Abstract
Aims
To assess the prevalence of left ventricular diastolic dysfunction in a population of patients with type 2 diabetes mellitus; to determine correlation of diastolic dysfunction with heart rate and its variability.
Methods
The study included 202 patients with type 2 diabetes mellitus. Echocardiography was performed with special reference to diastolic function, and heart rate variability was analysed using standard deviation of normal RR intervals, root mean square of successive differences and percentage of successive R–R intervals greater than 50 ms (pNN 50 %) in a 24-h electrocardiogram recording.
Results
Diastolic dysfunction is present in 79 % of type 2 diabetes mellitus patients: grade 1 in 52 %, grade 2 in 26 % and grade 3 in 1 % of patients. The subjects with grade 1 diastolic dysfunction had a statistically significantly higher heart rate variability compared with those with grade 2 diastolic dysfunction (LSD, post hoc test, p = 0.001). In the group with diastolic dysfunction, grade 2 reduced heart rate variability was recorded in 83 % of patients (37 and 7 % for grade 1 and normal diastolic function). An increase in the severity of diastolic dysfunction was associated with decreased heart rate variability and increased heart rate.
Conclusion
Progression of diastolic dysfunction is associated with a significantly greater prevalence of reduced heart rate variability, which is accompanied by increased heart rate.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cardiovascular autonomic neuropathy is a sympathetic and parasympathetic system dysfunction. In diabetic patients, cardiac autonomic tone is impaired due to lesions of the small nerve endings with predomination of parasympathetic damage [1], which then results in elevated heart rate and decreased heart rate variability. Result of sympathetic denervation is reduced coronary artery blood flow [2] and myocardial contractility [3]. The prevalence of cardiovascular autonomic neuropathy in diabetic patients varies from 2.6 % to as high as 90 %, averaging 30 % [4, 5]. Clinical manifestations include exercise intolerance, intraoperative cardiovascular instability, tachycardia at rest, orthostatic hypotension and silent ischaemia that leads to myocardial infarction associated with increased mortality. In patients with DM and cardiovascular autonomic neuropathy, the 5-year mortality is four times higher that recorded in DM patients without cardiovascular autonomic neuropathy [6].
Diabetic cardiomyopathy is a myocardial disease caused by DM irrespective of vascular or valvular pathology and arterial hypertension [7]. The pathogenesis of diabetic cardiomyopathy remains obscure. The potential causes include hyperglycaemia [8], hyperlipidaemia, hyperinsulinaemia, and glycolysis stimulation and glucose oxidation defects [9] that lead to structural and functional changes in myocardial cells, which in turn results in undesired myocardial remodelling, thus causing a vicious circle where heart failure increases insulin resistance and vice versa [9]. Recognition of diabetic cardiomyopathy in the early stage of the disease remains a challenge. Increased myocardial density and subendocardium dysfunction are lesions that can earliest be detected on echocardiography, whereas abnormalities in diastolic flow can be detected by tissue Doppler while conventional echocardiography still shows preserved left ventricular systolic function.
The aim of the study was to assess the prevalence of left ventricular diastolic dysfunction (DD) in a population of type 2 DM patients and to investigate the possible association of reduced DD with changes in heart rate variability (HRV) and heart rate.
Methods
The study included 202 type 2 DM patients, in whom diabetes was diagnosed according to the Guidelines of the European Association for the Study of Diabetes from 2007. Patients were collected from the Center for Diabetes Clinic of Internal Medicine, University Hospital Osijek, and the cardiac and diabetic outpatient “Sunce” Policlinic in Zagreb. In accordance with the Declaration of Helsinki, patients meeting the criteria for inclusion in the study received a verbal explanation of the purpose and progress of the study and the Information for potential respondents form, containing written information on all the relevant data pertaining to the study. The respondents’ consent to coercion-free and voluntary participation in the study was confirmed in writing on the Respondent’s informed consent form. Exclusion criteria were left ventricular ejection fraction <50 %, atrial fibrillation or undulation, pacemaker or cardioverter defibrillator implanted, history of myocardial infarction, angina pectoris, left bundle branch block, chronic congestive heart failure, serious valvular or congenital cardiac disease, active myocarditis, severe hepatic or renal disease, and type 1 DM. None of the study patients was being treated with beta blockers. Table 1 shows a basic characteristics of patients.
The detailed history of all study patients was taken. They then underwent a physical examination and 12-lead electrocardiography (ECG). The Bruce protocol exercise stress test was employed to exclude possible coronary disease. The subjects in whom the exercise test indicated a low probability of coronary disease continued the study, and the others were excluded and referred for additional work-up. The study patients underwent a comprehensive transthoracic echocardiographic examination that included two-dimensional imaging in parasternal long- and short-axis view, apical four-, two- and five-chamber view, followed by M-mode imaging and Doppler imaging on a Siemens Acuson Antares Px 4-1 transducer from 2, 3 to 3, 3 MHz and a Siemens Acuson CV 70 P4-2 transducer. The ultrasound was performed by two operators. The following parameters were used for diastolic function evaluation: isovolumic relaxation time (IVRT), pulsed Doppler determination of transmitral inflow (E-wave, A-wave, dt, E/A ratio), spectrogram of pulmonary vein inflow and measurement of myocardial tissue blood flow (E-wave, E/E’ ratio). The left ventricular diastolic function was assessed following the Nagueh criteria recommendations [11]. The mean duration of all beat-to-beat (NN) intervals was determined from 24-h Holter ECG recordings, and HRV was expressed as the standard deviation of interbeat intervals (SDNN), the root mean square of successive differences (RMSSD), and the percentage of successive R–R intervals greater then 50 ms (pNN50 %), mean 24-h heart rate, mean heart rate during daily activities, and mean heart rate during sleep expressed as beats per minute. An Elamedica two-channel digital recorder and a Schiller 200 three-channel digital recorder were used in the study.
Statistical analysis was performed using one-way and two-way analyses of variance, the χ 2-test and Pearson’s correlation coefficient. Data were descriptively expressed by arithmetic mean and standard deviation (SD), as well as by absolute and relative frequency, as needed.
Results
The study included 202 type 2 DM patients meeting the inclusion criteria. There were 123 (61 %) male and 79 (39 %) female patients. Twenty-nine patients (17 male and 12 female) were excluded from the study based on positive exercise test results. The mean age of the study patients was 60.2 years. Correlation of age and DD revealed that patients with normal diastolic function were 3 years younger than those with DD, the difference being significant (post hoc LSD test, p = 0.035). There was no significant difference between the groups of patients with grade 1 and grade 2 DD (post hoc LSD test, p = 0.85). The mean duration of DM in all study patients was 8.9 years. On study entry, there were 35 patients with newly detected DM, while the longest duration of DM was 33 years. Preserved diastolic function was found in 21 % of study patients, while the remaining 79 % had some form of impaired diastolic function: grade 1 DD (impaired relaxation; 52 %), followed by grade 2 (pseudonormalisation; 26 %) and grade 3 (reversible restriction; 1 %). The low number of patients in the last group prevented their inclusion in further statistical analysis. Basic echocardiographic measurements are sublimated in Table 2, and the diastolic function measurement values are shown in Table 3.
A linear correlation was found between the grade of diastolic dysfunction and DM duration. In patients without verified diastolic dysfunction, the mean length of DM was 4.02 years, whereas in those with grade 1, grade 2 and grade 3 diastolic dysfunction, the mean length of DM was 9.2, 12.0 and 19.3 years, respectively. A significantly longer DM duration was recorded in patients with impaired left ventricular relaxation time versus those without DD (post hoc LSD test, p = 0.0007), as well as in patients with grade 2 DD compared to those with grade 1 DD (post hoc LSD test, p = 0.014). Preserved diastolic function had 16 patients with newly diagnosed DM. Decreased HRV was found in 88 study patients (pathologic SDNN <100 ms).
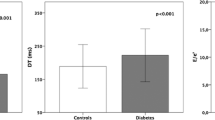
The study subjects were divided into groups with preserved and decreased HRV. The mean length of DM was 6.7 years in patients with preserved HRV and 11.9 years in those with decreased HRV, yielding a significant difference (ANOVA, p < 0.0001). The HRV values are shown in Fig. 1.
Significant differences in HRV were found in DM patients according to the presence and severity of DD. Patients with normal diastolic function had a significantly higher HRV than those with grade 1 and grade 2 DD (post hoc LSD test, p = 0.0002 and post hoc LSD test, p = 0.0000, respectively). Patients with grade 1 DD had a significantly higher HRV compared to those with grade 2 DD (post hoc LSD test, p = 0.001) (Table 4).
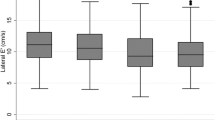
In patients with preserved diastolic function, HRV showed normal distribution, with SDNN of 120–130 ms in most patients. The group of patients with grade 1 DD was divided into two subgroups of subjects with decreased HRV and subjects with normal HRV (bimodal distribution); in this group, normal distribution was still maintained in some patients, whereas in others, it was formed according to pathologic, Poisson distribution. The majority of patients with grade 2 DD showed decreased HRV, usually between 90 and 100 ms, while lower values were less frequently recorded (Fig. 2).
Decreased HRV was recorded in 83 % of patients with grade 2 DD, 37 % of patients with grade 1 DD (post hoc LSD test, p < 0.001) and 7 % of patients with preserved diastolic function (post hoc LSD test, p < 0.001). The difference in the prevalence of HRV between patients with grade 1 DD and patients with normal diastolic function was significant (post hoc LSD test, p < 0.001). The mean SDNN was 121.8 ms in patients free from diastolic dysfunction, 109.2 ms in patients with grade 1 DD and 96.6 ms in patients with grade 2 DD. The mean SDNN was 88.2 ms (SD 8.6) in patients with decreased HRV and 124 ms in those with normal HRV (SD 11.8).
Significant differences were found in 24-h heart rate according to the presence and severity of diastolic function. The mean 24-h heart rate differed statistically significantly between patients without DD and those with grade 1 and grade 2 DD, as well as between patients with grade 1 and grade 2 DD (post hoc LSD test, p < 0.001 all). The mean diurnal heart rate was significantly higher in patients with grade 2 DD versus those with grade 1 DD (post hoc LSD test, p < 0.001). The same level of statistical significance was found for the difference between patients with grade 2 DD and those with preserved diastolic function, while the difference between patients with grade 1 DD and those with normal diastolic function showed a lower level of statistical significance (post hoc LSD test, p = 0.002). The mean nocturnal heart rate yielded no significant differences, irrespective of the grade of DD. The mean circadian (24-h) heart rate was 73.1/min in patients with preserved diastolic function, 77.6/min in patients with grade 1 DD and 81.2/min in patients with grade 2 DD (Fig. 3).
The correlation of HRV and heart rate was tested using Pearson’s correlation coefficient, yielding a significant correlation (p < 0.001) between the mean 24-h heart rate and HRV, whereby the patients with lower HRV had a higher mean heart rate (Pearson’s correlation coefficient, p = −0.64) (Fig. 4).
In addition, there was a significant correlation between the heart rate variability and the mean heart rate during daily activities (p < 0.001), with a significant Pearson’s correlation coefficient (p = −0.62). Significant changes were also recorded in the mean nocturnal heart rate according to the changes in heart rate variability, but with a lower Pearson’s correlation coefficient (p = −0.41).
Discussion
In the study group of type 2 DM patients, impaired relaxation of the left ventricle was most common (52 %), whereas normal diastolic function was found in 21 % and grade 2 diastolic dysfunction, or pseudonormalisation, in 26 % of patients. As there were only three patients with grade 3 diastolic dysfunction (reversible restriction) and such a small sample is a typical example of a small sample on statistical analysis, this sample was excluded from analysis due to impossible calculation of the significance. According to the literature data, pathologic transmitral diastolic inflow is quite usual and expected in DM patients. In a study reported by Poirier et al., diastolic function was assessed in 46 patients with well-controlled type 2 DM, free from clinical signs of coronary disease or hypertension, compensated and with preserved systolic function. Diastolic dysfunction was found in as many as 60 % of patients, 28 % of these with pseudonormal transmitral diastolic recording and 32 % with impaired left ventricular relaxation time [10]. In comparison with the present study, Poirier et al. had a greater proportion of patients without diastolic dysfunction (40 vs. 21 %), but in our study, hypertension was not an exclusion criterion. Poirier et al. included only patients with good glycaemic control, which could explain the result diversity, while hypertension and metabolic disbalance contribute considerably to the development of diastolic dysfunction. Attali et al. [11] investigated the prevalence of diastolic dysfunction in 49 type 1 and type 2 DM patients; however, the changes they recorded in diastolic function did not correlate with patient age, sex, DM duration or the presence of diabetic complications.
Astorri et al. investigated the possible existence of preclinical myocardial lesion in 20 type 1 DM patients, 10 type 2 DM patients and 12 non-DM subjects as a control group. Diastolic function measured by transmitral flow showed a more significant defect of left ventricular filling in type 2 DM compared with type 1 DM patients, whereby all had preserved left ventricular systolic function. The control group showed no impairment of the left ventricular diastolic function. The data obtained on diastolic flow showed a correlation with haemoglobin A1c (HbA1c), patient age and DM duration. The more pronounced diastolic function impairment found in type 2 DM patients was attributed to the presence of initial microangiopathy and borderline autonomic neuropathy in these patients [12].
In our study, 83 % of patients with a pseudonormalised pattern of left ventricular filling had decreased heart rate variability, pointing to a disbalance in neurovegetative response, which leads to patient vulnerability and susceptibility to cardiovascular events, in contrast to patients with normal diastolic function where significantly decreased heart rate variability was found in only 7 % of cases. The severity of diastolic impairment correlated with significant changes in terms of increased heart rate throughout 24-h Holter recording and during daily activities, but without nocturnal heart rate increase. The Pearson’s correlation coefficient yielded a good correlation between heart rate variability decrease and heart rate increase, with the highest correlation recorded for daily activities and during 24-h recording, and the lowest at rest. These results pointed to a possible association of impaired diastolic function as the earliest indicator of diabetic cardiomyopathy and autonomic dysfunction in our patients. The aetiologic factors that lead to diabetic cardiomyopathy and lesions of the autonomic nervous system act simultaneously and synergistically, and thus, a significant decrease in heart rate variability was observed with the progression of diastolic function impairment. An increase in resting heart rate, as a marker of autonomic nervous dysfunction, was found as a significant predictor of metabolic syndrome in non-obese Japanese men [13].
Poanta et al. [14] assessed the existence of both DD and HRV in type 2 DM patients and healthy subjects and found the patients with impaired diastolic relaxation to have a significantly higher heart rate. They conclude that cardiac autonomic neuropathy was associated with DD in patients with type 2 DM, but without clinically manifest heart disease. Rajan and Gokhale found cardiovascular autonomic neuropathy in 56 % of 33 type 1 DM patients, and 12 % of them had impaired left ventricular diastolic but preserved systolic function. All patients with DD also had autonomic neuropathy, but with no correlation of left ventricular systolic dysfunction and diabetic microvascular complications [15]. In another study including 20 type 1 DM patients, the E/A ratio was significantly lower in patients with autonomic neuropathy than in those without it, while the values of cardiovascular autonomic neuropathy measured by endothelin levels correlated with diastolic defect deterioration [16].
Diabetes mellitus is known to increase the morbidity and mortality of patients with heart failure [17]. The Spanish researchers study indicated that DM reduces survival in the non-ischaemic aetiology of heart failure irrespective of the presence or absence of left ventricular systolic dysfunction [18]. It is also known that systolic function is frequently impaired in patients with DM and without cardiovascular diseases [19].
With the advent of new ultrasonographic technologies, the question arises as to whether DD really is the first indicator of diabetic cardiomyopathy. DD diagnosed according to the current recommendations is frequent in patients with DM, but is also influenced by other factors. Systolic strain alteration may be found despite normal diastolic function, indicating that DD should not be considered the first marker of a preclinical form of diabetic cardiomyopathy [20].
Main limitation of the study
The study has a relatively small number of patients. Ageing and hypertension may also participate on the development of impaired diastolic function. Hypertension was not excluding criteria, and mean age in study was 60, 2 years.
Conclusion
Impaired diastolic function was found in 79 % of type 2 DM patients, of which 52 % had impaired relaxation, 26 % had pseudonormalisation, and 1 % had a reversible restriction. With progression of diastolic dysfunction decreases heart rate variability, while the mean 24-h heart rate and diurnal heart rate increase. The progression of diastolic dysfunction is associated with the occurrence of cardiovascular autonomic neuropathy as one of the causes of increased cardiovascular morbidity and mortality in DM patients independent of occurrence of cardiovascular diseases. Active screening for the presence of both entities in diabetic patients is recommended.
References
Bannister R (1998) Autonomic failure. Oxford University Press, A textbook of clinical disorders of autonomic nervous system. Oxford
Stevens MJ, Dayanikli F, Raffel DM, Allman KC, Sandford T, Feldmasn EL, Wieland DM (1998) Scintigraphic assessment of regionalized defects in myocardial sympathetic innervation and blood flow regulation in diabetic patients with autonomic neuropathy. J Am Coll Cardiol 31:1575–1584
Scognamiglio R, Avorago A, Casara D, Crepaldi C, Volta S (1998) Myocardial dysfunction and adrenergic cardiac innervation in patients with insulin-dependent diabetes mellitus. J Am Coll Cardiol 31:404–412
Ziegler D, Gries FA, Supler M (1992) Diabetic cardiovascular autonomic neuropathy multicenter study group: the epidemiology of diabetic neuropathy. J Diabetes Complications 6:49–57
Vinik AI, Maser RE, Mitchell BD (2003) Diabetic autonomic neuropathy. Diabetes Care 26:1553–1558
O’Brien IA, McFadden JP, Corrall RJ (1991) The influence of autonomic neuropathy on mortality in insulin dependent diabetes. Q J Med 79:495–520
Tarquini R, Lazzeri C, Pala L, Rottela CM, Gensini GF (2011) The dyabetic cardiomyopathy. Acta Diabetica 48:173–181
Chatham JC, Seymour AM (2002) Cardiac carbohydrate metabolism in Zucker diabetic fatty rats. Cardiovasc Res 55:104–112
Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA (2009) Recommendation for evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr 22:108–133
Poirier P, Bogaty P, Garneau C, Marois L, Dumensil JG (2001) Diastolic dysfunction in normotensive men with well-controlled type 2 diabetes: importance of maneuvers in echocardiographic screening for preclinical diabetic cardiomyopathy. Diabetes Care 24:5–10
Attali JR, Sachs RN, Valensi P, Palsky D, Tellier P, Vulpillat M (1988) Asymptomatic diabetic cardiomyopathy: a noninvasive study. Diabets Res Clin Pract 4:183–190
Astorri E, Fiorina P, Contini GA, Albertini D, Magnati G, Astorri A (1997) Isolated and preclinical impairment of left ventricular filling in insulin-dependent and non-insulin-dependent diabetic patients. Clin Cardiol 20:536–540
Oda E, Aziawa Y (2014) Resting heart rate predicts metabolic syndrome in apparently healthy non-obese Japanese men. Acta Diabetol 51:85–90
Poanta L, Porojan M, Dumitrascu DL (2011) Heart rate variability and diastolic dysfunction in patients with type 2 diabetes mellitus. Acta Diabetol 46:191–196
Rajan SK, Gokhale SM (2002) Cardiovascular function in patients with insulin-dependent diabetes mellitus: a study using noninvasive methods. Ann NY Acad Sci 958:425–430
Erbas T, Erbas B, Kabakci G, Aksoyek S, Koray Z, Gedik O (2000) Plasma big-endothelin levels, cardiac autonomic neuropathy, and cardiac functions in patients with insulin-dependent diabetes mellitus. Clin Cardiol 23:259–263
Solang L, Malmberg K, Ryden L (1999) Diabetes mellitus and congestive heart failure. Further knowledge needed. Eur Heart J 20:789–795
Varela RA, Shamagain LG, Caballero EB, Ramos PM, Veloso PR, Gonzales-Juanatey RJ (2005) Influence of diabetes mellitus on the survival of patients hospitalized with heart failure: a 12 year study. Eur J Heart Failure 7:859–864
Faganello G, Ciofi G, Faggiano P, Candido R, Tarantini L, De Feo S, Di Lenarda A, de Simone G (2014) Does metabolic syndrome worsen systolic dysfunction in diabetes? The shortwave study. Acta Diabetol. doi:10.1007/s00592-014-0620-0
Ernande L, Bergerot C, Rietzschel ER, De Buyzere ML, Thibault H, Pignonblanc PG, Croisille P, Ovize M, Groisne L, Moulin P, Gillebert TC, Derumeaux G (2011) Diastolic dysfunction in patients with type 2 diabetes mellitus: is it really the first marker of diabetic cardiomyopathy? J Am Soc Echocardiogr 11:1268–1275
Acknowledgments
This study was elaborated within the grant of the European Regional Development Fund—Project FNUSA-ICRC (No. CZ.1.05/1.1.00/02.0123).
Conflict of interest
Jasna Cerkez Habek, Nenad Lakusic, Peter Kruzliak, Jozica Sikic, Darija Mahovic and Luka Vrbanic declare that they have no conflict of interest.
Human and Animal Rights disclosure
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Informed consent disclosure
Informed consent was obtained from all patients for being included in the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Managed by Antonio Secchi.
Rights and permissions
About this article
Cite this article
Habek, J.C., Lakusic, N., Kruzliak, P. et al. Left ventricular diastolic function in diabetes mellitus type 2 patients: correlation with heart rate and its variability. Acta Diabetol 51, 999–1005 (2014). https://doi.org/10.1007/s00592-014-0658-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-014-0658-z