two groups were performed using the 2-tail unpaired Student’s t test, whereas comparisons of categorical variables were performed using the Chi-square test. After describing the differences between the two groups, a multiple logistic regression analysis was performed on the entire dataset with normal kidney function (G1A1) as the dependent variable and parameters that differed between the two groups at p < 0.10 as explanatory variables. To address the issue of missing data, we performed a multiple imputation (MI) procedure. Six imputations were performed using the Markov chain Monte Carlo (MCMC) method, which creates multiple imputed datasets using simulations from a Bayesian prediction distribution for normal data. Goodness of fit of the imputed data versus original data was compared by evaluating mean and distributions for continuous variables, and by evaluating percentages for categorical variables. Then, the logistic regression analysis was performed on each imputed dataset and coefficient pooled as described by Rubin [20]. SPSS version 25 was used. As imputation of a substantial amount of information may result in distortion of the model, we retained only variables that showed a significant association with normal kidney function in both the analysis with and without MI. The statistical significance threshold level was set at p < 0.05.
Results
Patients
Figure 1a shows the study flowchart. Of the total 281,217 patients, 167,357 were discarded for missing information on eGFR (n = 149,475) and/or AER (n = 155,258). Of the remaining 113,860 patients for whom both eGFR and AER were available, 21,648 patients (19.0%) were aged 80 years or older. Prevalence of the various degrees of kidney impairment according to NKF in subjects aged < 80 or 80+ years are shown in Fig. 1b, c, respectively. Among patients aged 80 years or older, 278 (1.3%) had normal kidney function, defined as eGFR > 90 ml/min/1.73 m2 and AER < 30 mg/24 h, or as G1A1 according to NKF. This rare group of elderly patients was primarily compared with a group of elderly patients with mild kidney impairment (n = 6647; 30.7%), defined as eGFR between 60 and 90 ml/min/1.73 m2 with AER < 30 mg/24 h, or as G2A1 class according to NKF. Secondarily, we compared G1A1 patients with G1A2/3 patients (n = 121), i.e., those with eGFR > 90 ml/min/1.73 m2 but AER ≥ 30 (in mg/g or equivalent).
Study flowchart and degrees of renal impairment. a Study flowchart. b Frequencies of the various degrees of renal impairment in patients aged < 80 years. c Frequencies of the various degrees of renal impairment in patients aged 80 years or older. G classes are determined according to eGFR values in ml/min/1.73 m2: G1 > 90; G2 60–90; G3 30–59; G4 15–29; G5 < 15. A classes are determined according to albuminuria values in mg/g of creatinine or mg/24h: A1 < 30; A2 30–300; A3 > 300
Comparisons between G1A1 and G2A1
The clinical characteristics of patients in the two main groups are summarized in Table 1. Patients with G1A1 versus those with G2A1 were younger by 1.3 years, more prevalently males (58.3 versus 48.7%), with lower BMI (26.6 versus 27.2 kg/m2) and lower triglyceride levels (106.5 versus 117.2 mg/dl). There was no significant difference in blood pressure, glucose control, diabetes duration, frequency or micro- and macroangiopathy. There were also no significant differences in the use of glucose-lowering medications between the two groups. Among other drugs, use of statin was less frequent and use of calcium channel blockers was more frequent in G1A1 versus G2A1 patients.
Gender-specific analysis
Among males, the differences between G1A1 and G2A1 patients remained the same as in the total cohort for age (82.4 ± 2.9 versus 83.5 ± 3.2 years; p < 0.001), BMI (26.2 ± 4.5 versus 27.0 ± 4.0 kg/m2; p = 0.034) and triglycerides (98.0 ± 41.4 versus 111.8 ± 56.7 mg/dl; p = 0.003). In addition, liver enzymes tended to be lower (SGOT 18.0 ± 5.4 versus 18.9 ± 4.8 U/l; p = 0.020–SGPT 16.9 ± 8.6 versus 17.7 ± 8.3; p = 0.058) and AER was significantly lower (mean ± SD 17.1 ± 6.1 versus 18.8 ± 4.7 mg/24 h; median and IQR: 18 IQR 13–22 versus 19 IQR 15–22 mg/24 h; p = 0.019) in G1A1 versus G2A1, even in the normal range.
Among females, similar trends were detected: the difference in age between G1A1 and G2A1 was still statistically significant (82.4 ± 3.2 versus 83.9 ± 3.5 years; p = 0.009), but the differences in BMI (27.2 ± 6.0 versus 27.4 ± 4.8 kg/m2; p = 0.060) and triglycerides (119.9 ± 66.2 versus 122.5 ± 57.9 mg/dl; p = 0.783) were not statistically significant.
There was no significant between-gender heterogeneity in the differences in drug use between the G1A1 and the G1A2 group.
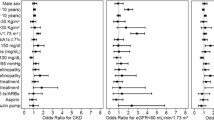
Multivariable analysis
Variables that differed at p < 0.10 between the two groups in Table 1 were entered in a multiple logistic regression analysis to evaluate which was independently associated with normal kidney function (Table 2). To verify whether data missingness affected results of this analysis, we performed MI and repeated the logistic regression analysis on the imputed dataset (Table 2). The variables that were independently associated with normal kidney function in the regression analyses performed with and without MI were age, BMI and triglyceride concentrations. In the original dataset without MI, only 182 (65%) patients in G1A1 and 5182 (78%) in G2A1a had complete data for all variables listed in Table 2. As a consequence of reduced sample size, especially for G1A1, statistical significance for BMI and triglycerides was borderline. Indeed, significance improved by analysing the imputed dataset.
When use of statins and of calcium channel blockers were added to the model, none remained independently associated with normal kidney function in both the original and imputed datasets (not shown).
Comparison between G1A1 and G1A2/3
The clinical characteristics of patients in these two groups are reported in Supplemental Table S1. Patients in the G1A2/3 group, versus those in the G1A1, had lower systolic blood pressure (although with no difference in the use of anti-hypertensive medications), markedly higher levels of liver enzymes, and a less frequent use of DPP-4 inhibitors.
Discussion
In this study, we phenotyped a rare population of elderly individuals with a fully preserved kidney function, despite long-lasting T2D. We elected to compare primarily patients in the G1A1 NKF class versus those with mild renal impairment (G2A1 class) to avoid the confounding factors of fluid retention and use of diuretics that are more frequent in patients with worse degrees of renal dysfunction (CKD stage III or higher). To further screen an ideal normal renal phenotype, we first excluded patients with elevations in AER. The comparison of elderly T2D patients with fully preserved versus those with mildly impaired kidney function identified significant and highly consistent differences in age, BMI, and plasma triglycerides. Since eGFR declines with normal aging, patients with fully preserved kidney function were indeed expected to be relatively younger than those with mild kidney impairment. However, all were aged 80 years or older and the age difference between the two groups was very small compared to the eGFR difference. It is of great interest that, besides age, triglycerides and BMI were the only variables significantly and independently associated with normal kidney function, whereas other known determinants of progressive renal impairment, such as diabetes duration, blood pressure and glycemic control, did not show any association. Furthermore, no robust difference was noted between the two groups in the frequency of other chronic diabetic complications and in the use of a wide range of medications. This observation indicates that the two groups were highly comparable in their natural history, except for kidney function.
A relationship between triglycerides and renal function in T2D has already been identified: in the cross-sectional analysis of the RIACE study, the prevalence of CKD increased by 7–20% for every decile increase in triglyceride concentrations [21]. Triglycerides predicted the development of CKD in a similar population of T2D patients over time [22], and a high triglyceride to HDL cholesterol level was associated with adverse renal outcomes in CKD [23]. However, a recent Mendelian randomization study performed in non-diabetic CKD suggested that genetically higher triglycerides were not associated with kidney function [24].
A possible explanation for the association we detected between fully preserved eGFR and lower BMI would be the presence of sarcopenia that may have resulted in lower creatinine production. However, sarcopenia is not expected to be associated with lower age and with lower plasma triglycerides [25, 26]. Thus, although we do not have a direct measure of insulin resistance, we speculate that lower BMI and lower triglycerides concentrations identifies a condition of better insulin sensitivity in patients with a fully preserved kidney function. In the last decade, it has been recognized that lipotoxicity, as can result from obesity and hypertriglyceridemia, contributes to the development of kidney disease [27]. This can be mediated by ectopic lipid accumulation in the kidney and by the detrimental effects exerted on the glomerular filtration barrier by a deranged humoral milieu including adipokines, cytokines, growth factors, and reactive oxygen species. In T2D, insulin resistance is considered as a major player in the early phases of diabetic kidney disease as well as an accelerator of the decline in glomerular filtration rate [28]. In patients with eGFR > 60 ml/min/1.73 m2, as those included in the present study, insulin resistance may mediate the initial interactions between metabolic and haemodynamic perturbations that trigger kidney disease.
It is remarkable that BMI and triglycerides were determinants of a fully preserved kidney function even in the elderly, independently from glycemic and blood pressure control, and despite a long-lasting diabetes duration. With aging of the general population and of the diabetic population in particular, the clinical phenotyping of normal kidney function can uncover strategies to preserve renal function over time. Since kidney function is a determinant of several health outcomes [29], our data indicate that, even in aged individuals, avoiding lipotoxicity may ultimately translate into reduced morbidity and mortality.
Intriguingly, phenotyping aged patients with micro-/macroalbuminuria despite normal eGFR (G1A2/3) yielded differences versus G1A1 that did not reflect those between G1A1 and G1A2, liver enzymes being the most striking difference. A link between non-alcoholic fatty liver disease, the most common cause of liver enzymes elevation in diabetic patients, and albuminuria or CKD was shown before and has a strong biological rationale [30, 31]. In addition, the less frequent use of DPP-4 inhibitors in aged patients with micro-/macroalbuminuria may lend support to the microvascular protection exerted by these drugs [32], which are particularly suitable for the treatment of T2D in the elderly [33]. Anyway, the comparison between G1A1 and G1A2/3 clearly indicates that eGFR decline and AER increase in aged diabetic patients are most likely determined by distinct pathways.
An additional aim of the present study was to describe the prevalence of the different NFK classes in a large subset of very elderly people with type 2 diabetes from a real-world database. The percent of diabetic patients aged 80 years or older with eGFR < 60 ml/min/1.73 m2, as well as that of normoalbuminuric individuals, was overall superimposable to that reported in other studies [34, 35]. However, we would like to underline that the approach taken by the present study was a non-traditional one, as it addressed a rare healthy phenotype rather than a diseased one. In fact, the group of patients with a fully preserved eGFR despite advanced age and long-standing diabetes represented only 0.4% of the total T2D population and only 1.3% of those aged 80 years or older. In the field of diabetes research, there is a great interest in the search for factors that protect against chronic complications [36], in addition to those that promote their development. A typical study on protective factors in type 1 diabetes is represented by the Joslin Medalist Study [37], but fewer data on protective factors are available for T2D.
This study has limitations. First, glomerular filtration was estimated from a single serum creatinine value and using equations that may not be validated for the elderly population, but for whom alternative estimations of kidney function are not available. It has been shown that the use of a single eGFR measure can lead to a wrong CKD classification in up to 25% of cases [38]. Second, AER was determined on the basis of a single morning urine and had to be converted from different units of measure. This approach, which is routinely applied in epidemiological research [39], may affect the definition of micro- and macro-albuminuria, but it is less prone to false negatives. As a result, some patients may have been incorrectly classified in NKF groups based on single eGFR and AER measure. Finally, a substantial amount of missing data was expected in a retrospective study with automated data extraction where no attempt were made by investigators to fill the gaps, to limit human intervention and data manipulation. In the multiple regression analyses, where only patients with complete data are retained, a MI was needed and we purportedly retained as significant only variables that were significant with both the original and imputed datasets: the most relevant results on the differences in BMI and triglycerides were highly consistent in the analysis of the dataset with or without MI, implying that data missingness was not a major bias in the study results.
On the other side, the study has remarkable strengths. First, the large sample size with nationwide distribution was representative of the T2D population attending diabetes outpatient clinics and allowed for the collection of a non-negligible number of aged individuals belonging to a rare phenotype of fully preserved kidney function. Furthermore, patients were extensively characterized in terms of demographic, biochemical data, complication burden, and medications, with an uncommonly high degree of detail. Finally, automatic data extraction from the same electronic chart at all centers granted uniform data coding, and limited biases derived from data manipulation or data entry into dedicated clinical research forms.
In conclusion, we report that the presence of a fully preserved kidney function is a rare finding in elderly patients with T2D, representing 1.3% of all T2D patients aged 80 years or older. This peculiar population of patients showed lower BMI and lower plasma triglycerides compared with elderly patients with mildly impaired kidney function. These data imply that avoiding lipotoxicity and insulin resistance may be a way to preserve kidney function during aging despite the long-lasting detrimental effects of hyperglycemia. Since even mild reductions in eGFR was previously shown to predict mortality [40], strategies to fully preserve kidney function in the elderly may result in better outcome and even longer lifespan.
References
Mazzola P, Rimoldi SM, Rossi P et al (2016) Aging in Italy: the need for new welfare strategies in an old country. Gerontologist 56:383–390
England K, Azzopardi-Muscat N (2017) Demographic trends and public health in Europe. Eur J Public Health 27:9–13
Lopreite M, Mauro M (2017) The effects of population ageing on health care expenditure: a Bayesian VAR analysis using data from Italy. Health Policy 121:663–674
Vanholder R, Annemans L, Brown E et al (2017) Reducing the costs of chronic kidney disease while delivering quality health care: a call to action. Nat Rev Nephrol 13:393–409
Stevens LA, Li S, Wang C et al (2010) Prevalence of CKD and comorbid illness in elderly patients in the United States: results from the Kidney Early Evaluation Program (KEEP). Am J Kidney Dis 55:S23–S33
Tsai CW, Ting IW, Yeh HC, Kuo CC (2017) Longitudinal change in estimated GFR among CKD patients: a 10-year follow-up study of an integrated kidney disease care program in Taiwan. PLoS One 12:e0173843
Fox CS, Matsushita K, Woodward M et al (2012) Associations of kidney disease measures with mortality and end-stage renal disease in individuals with and without diabetes: a meta-analysis. Lancet 380:1662–1673
Bruck K, Stel VS, Gambaro G et al (2016) CKD prevalence varies across the European general population. J Am Soc Nephrol 27:2135–2147
Pugliese G, Solini A, Bonora E et al (2014) Chronic kidney disease in type 2 diabetes: lessons from the renal insufficiency and cardiovascular events (RIACE) Italian Multicentre Study. Nutr Metab Cardiovasc Dis 24:815–822
Zheng Y, Ley SH, Hu FB (2018) Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat Rev Endocrinol 14:88–98
Canaud B, Tong L, Tentori F et al (2011) Clinical practices and outcomes in elderly hemodialysis patients: results from the dialysis outcomes and practice patterns study (DOPPS). Clin J Am Soc Nephrol 6:1651–1662
Kurella Tamura M, Covinsky KE, Chertow GM, Yaffe K, Landefeld CS, McCulloch CE (2009) Functional status of elderly adults before and after initiation of dialysis. N Engl J Med 361:1539–1547
Thomas B, Matsushita K, Abate KH et al (2017) Global cardiovascular and renal outcomes of reduced GFR. J Am Soc Nephrol 28:2167–2179
Fung CS, Wan EY, Chan AK, Lam CL (2017) Association of estimated glomerular filtration rate and urine albumin-to-creatinine ratio with incidence of cardiovascular diseases and mortality in Chinese patients with type 2 diabetes mellitus—a population-based retrospective cohort study. BMC Nephrol 18:47
Fadini GP, Zatti G, Baldi I et al (2018) Use and effectiveness of dapagliflozin in routine clinical practice: an Italian multicentre retrospective study. Diabetes Obes Metab 20:1781–1786. https://doi.org/10.1111/dom.13280
Fadini GP, Zatti G, Consoli A, Bonora E, Sesti G, Avogaro A (2017) Rationale and design of the DARWIN-T2D (DApagliflozin Real World evIdeNce in Type 2 Diabetes): a multicenter retrospective nationwide Italian study and crowdsourcing opportunity. Nutr Metab Cardiovasc Dis 27:1089–1097
Friedewald WT, Levy RI, Fredrickson DS (1972) Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 18:499–502
Levey AS, Stevens LA, Schmid CH et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150:604–612
National Kidney Foundation (2018) https://www.kidneyorg/professionals/explore-your-knowledge/how-to-classify-ckd. Accessed April 2018
Rubin R (1996) Multiple imputation after 18+ years. J Am Stat Assoc 91:473–489
Penno G, Solini A, Zoppini G et al (2015) Hypertriglyceridemia Is independently associated with renal, but not retinal complications in subjects with type 2 diabetes: a cross-sectional analysis of the renal insufficiency and cardiovascular events (RIACE) Italian Multicenter Study. PLoS One 10:e0125512
Russo GT, De Cosmo S, Viazzi F et al (2016) Plasma triglycerides and HDL-C levels predict the development of diabetic kidney disease in subjects with type 2 diabetes: the AMD annals initiative. Diabetes Care 39:2278–2287
Tsuruya K, Yoshida H, Nagata M et al (2015) Impact of the triglycerides to high-density lipoprotein cholesterol ratio on the incidence and progression of CKD: a longitudinal study in a large Japanese population. Am J Kidney Dis 66:972–983
Lanktree MB, Theriault S, Walsh M, Pare G (2018) HDL cholesterol, LDL cholesterol, and triglycerides as risk factors for CKD: a Mendelian randomization study. Am J Kidney Dis 71:166–172
Scott D, Cumming R, Naganathan V et al (2018) Associations of sarcopenic obesity with the metabolic syndrome and insulin resistance over five years in older men: the concord health and ageing in men project. Exp Gerontol 108:99–105
Ferrara LA, Capaldo B, Mancusi C et al (2014) Cardiometabolic risk in overweight subjects with or without relative fat-free mass deficiency: the strong heart study. Nutr Metab Cardiovasc Dis 24:271–276
Izquierdo-Lahuerta A, Martinez-Garcia C, Medina-Gomez G (2016) Lipotoxicity as a trigger factor of renal disease. J Nephrol 29:603–610
Karalliedde J, Gnudi L (2016) Diabetes mellitus, a complex and heterogeneous disease, and the role of insulin resistance as a determinant of diabetic kidney disease. Nephrol Dial Transpl 31:206–213
Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY (2004) Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med 351:1296–1305
Targher G, Byrne CD (2017) Non-alcoholic fatty liver disease: an emerging driving force in chronic kidney disease. Nat Rev Nephrol 13:297–310
Hwang ST, Cho YK, Yun JW et al (2010) Impact of non-alcoholic fatty liver disease on microalbuminuria in patients with prediabetes and diabetes. Intern Med J 40:437–442
Avogaro A, Fadini GP (2014) The effects of dipeptidyl peptidase-4 inhibition on microvascular diabetes complications. Diabetes Care 37:2884–2894
Tella SH, Rendell MS (2015) DPP-4 inhibitors: focus on safety. Expert Opin Drug Saf 14:127–140
Russo GT, De Cosmo S, Viazzi F et al (2018) Diabetic kidney disease in the elderly: prevalence and clinical correlates. BMC Geriatr 18:38
Solini A, Penno G, Bonora E et al (2013) Age, renal dysfunction, cardiovascular disease, and antihyperglycemic treatment in type 2 diabetes mellitus: findings from the Renal Insufficiency and Cardiovascular Events Italian Multicenter Study. J Am Geriatr Soc 61:1253–1261
Vinik A (2011) The question is, my dear watson, why did the dog not bark? The Joslin 50-year medalist study. Diabetes Care 34:1060–1063
Qi W, Li Q, Gordin D, King GL (2018) Preservation of renal function in chronic diabetes by enhancing glomerular glucose metabolism. J Mol Med (Berl) 96:373–381
Hirst JA, Montes MDV, Taylor CJ et al (2018) Impact of a single eGFR and eGFR-estimating equation on chronic kidney disease reclassification: a cohort study in primary care. Br J Gen Pract 68:e524–e530. https://doi.org/10.3399/bjgp18X697937
Pugliese G, Solini A, Fondelli C et al (2011) Reproducibility of albuminuria in type 2 diabetic subjects. Findings from the renal insufficiency and cardiovascular events (RIACE) study. Nephrol Dial Transpl 26:3950–3954
Penno G, Solini A, Bonora E et al (2018) Defining the contribution of chronic kidney disease to all-cause mortality in patients with type 2 diabetes: the renal insufficiency and cardiovascular events (RIACE) Italian Multicenter Study. Acta Diabetol 55:603–612
Acknowledgements
We wish to thank Alessia Russo, Italian Diabetes Society, for the invaluable technical support.
Agostino Consoli and Gloria Formoso (Dipartimento di Medicina e Scienze dell’Invecchiamento—Università Degli studi G. D’Annunzio di Chieti-Pescara); Giovanni Grossi (Ospedale San Francesco di Paola—Azienda Sanitaria Provinciale di Cosenza); Achiropita Pucci (Azienda Sanitaria Provinciale di Cosenza); Giorgio Sesti and Francesco Andreozzi (Azienda Ospedaliero Universitaria di Catanzaro); Giuseppe Capobianco (Azienda Sanitaria Locale Napoli 2 Nord); Adriano Gatti (Ospedale San Gennaro dei Poveri—Azienda Sanitaria Locale Napoli 1 Centro); Riccardo Bonadonna, Ivana Zavaroni and Alessandra Dei Cas (Azienda Ospedaliero Universitaria di Parma); Giuseppe Felace (Ospedale di Spilimbergo—Azienda per l’Assistenza Sanitaria n.5 Friuli Occidentale); Patrizia Li Volsi (Ospedale di Pordenone—Azienda per l’Assistenza Sanitaria n.5 Friuli Occidentale); Raffaella Buzzetti and Gaetano Leto (Ospedale Santa Maria Goretti—Azienda Sanitaria Locale di Latina); Gian Pio Sorice (Fondazione Policlinico Universitario A. Gemelli, Roma); Paola D’Angelo (Ospedale Sandro Pertini—Azienda Sanitaria Locale Roma 2); Susanna Morano (Azienda Ospedaliera Universitaria Policlinico Umberto I, Roma); Antonio Carlo Bossi (Ospedale di Treviglio—Azienda Socio Sanitaria Territoriale Bergamo Ovest); Edoardo Duratorre (Ospedale Luini Confalonieri di Luino—Azienda Socio Sanitaria Territoriale Sette Laghi); Ivano Franzetti (Ospedale Sant’Antonio Abate di Gallarate—Azienda Socio Sanitaria Territoriale Valle Olona); Paola Silvia Morpurgo (Ospedale Fatebenefratelli—Azienda Socio Sanitaria Territoriale Fatebenefratelli Sacco); Emanuela Orsi (Fondazione IRCCS Ca’ Granda—Ospedale Maggiore Policlinico di Milano); Fabrizio Querci (Ospedale Pesenti Fenaroli di Alzano Lombardo—Azienda Socio Sanitaria Territoriale Bergamo Est); Massimo Boemi† and Federica D’Angelo (Presidio Ospedaliero di Ricerca INRCA-IRCCS di Ancona); Massimiliano Petrelli (Azienda Ospedaliero Universitaria Ospedali Riuniti di Ancona); Gianluca Aimaretti and Ioannis Karamouzis (Azienda Ospedaliero Universitaria Maggiore della Carità di Novara); Franco Cavalot (Azienda Ospedaliero Universitaria San Luigi Gonzaga, Orbassano); Giuseppe Saglietti† (Ospedale Madonna del Popolo di Omegna—Azienda Sanitaria Locale Verbano Cusio Ossola); Giuliana Cazzetta (Casa della Salute, Ugento—Distretto Socio Sanitario Gagliano del Capo—Azienda Sanitaria Locale di Lecce); Silvestre Cervone (Presidio ospedaliero San Marco in Lamis—Distretto Socio Sanitario San Marco in Lamis—Azienda Sanitaria Locale di Foggia); Eleonora Devangelio (Distretto Socio Sanitario di Massafra—Azienda Sanitaria Locale di Taranto); Olga Lamacchia (Azienda Ospedaliero Universitaria Ospedali Riuniti di Foggia); Salvatore Arena (Ospedale Umberto I—Azienda Sanitaria Provinciale di Siracusa); Antonino Di Benedetto (Azienda Ospedaliera Universitaria Policlinico G. Martino di Messina); Lucia Frittitta (Azienda Ospedaliera di Rilievo Nazionale e di Alta Specializzazione Garibaldi di Catania); Carla Giordano (Azienda Universitaria Policlinico Paolo Giaccone di Palermo); Salvatore Piro (Azienda Ospedaliera di Rilievo Nazionale e di Alta Specializzazione Garibaldi di Catania); Manfredi Rizzo, Roberta Chianetta and Carlo Mannina (Azienda Universitaria Policlinico Paolo Giaccone di Palermo); Roberto Anichini (Ospedale San Jacopo di Pistoia—Azienda USL Toscana Centro); Giuseppe Penno (Azienda Ospedaliero Universitaria Pisana); Anna Solini (Azienda Ospedaliera Universitaria Pisana); Bruno Fattor (Comprensorio Sanitario di Bolzano—Azienda Sanitaria della Provincia Autonoma di Bolzano); Enzo Bonora and Massimo Cigolini (Azienda Ospedaliero Universitaria Integrata di Verona); Annunziata Lapolla and Nino Cristiano Chilelli (Complesso Socio Sanitario Ai Colli—Azienda ULSS n.6 Euganea); Maurizio Poli (Ospedale Girolamo Fracastoro di San Bonifacio—Azienda ULSS n.9 Scaligera); Natalino Simioni and Vera Frison (Ospedale di Cittadella—Azienda ULSS n.6 Euganea); Carmela Vinci (Azienda ULSS n.4 Veneto Orientale).
Funding
The study was supported by the Italian Diabetes Society.
Author information
Authors and Affiliations
Consortia
Contributions
Study design: GPF and AS. Data collection and analysis: GPF, AS, AA, GZ, MLM, IK, LF, ADB. Manuscript writing GPF, AS, AA. Manuscript revision GZ, MLM, LF, ADB, IK. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
GPF received Grant support, lecture or advisory board fees from AstraZeneca, Boehringer-Ingelheim, Eli Lilly, NovoNordisk, Sanofi, Genzyme, Abbott, Novartis, Merck Sharp and Dohme. AS received research Grants from Astra Zeneca and served as advisory board member for Boehringer-Ingelheim and Eli-Lilly. ADB received research grants from NovoNordisk and AstraZeneca, and lecture fees from Boehringer-Ingelheim, Eli-Lilly, Sanofi, Lifescan, Menarini diagnostics. LF received research grant from Therascience, lecture or advisory board fees from Eli-Lilly, Novo-Nordisk, Takeda, AstraZeneca. AA received research grants, lecture or advisory board fees from Merck Sharp and Dome, AstraZeneca, Novartis, Boeringher-Ingelheim, Sanofi, Mediolanum, Janssen, NovoNordisk. GZ, MLM and IK declare no conflict of interest.
Ethical standard
The study was approved by ethical committees of participanting Centers and it was conducted in accordance with the ethical standards of the 1964 Declaration of Helsinki.
Informed consent
In agreement with National regulations on data protection and privacy, no informed consent was collected because the database was anonymous.
Additional information
Managed by Massimo Porta.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Fadini, G.P., Solini, A., Manca, M.L. et al. Phenotyping normal kidney function in elderly patients with type 2 diabetes: a cross-sectional multicentre study. Acta Diabetol 55, 1121–1129 (2018). https://doi.org/10.1007/s00592-018-1194-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-018-1194-z