Abstract
Aims
To define the contribution of chronic kidney disease (CKD) to excess mortality in patients with type 2 diabetes and identify the baseline variables associated with all-cause death in those with and without CKD using the RECursive Partitioning and Amalgamation (RECPAM) method.
Methods
This observational, longitudinal, cohort study enrolled 15,773 consecutive non-dialytic patients with type 2 diabetes in 19 Diabetes Clinics throughout Italy in 2006–2008. Based on the presence of albuminuria ≥ 30 mg day−1 and/or estimated glomerular filtration rate (eGFR) < 60 mL min−1·1.73 m−2 at baseline, patients were classified as having or not CKD. Vital status was verified on October 31, 2015 for 99.26% of patients.
Results
Mortality increased with increasing albuminuria and eGFR category. Excess risk versus the general population was maximal in patients aged < 55 years in the worse albuminuria or eGFR category. Conversely, in subjects aged ≥ 75 years with albuminuria < 10 mg day−1 or eGFR ≥ 75 mL min−1·1.73 m−2, excess mortality was no longer detectable. At RECPAM analysis, the main correlates of death in the whole cohort were albuminuria > 44 mg day−1, prevalent CVD, and eGFR < ~ 75 mL min−1·1.73 m−2; gender, prevalent CVD, and higher albuminuria in the normoalbuminuric range, in patients without CKD; and CVD, eGFR ~ < 50 mL min−1·1.73 m−2, and albuminuria > 53 mg day−1, in those with CKD.
Conclusions
CKD is a major contributor to excess mortality in type 2 diabetes, conferring a very high risk in younger patients and fully accounting for excess risk in the older ones. Higher albuminuria and lower eGFR, even in the normal range, identify individuals with increased mortality risk.
Trial registration ClinicalTrials.gov (NCT00715481; https://clinicaltrials.gov/ct2/show/NCT00715481).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes is associated with excess mortality mainly, though not exclusively attributable to an increased risk of cardiovascular disease (CVD) [1]. Death rates have consistently decreased over time in western countries [2,3,4,5,6,7,8], likely due to improved treatment of multiple risk factors, including hyperglycemia, dyslipidemia, and hypertension. Nevertheless, mortality risk remains approximately twice higher in diabetic than in non-diabetic individuals in most studies [1,2,3,4,5, 9].
It is widely recognized that chronic kidney disease (CKD) is a powerful risk factor for CVD since its early pre-dialytic stages, via multiple pathophysiological mechanisms [10]. Data from the general population [11,12,13,14] and patients with type 1 [15, 16] and type 2 [17, 18] diabetes showed that albuminuria and reduced eGFR are independently associated with all-cause and CVD mortality. In addition, CKD was shown to be a major contributor to excess death in both type 1 [16, 19] and type 2 [9, 20] diabetes, possibly as a mediator of the relationship between hyperglycemia and adverse outcomes. However, it is still unclear whether CKD fully accounts for excess mortality and how CKD interacts with CVD risk factors in determining the risk of death in diabetic individuals.
Aim of this study was to further explore the well-established relationship between CKD and mortality by applying the RECursive Partitioning and Amalgamation (RECPAM) method to the large cohort of patients with type 2 diabetes from the Renal Insufficiency And Cardiovascular Events (RIACE) Italian Multicenter Study. Specific aims were to (a) define the extent of the contribution of CKD to excess mortality; and (b) identify the baseline variables associated with all-cause death in patients with and without CKD and their clustering in homogeneous subgroups of subjects with distinct mortality risks.
Materials and methods
Design
The RIACE is an observational, prospective cohort study on the impact of eGFR on morbidity and mortality in patients with type 2 diabetes [21].
Subjects
The RIACE population consists of 15,933 Caucasian patients with type 2 diabetes visiting consecutively 19 hospital-based, tertiary referral Diabetes Clinics of the National Health Service throughout Italy (see Online-only Supplementary Materials) in the years 2006–2008. Exclusion criteria were dialysis or renal transplantation. After excluding 160 patients for missing or implausible values, the remaining 15,773 subjects were analyzed.
The vital status of study subjects on 31 October, 2015 was verified by interrogating the Italian Health Card database (http://sistemats1.sanita.finanze.it/wps/portal/), which provides updated information on all current Italian residents.
Measurements
At baseline, information was obtained on age, smoking status, known diabetes duration, co-morbidities, and current treatments. Body mass index (BMI), BP, and waist circumference were then assessed, and blood samples were obtained for measurements of hemoglobin (Hb) A1c, fasting triglycerides, and total and HDL cholesterol, and calculation of non-HDL and LDL cholesterol [21, 22].
The presence of DKD was assessed by measuring albuminuria and serum creatinine. As previously detailed [21, 23], albumin excretion rate (AER) was obtained from 24-h urine collections or calculated from albumin-to-creatinine ratio in early morning, first-voided urine samples, using a conversion formula developed in patients with type 1 diabetes and preliminarily validated in a subgroup of subjects from the RIACE cohort. Albuminuria was measured in fresh urine samples by immunonephelometry or immunoturbidimetry, in the absence of interfering clinical conditions. One-to-three measurements for each patient were obtained; in cases of multiple measurements, the geometric mean of 2 or 3 values was used for analysis. In subjects with multiple measurements (4062 with at least two and 2310 with three values), concordance rate between the first value and the geometric mean was > 90% for all albuminuria classes [23]. Patients were assigned to one of the following categories of albuminuria (mg day−1): normoalbuminuria (A1, AER < 30), microalbuminuria (A2, AER 30-299), or macroalbuminuria (A3, AER ≥ 300). Normoalbuminuric patients were further divided in those with normal (A1a, AER < 10) and low (A1b, 10–29) albuminuria [24]. Serum (and urine) creatinine was measured by the modified Jaffe method, and eGFR was calculated by the CKD Epidemiology Collaboration equation [25]. Patients were assigned to one of the following categories of eGFR (mL min−1·1.73 m−2): G1 (≥ 90); G2 (60–89); G3 (30–59); G4 (15–29); and G5 (< 15). The G2 and G3 categories were further divided in G2a (75–89) and G2b (60–74) and G3a (45–59) and G3b (30–44), respectively, whereas G4 and G5 categories were pooled together (G4–5). Then, patients were classified as having or not CKD based on the presence or absence of values of albuminuria ≥ 30 mg day−1 and/or eGFR < 60 mL min−1·1.73 m−2.
In each center, the presence of diabetic retinopathy (DR) was assessed by an expert ophthalmologist with dilated fundoscopy. Patients with mild or moderate nonproliferative DR were classified as having non-advanced DR, whereas those with severe nonproliferative DR, proliferative DR, or maculopathy were grouped into the advanced DR category. DR grade was assigned based on the worst eye [26].
Previous major acute CVD events, including myocardial infarction, stroke, foot ulcer/gangrene/amputation, and coronary, carotid, and lower limb revascularization, were adjudicated based on hospital discharge records by an ad hoc committee in each center [27].
Statistical analysis
Data are expressed as mean ± SD or median (interquartile range) for continuous variables, and number of cases and percentage for categorical variables. Continuous variables were compared by one-way ANOVA or the Kruskal–Wallis test in case of parametric and nonparametric distribution, respectively. Pearson’s χ2 was applied to categorical variables.
Crude mortality rates were described as events per 1000 patient-years, with 95% exact Poisson confidence intervals. Mortality among patients with type 2 diabetes from the RIACE cohort was then compared to that of coeval male and female individuals from the Italian general population, as derived from the Italian National Institute of Statistics (ISTAT) life tables during the same time period (2006–2015) [28]. Data were stratified by gender and age category and, within each age category, by AER and eGFR category at baseline.
Kaplan–Meier survival curves for all-cause mortality were calculated according to albuminuria and eGFR categories. Differences in survival rates were analyzed using the log-rank statistic. Survival analyses according to albuminuria and eGFR categories were performed by Cox proportional hazards regression, unadjusted (model 1) or adjusted by gender and baseline age, smoking status, diabetes duration, HbA1c, BMI, waist circumference, triglycerides, total and HDL cholesterol, lipid-lowering treatment, systolic and diastolic BP, anti-hypertensive treatment, retinopathy grade, any CVD, and any cancer (model 2), and also for eGFR and albuminuria categories, respectively (model 3). Results are expressed as HRs and their 95% CIs.
The RECPAM method, which combines the advantages of standard Cox regression and tree-growing techniques, was used to evaluate interactions among covariates and identify homogeneous subgroups of patients with distinct mortality risks in the whole cohort and in subjects with and without CKD [29]. The variables entered into the RECPAM model were those used in the multivariable Cox regression analysis, except LDL cholesterol, which was substituted for total cholesterol. Age was introduced as a global variable, and categorization of values for continuous variables was omitted to allow algorithm-based selection of the natural cut-off points.
Tests were 2-sided, and a P value < 0.05 was considered statistically significant. Statistical analyses were performed using SPSS version 13.0 (SPSS Inc., Chicago, IL) and SAS Software Release 9.4 (SAS Institute, Cary, NC).
Results
Valid information on vital status was retrieved for 15,656 patients (99.26% of the original cohort). The baseline clinical characteristics of these subjects are shown in Supplementary Table 1. Prevalence of normo-, micro-, and macroalbuminuria was 73.20, 22.13, and 4.67%, respectively. Of the normoalbuminuric subjects, 52.27% had normal albuminuria (38.26% of the whole cohort) and 47.73% had low albuminuria (34.94% of the whole cohort). Prevalence of eGFR categories 1, 2, 3, and 4–5 was 36.89%, 45.82% (2a: 27.26%; and 2b: 18.56%), 15.50% (3a: 10.65%; and 3b: 4.85%), and 1.78%, respectively. Prevalence of CKD was 36.33%, 18.94% with albuminuria alone, 9.43% with reduced eGFR alone, and 7.86% with both abnormalities. As compared with patients without CKD, those with CKD were older, more frequently males, and had longer diabetes duration, higher HbA1c, BMI, waist circumference, triglycerides, non-HDL cholesterol, and systolic BP, and lower HDL and LDL cholesterol. Moreover, they had a higher prevalence of DR, CVD, and cancer and were more frequently on treatments.
On 31 October, 2015, 12,054 (76.99%) patients were alive, whereas 3602 (23.01%) patients had deceased (follow-up duration: 7.42 ± 2.05 years, range 0–10.07; death rate: 31.02 per 1000 person-years). Excess mortality in patients with type 2 diabetes from the RIACE cohort was slightly higher in women than in men (1.64 vs. 1.50) and decreased from 3.49- and 2.75-fold, respectively, in those with < 55 years, to 1.19- and 1.30-fold, respectively, in those with ≥75 years of age (Supplementary Table 2).
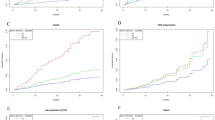
Crude mortality rates increased with increasing albuminuria and eGFR category (Table 1). Likewise, the Kaplan–Meier curves (not shown) and unadjusted Cox proportional hazards regression (model 1; Fig. 1a, d and Supplementary Figure 1A and D) showed a stepwise increase in mortality with increasing albuminuria and eGFR categories/subcategories. When adjusted for several confounders (model 2; Fig. 1b, e and Supplementary Figure 1A and D) and also for each other (model 3; Fig. 1c, f and Supplementary Figure 1B and E), differences in mortality remained across albuminuria categories (including those between normal and low albuminuria) and eGFR categories, except for eGFR G1 and G2 (including G2a and G2b). Other variables independently associated with mortality were age, male gender, current smoking, HbA1c, lipid-lowering treatment, anti-hypertensive treatment, non-advanced and advanced DR, any CVD, any cancer and, inversely, total and HDL cholesterol and diastolic BP; diabetes duration and triglycerides entered only in regression model 2 for albuminuria. Interestingly, the HRs for the worst albuminuria and eGFR categories, even when adjusted for each other, were not lower, if any, than those for prevalent CVD or cancer (Supplementary Tables 3–6). For any albuminuria and eGFR category, the excess risk of all-cause death versus the general population was highest in patients aged < 55 years and decreased progressively with increasing age category. In subjects aged ≥ 75 years with albuminuria < 10 mg day−1 or eGFR ≥ 75 mL min−1·1.73 m−2, excess mortality was no longer detectable, and patients with an eGFR falling in the G1 category appeared to be even protected (Table 2).
Cumulative survival by Cox proportional hazards regression, unadjusted (a, d), adjusted for multiple confounders (b, e) and further adjusted for each other (c, f), according to albuminuria (A1, A2, and A3, a–c) and eGFR (G1, G2, G3, and G4-5, d–f) categories. HRs (95% CI) for mortality are shown for each category. HR hazard ratio, CI confidence interval
RECPAM analysis of the whole cohort identified ten patient subgroups (Fig. 2 and Supplementary Table 7). Among baseline variables, AER was the most relevant correlate of subsequent death, followed by CVD and eGFR. Death was most likely in subjects with AER values > 44 mg day−1 and prevalent CVD (class 1), whereas it was least likely in female patients with values AER ≤ 44 mg day−1, no CVD, and an eGFR > 73 mL min−1·1.73 m−2 (class 10 or reference vs. class 9 for those with an eGFR ≤ 73 mL min−1·1.73 m−2). An eGFR threshold of 79 and 72 mL min−1·1.73 m−2 further separated subjects with AER values > 44 mg day−1 and no CVD and those with AER levels ≤ 44 mg day−1 and CVD, respectively (class 2–class 5). Finally, among male patients with an AER ≤ 44 mg day−1 hours without CVD, further separation was associated with LDL cholesterol values ≤ 83 mg dL−1 (class 6) and, in those with LDL levels above this threshold, with AER values > and ≤ 17 mg day−1 (i.e., within the normoalbuminuric range; class 7 and 8, respectively). In patients without CKD (Fig. 3 and Supplementary Table 8), gender and prevalent CVD were the main correlates of death, with the highest risk in males with previous CVD and an HbA1c > 7.2% (class 1) and the lowest risk in females with no CVD and on lipid-lowering treatment (class 12 or reference). In male subjects without CVD, higher HbA1c, lower LDL cholesterol, and higher AER within the normoalbuminuric range at two cutoffs (15 and 7 mg day−1) identified subjects at higher risk. In female subjects, those with CVD had the highest likelihood of death, whereas among patients without CVD and no lipid-lowering treatment, higher HbA1c and lower LDL cholesterol were associated with higher risk. Also in patients with CKD (Fig. 4 and Supplementary Table 9), CVD was the main correlate of death. In addition, among subjects with and without CVD, an eGFR threshold of ~ 50 mL min−1·1.73 m−2 identified four subgroups with distinct risks of death, the highest of which was in those with CVD and an eGFR below this value (class 1). Among subjects without CVD and an eGFR above this value, other correlates were an AER > or ≤ 53 mg day−1, followed by an HbA1c > or ≤ 8.5% or an HDL cholesterol ≥ and < 42 mg dL−1 and gender, with the lowest risk in females with lower AER and higher HDL cholesterol (class 10 or reference).
RECPAM analysis for identification of patient subgroups with different mortality risks in the whole cohort. The analysis was conducted on patients with calculable LDL cholesterol values. The data in the circles and rectangles represent the number of deaths (upper) and the number of patients (lower) in each subgroup. HRs for mortality with 95% CIs are shown for each class and the global variable (age). RECPAM Results of RECursive Partitioning and Amalgamation, HR hazard ratio, CI confidence interval, AER albumin excretion rate, CVD cardiovascular disease, eGFR estimated glomerular filtration rate, HbA 1c hemoglobin A1c, LDL-C LDL cholesterol
RECPAM analysis for identification of patient subgroups with different mortality risks in the patients without CKD. The analysis was conducted on patients with calculable LDL cholesterol values. The data in the circles and rectangles represent the number of deaths (upper) and the number of patients (lower) in each subgroup. HRs for mortality with 95% CIs are shown for each class and the global variable (age). RECPAM Results of RECursive Partitioning and Amalgamation, CKD chronic kidney disease, HR hazard ratio, CI confidence interval, M males, F females, CVD cardiovascular disease, HbA 1c hemoglobin A1c, LDL-C LDL cholesterol, LLT lipid-lowering treatment, AER albumin excretion rate
RECPAM analysis for identification of patient subgroups with different mortality risks in the patients with CKD. The analysis was conducted on patients with calculable LDL cholesterol values. The data in the circles and rectangles represent the number of deaths (upper) and the number of patients (lower) in each subgroup. HRs for mortality with 95% CIs are shown for each class and the global variable (age). RECPAM Results of RECursive Partitioning and Amalgamation, CKD chronic kidney disease, HR hazard ratio, CI confidence interval, M males, F females, CVD cardiovascular disease, HbA 1c hemoglobin A1c, AER albumin excretion rate, eGFR estimated glomerular filtration rate, HDL-C HDL cholesterol
Discussion
This study provides important new insights into the well-established relationship between CKD and all-cause mortality in patients with type 2 diabetes. The application of RECPAM analysis in addition to standard Cox regression allowed us to analyze in depth the contribution of CKD and its main manifestations, i.e., albuminuria and reduced eGFR, to excess mortality in these individuals as well as their relationship with other known risk factors.
Our study supports the concept that presence and severity of CKD are powerful predictors of all-cause mortality in subjects with type 2 diabetes, with excess risk over non-diabetic individuals decreasing progressively with increasing age for any albuminuria and eGFR category. Indeed, the adjusted risk of death associated with the highest albuminuria or the lowest eGFR category was higher than that attributable to prevalent CVD or cancer, two major determinants of death in diabetic and non-diabetic individuals. In addition, RECPAM analysis showed that increased albuminuria and reduced eGFR are the most relevant correlates of death, together with CVD.
As expected, both albuminuria and reduced eGFR were strongly related to mortality risk. In particular, risk increased linearly with increasing albuminuria, with no threshold, as even increases within the normoalbuminuric range were associated with increased mortality. This finding is consistent with previous meta-analyses [12, 13, 30], post hoc analyses of randomized controlled trials in high-risk individuals [31, 32], community-based cohort studies [33, 34], and the cross-sectional analysis of the RIACE cohort [24] showing a linear relationship with risk for all-cause and CVD mortality as well as CVD events. The importance of increased albuminuria within the normoalbuminuric range was confirmed by the RECPAM analysis of the whole cohort, showing that a level of albuminuria of 17 mg day−1 further discriminated among male patients without previous CVD and with LDL cholesterol values > 83 mg dL−1. Likewise, in patients without CKD, an albuminuria of 15 mg day−1 and then of 7 mg day−1 discriminated among male subjects without CVD and with LDL cholesterol values > 100 mg dL−1. In addition, RECPAM analysis indicated that albuminuria is the main correlate of all-cause mortality in the whole cohort, with a threshold at the lower end of the microalbuminuric range (i.e., 44 mg day−1), likely discriminating between subjects with normoalbuminuria or intermittent microalbuminuria and those with persistent microalbuminuria. Likewise, in patients with CKD, an albuminuria of 53 mg day−1 discriminated among subjects without CVD and with an eGFR > 49 mL min−1·1.73 m−2.
Conversely, risk of death associated with reduced eGFR increased significantly only in patients with values < 60 mL min−1·1.73 m−2, with no difference between G1 and G2 category and also between G2a and G2b. RECPAM analysis showed that this was the case in subjects without CKD, but not in the whole cohort, in which the threshold for increased mortality risk was set at an eGFR level between G2a and G2b (72–79 mL min−1·1.73 m−2), i.e., still in the normal (or non-reduced) range, consistent with a previous report from the general population [13] and the cross-sectional analysis of the RIACE cohort [23]. Moreover, a threshold between G3a and G3b (i.e., 48–49 mL min−1·1.73 m−2) further discriminated among subjects with CKD, no matter whether they had or had not CVD.
Overall, the presence of CKD did not appear to explain all the excess mortality risk conferred by diabetes, except than in older individuals. In fact, in subjects aged < 55 years with normal AER and eGFR values, mortality was still two-to-three fold higher in diabetic than in the general population. Conversely, in patients aged ≥ 75 years falling in the lowest albuminuria or the highest eGFR category, excess mortality over non-diabetic individuals was no longer detectable. This finding is consistent with two recent reports from the Swedish National Diabetes Register showing that, in addition to glycemic control, the presence of CKD is a major determinant of excess risk of death in patients with type 1 [19] and type 2 [20] diabetes.
Other correlates of death were CVD, HbA1c, and lipid parameters. In particular, CVD was the main correlate of death in patients, especially males, with albuminuria in the normoalbuminuria or low microalbuminuria range (i.e., ≤ 44 mg day−1), whereas albuminuria further discriminated among subjects without CVD and eGFR further discriminated among those with and without CVD. Moreover, the surprising finding that LDL cholesterol (in the whole cohort and in subjects without CKD) was inversely related to mortality risk is difficult to explain and requires further investigation. In fact, it does not simply reflect the fact that subjects with lower LDL cholesterol levels were more frequently on lipid-lowering treatment because of a more complicated disease, since it applied also to patients not on statin treatment and only to those without CVD.
Strengths of our study include the large size of the cohort, the completeness of baseline and follow-up data, and the analysis of a contemporary and real-life dataset, and the statistical analysis combining standard Cox regression and RECPAM method. Furthermore, we are confident that our cohort may be representative of non-dialytic patients with type 2 diabetes attending tertiary referral outpatients Diabetes Clinics in Italy. The main limitation is that these individuals do not represent the totality of patients with type 2 diabetes in Italy, as a significant proportion of them is followed by the general practitioner or secondary referral centers. Potential limitations concerning non-centralized measurements of albuminuria and creatinine and the use of funduscopy in the assessment of DR have been extensively addressed in previous reports [21,22,23,24, 26, 27].
In conclusion, this study supports the concept that CKD is a major contributor to all-cause death in type 2 diabetes. Though CKD-related mortality risk is much higher in younger individuals, CKD appears to fully account for excess risk of death associated with type 2 diabetes only in older patients. Higher albuminuria and lower eGFR, even in the normal range, identify individuals with increased mortality risk and further discriminate among subjects with and particularly without CVD.
Abbreviations
- CVD:
-
Cardiovascular disease
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
- CKD:
-
Chronic kidney disease
- eGFR:
-
Estimated glomerular filtration rate
- RECPAM:
-
RECursive Partitioning and Amalgamation
- RIACE:
-
Renal Insufficiency and Cardiovascular Events
- BP:
-
Blood pressure
- BMI:
-
Body mass index
- HbA1c :
-
Hemoglobin A1c
- AER:
-
Albumin excretion rate
- DR:
-
Diabetic retinopathy
- ISTAT:
-
Italian National Institute of Statistics
References
Collaboration Emerging Risk Factors, Seshasai SR, Kaptoge S et al (2011) Diabetes mellitus, fasting glucose, and risk of cause-specific death. N Engl J Med 364:829–841
Gregg EW, Cheng YJ, Saydah S et al (2012) Trends in death rates among U.S. adults with and without diabetes between 1997 and 2006: findings from the National Health Interview Survey. Diabetes Care 35:1252–1257
Preis SR, Hwang SJ, Coady S et al (2009) Trends in all-cause and cardiovascular disease mortality among women and men with and without diabetes mellitus in the Framingham Heart Study, 1950 to 2005. Circulation 119:1728–1735
Lind M, Garcia-Rodriguez LA, Booth GL et al (2013) Mortality trends in patients with and without diabetes in Ontario, Canada and the UK from 1996 to 2009: a population-based study. Diabetologia 56:2601–2608
Eliasson M, Talbäck M, Rosén M (2008) Improved survival in both men and women with diabetes between 1980 and 2004—a cohort study in Sweden. Cardiovasc Diabetol 7:32
Carstensen B, Kristensen JK, Ottosen P, Borch-Johnsen K, Steering Group of the National Diabetes Register (2008) The Danish National Diabetes Register: trends in incidence, prevalence and mortality. Diabetologia 51:2187–2196
Gulliford MC, Charlton J (2009) Is relative mortality of type 2 diabetes mellitus decreasing? Am J Epidemiol 169:455–461
Tsujimoto T, Kajio H, Sugiyama T (2018) Favourable changes in mortality in people with diabetes: US NHANES 1999–2010. Diabetes Obes Metab 20:85–93
Afkarian M, Sachs MC, Kestenbaum B et al (2013) Kidney disease and increased mortality risk in type 2 diabetes. J Am Soc Nephrol 24:302–308
Gansevoort RT, Correa-Rotter R, Hemmelgarn BR et al (2013) Chronic kidney disease and cardiovascular risk: epidemiology, mechanisms, and prevention. Lancet 382:339–352
Astor BC, Hallan SI, Miller ER 3rd, Yeung E, Coresh J (2008) Glomerular filtration rate, albuminuria, and risk of cardiovascular and all-cause mortality in the US population. Am J Epidemiol 167:1226–1234
Chronic Kidney Disease Prognosis Consortium, Matsushita K, van der Velde M et al (2010) Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis. Lancet 375:2073–2081
Fox CS, Matsushita K, Woodward M et al (2012) Associations of kidney disease measures with mortality and end-stage renal disease in individuals with and without diabetes: a meta-analysis. Lancet 380:1662–1673
Astor BC, Matsushita K, Gansevoort RT et al (2011) Lower estimated glomerular filtration rate and higher albuminuria are associated with mortality and end-stage renal disease. A collaborative meta-analysis of kidney disease population cohorts. Kidney Int 79:1331–1340
Groop PH, Thomas MC, Moran JL et al (2009) The presence and severity of chronic kidney disease predicts all-cause mortality in type 1 diabetes. Diabetes 58:1651–1658
Orchard TJ, Secrest AM, Miller RG, Costacou T (2010) In the absence of renal disease, 20 year mortality risk in type 1 diabetes is comparable to that of the general population: a report from the Pittsburgh Epidemiology of Diabetes Complications Study. Diabetologia 53:2312–2319
de Boer IH, Katz R, Cao JJ et al (2009) Cystatin C, albuminuria, and mortality among older adults with diabetes. Diabetes Care 32:1833–1838
Ninomiya T, Perkovic V, de Galan BE et al (2009) Albuminuria and kidney function independently predict cardiovascular and renal outcomes in diabetes. J Am Soc Nephrol 20:1813–1821
Lind M, Svensson AM, Rosengren A (2015) Glycemic control and excess mortality in type 1 diabetes. N Engl J Med 372:880–881
Tancredi M, Rosengren A, Svensson AM et al (2015) Excess mortality among persons with type 2 diabetes. N Engl J Med 373:1720–1732
Penno G, Solini A, Bonora E et al (2011) Clinical significance of nonalbuminuric renal impairment in type 2 diabetes. J Hypertens 29:1802–1809
Penno G, Solini A, Bonora E et al (2013) Gender differences in cardiovascular disease risk factors, treatments and complications in patients with type 2 diabetes: the RIACE Italian multicentre study. J Intern Med 274:176–191
Pugliese G, Solini A, Fondelli C et al (2011) Reproducibility of albuminuria in type 2 diabetic subjects. Findings from the Renal Insufficiency and Cardiovascular Events (RIACE) Study. Nephrol Dial Transpl 26:3950–3954
Penno G, Solini A, Zoppini G et al (2015) Independent correlates of urinary albumin excretion within the normoalbuminuric range in patients with type 2 diabetes: the Renal Insufficiency and Cardiovascular Events (RIACE) Italian Multicentre Study. Acta Diabetol 52:971–981
Levey AS, Stevens LA, Schmid CH et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150:604–612
Penno G, Solini A, Zoppini G et al (2012) Rate and determinants of association between advanced retinopathy and chronic kidney disease in patients with type 2 diabetes: the Renal Insufficiency and Cardiovascular Events (RIACE) Italian multicenter study. Diabetes Care 35:2317–2323
Solini A, Penno G, Bonora E et al (2012) Diverging association of reduced glomerular filtration rate and albuminuria with coronary and noncoronary events in patients with type 2 diabetes: the Renal Insufficiency and Cardiovascular Events (RIACE) Italian Multicenter Study. Diabetes Care 35:143–149
Italian National Institute of Statistics (ISTAT) Life tables of the residents in Italy, 2006–2015. http://demo.istat.it/tvm2016/index.php?lingua=eng. Last accessed 6 Sept 2017
Ciampi A, Hogg SA, McKinney S, Thiffault J (1988) RECPAM: a computer program for recursive partition and amalgamation for censored survival data and other situations frequently occurring in biostatistics. I. Methods and program features. Comput Methods Programs Biomed 26:239–256
Nitsch D, Grams M, Sang Y et al (2013) Associations of estimated glomerular filtration rate and albuminuria with mortality and renal failure by sex: a meta-analysis. BMJ 346:f324
Gerstein HC, Mann JF, Yi Q et al (2001) Albuminuria and risk of cardiovascular events, death, and heart failure in diabetic and nondiabetic individuals. JAMA 286:421–426
Hillege HL, Fidler V, Diercks GF et al (2002) Urinary albumin excretion predicts cardiovascular and noncardiovascular mortality in general population. Circulation 106:1777–1782
Blecker S, Matsushita K, Köttgen A et al (2011) High-normal albuminuria and risk of heart failure in the community. Am J Kidney Dis 58:47–55
Wachtell K, Ibsen H, Olsen MH et al (2003) Albuminuria and cardiovascular risk in hypertensive patients with left ventricular hypertrophy: the LIFE study. Ann Intern Med 139:901–906
Acknowledgements
This research was supported by the Research Foundation of the Italian Diabetes Society (Diabete Ricerca) and the Diabetes, Endocrinology and Metabolism (DEM) Foundation, and by unconditional grants from Eli Lilly, Sigma-Tau, Takeda, Chiesi Farmaceutici, and Boehringer Ingelheim.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
Dr. Penno reported receiving personal fees from Astra-Zeneca, Boehringer Ingelheim, Eli Lilly, and Merck Sharp & Dohme. Dr. Solini reported receiving grant from Astra-Zeneca and personal fees from Boehringer Ingelheim and Eli Lilly. Dr. Bonora reported receiving grants from Astra-Zeneca, Novo Nordisk, Roche, and Takeda and personal fees from Abbot, Astra-Zeneca, Boehringer Ingelheim, Bristol-Myers Squibb, Eli Lilly, Janssen, Merck Sharp & Dohme, Novo Nordisk, Roche, Sanofi-Aventis, and Takeda. Dr. Orsi reported personal fees from Abbot, Astra-Zeneca, Boehringer Ingelheim, Eli Lilly, Lifescan, Novo Nordisk, Sanofi-Aventis, and Takeda. Dr. Trevisan reported receiving personal fees from Astra-Zeneca, Boehringer Ingelheim, Eli Lilly, Janssen, Medtronic, Novartis, Novo Nordisk, and Sanofi-Aventis and grants from Astra-Zeneca, Boehringer Ingelheim, Eli Lilly, Janssen, Novo Nordisk, and Sanofi-Aventis. Dr. Cavalot reported receiving personal fees from Astra-Zeneca, Sanofi-Aventis, and Takeda. Dr. Nicolucci reported receiving grants from Artsana, Astra-Zeneca, Eli Lilly, Novo Nordisk, and Sanofi-Aventis and personal fees from Eli Lilly and Novo Nordisk. Dr. Pugliese reported receiving personal fees from Astra-Zeneca, Boehringer Ingelheim, Eli Lilly, Merck Sharp & Dohme, Mylan, Shire, Sigma-Tau, and Takeda. No other disclosures were reported.
Ethical standard
The study was conducted in accordance with the 1964 Declaration of Helsinki and its later amendments. The study protocol was approved by the locally appointed ethics committees.
Informed consent
Informed consent was obtained from all patients for being included in the study.
Additional information
Managed by Massimo Porta.
A complete list of the RIACE Investigators can be found in the Online-only Supplementary Materials.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Penno, G., Solini, A., Bonora, E. et al. Defining the contribution of chronic kidney disease to all-cause mortality in patients with type 2 diabetes: the Renal Insufficiency And Cardiovascular Events (RIACE) Italian Multicenter Study. Acta Diabetol 55, 603–612 (2018). https://doi.org/10.1007/s00592-018-1133-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-018-1133-z