Abstract
Aims
The present study aims to investigate the association between serum ferritin and diabetes, diabetes control, and insulin resistance (IR) and examine whether gender is a modifier for these associations in a community-based sample.
Methods
A cross-sectional survey of 8,235 participants was conducted in 2009. Serum ferritin, glucose, hemoglobin A1c (HbA1c), insulin, inflammatory markers, and lipid markers were measured. IR was estimated with a Homeostasis Model Assessment (HOMA-IR) equation. Multiple logistic and linear regression models were applied to evaluate these associations.
Results
The numbers of diabetic patients and non-diabetic participants in the present study were 644 (7.8 %) and 7,591 (92.2 %). After adjusting for multiple confounders, the odds ratios (ORs) and 95 % confidence intervals (CIs) for diabetes were 1.48 (1.31–1.69) in men and 1.43 (1.24–1.65) in women for one-unit increase in log-transformed serum ferritin levels. Likewise, ORs (95 % CIs) for poor diabetes control (HbA1c ≥7.5 %) were 1.58 (1.21–2.05) and 1.37 (1.07–1.77) in men and women, respectively. As for HOMA-IR, the respective betas (P value) for one-unit increase in log-transformed serum ferritin were 0.07 (P < 0.0001) and 0.06 (P < 0.0001) in men and women.
Conclusions
In conclusion, elevated serum ferritin levels were associated with higher risks of diabetes, higher levels of HbA1c, and HOMA-IR independent of several confounders.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recent studies reported the prevalence of diabetes in China soared from 1.9 to 11.6 % between 1993 and 2010 [1–3]. As a country with the largest population in the world, China has to face the major public health problem with regard to the absolute number and economic burden of potential diabetic patients. Given the consequences of diabetes and its complications, clarifying its etiology, looking for modifiable risk factors, and exploring possible treatment strategies are of paramount importance for diabetes control and prevention.
During the last decades, accumulating evidences were suggestive of elevated serum ferritin concentrations associating with higher risks of diabetes [4–7], insulin resistance (IR) [8], metabolic syndrome [9, 10], and hypertension [11]. Likewise, heme iron intake was also reported to increase the risk of diabetes [12]. Anemia is another big public health problem in many developing countries with the prevalence ranging from 12.7 to 47.4 % [13]. A number of factors might contribute to anemia, but the most important one is iron deficiency [14]. The prevalence of anemia and distribution of ferritin varied between men and women. Previous studies reported that the association between serum ferritin and IR was only found in men but not in women [8]. Thus, we hypothesized that gender might modify the association of ferritin with diabetes risk.
In the present study, we aimed to investigate the association between serum ferritin and diabetes, diabetes control, and IR and examined whether the associations differed by gender in a national representative sample from the China Health and Nutrition Survey (CHNS) 2009.
Methods
Participants
The CHNS [15] started in 1989 and aimed to understand the changes of health status with the follow-up intervals of 2 or 3 years. The CHNS selected individuals from 228 communities and was designed to represent 56 % of China’s population from nine provinces including Liaoning, Shandong, Heilongjiang, Henan, Jiangsu, Hubei, Hunan, Guizhou, and Guangxi. A multistage, random cluster sampling design was used to draw study samples. This survey was approved by the institutional review committees of the University of North Carolina at Chapel Hill, the National Institute of Nutrition and Food Safety, the Chinese Center for Disease Control and Prevention, and the China–Japan Friendship Hospital, Ministry of Health. This study was performed in accordance with the ethical standards laid down in 1964 Declaration of Helsinki and its later amendments. All participants provided written informed consent. Details about the study design were reported elsewhere [15, 16].
In the 2009 wave of CHNS, blood samples were collected and assessed for the first time. In our study, we excluded those with missing information on serum ferritin, glucose, insulin, or other interested variables. Altogether, 8,235 adults aged 18 years and over were included in the analysis.
Data collection
All participants were interviewed by trained physicians and nutritionists using a validated questionnaire to collect demographic, anthropometric, and lifestyle data, which included date of birth, gender, education, height, weight, and smoking. Height and weight were measured by physicians following a standard protocol similar to that developed by the National Center for Health Statistics for the National Health and Nutrition Examination Survey in the USA. Height was measured without shoes and rounded to the nearest 0.1 cm. Weight was recorded in light clothing to the nearest 0.1 kg.
Measurements of glucose, glycated hemoglobin, insulin, and serum ferritin
Blood samples were collected by venipuncture after an overnight fast. Plasma and serum samples were then frozen and stored at −86 °C for laboratory analysis. The samples were analyzed in a national central laboratory in Beijing (medical laboratory accreditation certificate ISO 15189:2007) with strict quality control. Fasting glucose was measured using by the GOD-PAP method (Randox Laboratories Ltd, UK), and glycated hemoglobin (HbA1C) was assessed with high-performance liquid chromatography method. The concentrations of fasting serum ferritin and insulin were determined by a commercial Radioimmunoassay Kit (Beijing North Institute of Biological Technology, China).
Diabetes, diabetes control, and insulin resistance
Diabetes was defined as fasting glucose ≥7.0 mmol/L or current usage of anti-diabetes medications, poor diabetes control was defined as HbA1C ≥7.5 % or 58 mmol/mol IFCC, and IR was estimated with a Homeostasis Model Assessment (HOMA-IR) equation.
Covariates
Body mass index (BMI) was calculated as weight in kilograms divided by squared height in meters. Education level was classified into 0–9, 10–12, and ≥13 years. Smoking status was categorized as never smoker, former smoker, and current smoker. High-sensitivity C-reactive protein (hs-CRP) was analyzed by an automatic clinical chemistry analyzer (Hitachi 7600 D and P model, Japan). Hypertension was defined as systolic blood pressure ≥140 mm Hg, diastolic blood pressure ≥90 mm Hg, or current antihypertensive drug use. Anemia was defined as hemoglobin <130 g/L in men and <120 g/L in women.
Statistical analysis
In the descriptive analysis, we presented the basic characteristics of the study participants as mean (standard deviation) for continuous variables and number (percentage) for category variables by quartiles of serum ferritin. Chi-square test was applied to compare the differences of category variables among the quartiles of serum ferritin, while ANOVA was used for continuous variables. Then we used multivariable logistic regression models to examine the association between serum ferritin and diabetes and poor diabetes control. In the exploratory analysis, we tested the interaction terms between ferritin and other covariates in all participants and found that the interaction terms between gender and low serum ferritin was significant (P < 0.0001). Then we stratified the analysis by gender in the subsequent analysis. Three models were used in the present study. The first model included serum ferritin as an independent variable followed by the second model further adjusting age. The third model additionally included BMI, education, smoking, hsCRP, serum lipids, and hypertension. Additionally, since a linear relationship across the serum ferritin quartiles was observed, serum ferritin was treated as a continuous variable (log-transformed serum ferritin), and odds ratios (ORs) with 95 % confidence intervals (CIs) were calculated with one-unit increase in log-transformed serum ferritin. We applied multivariable linear regression models to investigate the relationship between serum ferritin and HOMA-IR in the whole cohort and presented betas (P values). We also tested whether anemia was significantly associated with diabetes in the whole cohort using multivariable logistic regression models. P values were two-tailed, and P < 0.05 was considered as statistical significance. All analysis was conducted using R 3.0.
Results
Basic characteristics of participants
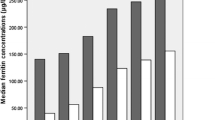
Tables 1, 2 summarize the basic characteristics by quartiles of serum ferritin in men and women, respectively. Because serum ferritin was not normally distributed, log-transformed serum ferritin was used in the following analysis. All basic demographic and metabolic parameters were significantly different among the four quartiles in both men and women except the prevalence of hypertension in men.
Association between serum ferritin and diabetes, diabetes control, and HOMA-IR
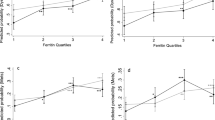
As shown in Table 3, higher serum ferritin levels were associated with a higher risk of diabetes in all models. Compared with participants in the first quartile of serum ferritin, the OR (95 % CI) for those in the fourth quartile was 2.32 (1.65–3.26) in men and 2.30 (1.39–3.80) in women after adjusting for multiple confounders in Model 3. When serum ferritin was treated as a continuous variable, each one-unit increase in log-transformed serum ferritin was associated with 48 % higher risk of diabetes in men (OR 1.48, 95 % CI 1.31–1.69) and 43 % higher risk of diabetes in women(OR 1.43, 95 % CI 1.24–1.65).
Associations between serum ferritin and poor diabetes control in diabetic patients are presented in Table 4. Similar to the results in Table 3, one-unit increase in the log-transformed serum ferritin was associated with 58 % higher risk of poor diabetes control in men and 37 % higher risk of poor diabetes control in women after adjusting for multiple confounders. Likewise, regarding the relationship between serum ferritin and log-transformed HOMA-IR, each one-unit increase in the log-transformed serum ferritin was associated with 0.07 (P < 0.0001) higher of log-transformed HOMA-IR in men. The result was similar in women with effect size being 0.06 (P < 0.0001). The respective prevalence of anemia was 8.5 and 10.5 % (P = 0.2308) in men with and without diabetes, while that of anemia was 18.4 and 19.7 % (P = 0.6151) in women with and without diabetes, respectively. The respective ORs (95 % CI) of diabetes were 1.16 (0.79–1.70) and 1.18 (0.86–1.63) in men and women with anemia after adjusting for multiple confounders. No significant difference between men and women was observed.
Discussion
In the present study with a large sample size, we observed a significant association between serum ferritin levels and the prevalence of diabetes, poor diabetes control, and HOMA-IR in both men and women. Higher serum ferritin levels were associated with a higher risk of diabetes, higher levels of HbA1c and HOMA-IR. These associations were independent of several established confounders and risk factors of diabetes and were slightly different in men than women. The prevalence of anemia was not associated with having diabetes. These findings provided us with new evidence of serum ferritin being regarded as biomarker for diabetes and HOMA-IR.
The overall prevalence of diabetes in this national sample was lower than that previously reported in other surveys [2, 3]. The discrepancy might be largely attributed to the methodology and definition of diabetes as well as age distributions of study populations. Previous surveys used oral glucose tolerance test which is one of the gold standards for diabetes diagnosis, and the participants were mainly the middle and elderly people. In the present study, the study population was younger than those in other studies. In addition to that, diabetes was mainly defined by fasting glucose, which could underestimate the true prevalence of diabetes.
Although several studies were conducted to examine the association between serum ferritin and diabetes, most of them were based on Caucasian samples [17–22]. To the best of our knowledge, only a few studies [7, 9, 23–25] were published to investigate the association in the Chinese population and few of them extensively studied serum ferritin and its association with diabetes, diabetes control, and IR simultaneously. Recent cohort studies reported higher serum ferritin was associated with diabetes incidence in an elderly Chinese population [7] and Korean men [6]. Previous studies also found serum ferritin level is higher in the poorly controlled patients with Type 2 diabetes [26]. Our results were consistent with the aforementioned studies and those conclusions from studies which collected data from Caucasian descent [17–22].
Serum ferritin differed between men and women to a large extent, but the prevalence of diabetes in men and women was comparable. Thus, we hypothesized that gender might have an effect on the association between serum ferritin and diabetes, poor diabetes control, or HOMA-IR. Our results were not contradictory to the hypothesis and were parallel to several studies. In a Japanese study, gender was found to modify the association between serum ferritin and IR [8]. Likewise, a Korean study also found gender might modify the effects of serum ferritin on diabetes and IR [27]. Sex difference of these associations was also reported in the SUNSET Study, which included South Asian Surinamese, African Surinamese, and ethnic Dutch participants [5]. Similar result was also reported in another study, which found elevated serum ferritin concentration was associated with IR only in women with diabetes but not in men [28]. However, although the interaction term between gender and serum ferritin was statistically significant, the differences of the absolute effect sizes in men and women were not too large. Thus, the hypothesis that gender modifies the association of ferritin with diabetes should be interpreted with caution from our results. This might be merely statistical interaction, which does not mean biological interaction between gender and ferritin.
The exact mechanism of the association between serum ferritin and diabetic disorder remains to be clarified. Till now, several possible biological pathways might be proposed to explain the observed findings. Firstly, serum ferritin is regarded as a biomarker of body iron store, whose catalytic effects could induce lipid peroxidation [29]. A recent study suggested lipid peroxidation might be involved in the development of IR [30]. Secondly, iron is able to form highly reactive free radicals [31], which can lead to disturbed glucose metabolism and subsequent hyperglycemia [32]. Additionally, iron deposition and accumulation in hepatocytes may directly involve in insulin signaling [33]. Finally, iron was closely related to inflammation, which imposed a higher risk on diabetes and IR. However, in our study after adjusting for hsCRP, the associations between serum ferritin and diabetes were still significant, which might be suggestive of other pathways of the effects of serum ferritin on diabetes and IR.
The strength of the present study was its large sample size that enabled us to stratify the analysis by gender. Our findings provide new evidence to support the relationship between serum ferritin and diabetes. Admittedly, the current study had some limitations that deserved to be considered when interpreting the results. The cross-sectional study design prevents us from drawing causal inference and highlights the necessity of prospective study with repeated measurements of serum ferritin, glucose, HbA1C, and insulin. In addition to that, the residual confounding is still possible to exist although several confounders were considered in the analysis. Future studies are warranted to clarify the underlying biological mechanisms and causal pathways between serum ferritin and diabetes.
In conclusion, our study suggested that higher serum ferritin was associated with higher prevalence of diabetes, higher levels of HbA1c, and HOMA-IR. The observed results were independent of several confounders including age, gender, education, smoking, BMI, serum lipids, and hypertension.
References
Wang Y, Mi J, Shan XY, Wang QJ, Ge KY (2007) Is China facing an obesity epidemic and the consequences? The trends in obesity and chronic disease in China. Int J Obes (Lond) 31:177–188
Xu Y, Wang L, He J, Bi Y, Li M et al (2013) Prevalence and control of diabetes in Chinese adults. JAMA 310:948–959
Yang W, Lu J, Weng J, Jia W, Ji L et al (2010) Prevalence of diabetes among men and women in China. N Engl J Med 362:1090–1101
Adams PC (2012) Diabetes: serum ferritin levels and T2DM–are body iron stores elevated? Nat Rev Endocrinol 8:573–575
Dekker LH, Nicolaou M, van der AD, Busschers WB, Brewster LM et al (2013) Sex differences in the association between serum ferritin and fasting glucose in type 2 diabetes among South Asian Surinamese, African Surinamese, and ethnic Dutch: the population-based SUNSET study. Diabetes Care 36:965–971
Jung CH, Lee MJ, Hwang JY, Jang JE, Leem J et al (2013) Elevated serum ferritin level is associated with the incident type 2 diabetes in healthy Korean men: a 4 year longitudinal study. PLoS One 8:e75250
Sun L, Zong G, Pan A, Ye X, Li H et al (2013) Elevated plasma ferritin is associated with increased incidence of type 2 diabetes in middle-aged and elderly Chinese adults. J Nutr 143:1459–1465
Pham NM, Nanri A, Yi S, Kurotani K, Akter S et al (2013) Serum ferritin is associated with markers of insulin resistance in Japanese men but not in women. Metabolism 62:561–567
Li J, Wang R, Luo D, Li S, Xiao C (2013) Association between serum ferritin levels and risk of the metabolic syndrome in Chinese adults: a population study. PLoS One 8:e74168
Park SK, Ryoo JH, Kim MG, Shin JY (2012) Association of serum ferritin and the development of metabolic syndrome in middle-aged Korean men: a 5-year follow-up study. Diabetes Care 35:2521–2526
Kim MK, Baek KH, Song KH, Kang MI, Choi JH et al (2012) Increased serum ferritin predicts the development of hypertension among middle-aged men. Am J Hypertens 25:492–497
Bao W, Rong Y, Rong S, Liu L (2012) Dietary iron intake, body iron stores, and the risk of type 2 diabetes: a systematic review and meta-analysis. BMC Med 10:119
Bd Benoist, Mclean E, Egli I, Cogswell M (eds) (2008) Worldwide prevalence of anaemia 1993–2005. World Health Organization, Geneva
Mehdi U, Toto RD (2009) Anemia, diabetes, and chronic kidney disease. Diabetes Care 32:1320–1326
Popkin BM, Du S, Zhai F, Zhang B (2010) Cohort Profile: the China Health and Nutrition Survey–monitoring and understanding socio-economic and health change in China, 1989-2011. Int J Epidemiol 39:1435–1440
Sun X, Du T, Huo R, Xu L (2014) Hemoglobin A1c as a marker for identifying diabetes and cardiovascular risk factors: the China Health and Nutrition Survey 2009. Acta Diabetol 51:353–360
Forouhi NG, Harding AH, Allison M, Sandhu MS, Welch A et al (2007) Elevated serum ferritin levels predict new-onset type 2 diabetes: results from the EPIC-Norfolk prospective study. Diabetologia 50:949–956
Kunutsor SK, Apekey TA, Walley J, Kain K (2013) Ferritin levels and risk of type 2 diabetes mellitus: an updated systematic review and meta-analysis of prospective evidence. Diabetes Metab Res Rev 29:308–318
Wrede CE, Buettner R, Bollheimer LC, Scholmerich J, Palitzsch KD et al (2006) Association between serum ferritin and the insulin resistance syndrome in a representative population. Eur J Endocrinol 154:333–340
Jehn ML, Guallar E, Clark JM, Couper D, Duncan BB et al (2007) A prospective study of plasma ferritin level and incident diabetes: the Atherosclerosis Risk in Communities (ARIC) Study. Am J Epidemiol 165:1047–1054
Fumeron F, Pean F, Driss F, Balkau B, Tichet J et al (2006) Ferritin and transferrin are both predictive of the onset of hyperglycemia in men and women over 3 years: the data from an epidemiological study on the Insulin Resistance Syndrome (DESIR) study. Diabetes Care 29:2090–2094
Gonzalez AS, Guerrero DB, Soto MB, Diaz SP, Martinez-Olmos M et al (2006) Metabolic syndrome, insulin resistance and the inflammation markers C-reactive protein and ferritin. Eur J Clin Nutr 60:802–809
Sun L, Franco OH, Hu FB, Cai L, Yu Z et al (2008) Ferritin concentrations, metabolic syndrome, and type 2 diabetes in middle-aged and elderly Chinese. J Clin Endocrinol Metab 93:4690–4696
Chen T, Ren Y, Liu Y, Long Y, Zhang X et al (2010) Serum gamma-glutamyl transferase, ferritin and the risk of type 2 diabetes in women from a Chinese minority. Diabetes Res Clin Pract 90:352–357
Guo X, Zhou D, An P, Wu Q, Wang H et al (2013) Associations between serum hepcidin, ferritin and Hb concentrations and type 2 diabetes risks in a Han Chinese population. Br J Nutr 110:2180–2185
Batchuluun B, Matsumata T, Erdenebileg N, Tsagaantsooj G, Boldbaatar K et al (2014) Serum ferritin level is higher in poorly controlled patients with Type 2 diabetes and people without diabetes, aged over 55 years. Diabet Med 31:419–424
Kim CH, Kim HK, Bae SJ, Park JY, Lee KU (2011) Association of elevated serum ferritin concentration with insulin resistance and impaired glucose metabolism in Korean men and women. Metabolism 60:414–420
Yu FJ, Huang MC, Chang WT, Chung HF, Wu CY et al (2012) Increased ferritin concentrations correlate with insulin resistance in female type 2 diabetic patients. Ann Nutr Metab 61:32–40
Deray G, Heurtier A, Grimaldi A, Launay Vacher V, Isnard Bagnis C (2004) Anemia and diabetes. Am J Nephrol 24:522–526
Thomas MC, MacIsaac RJ, Tsalamandris C, Power D, Jerums G (2003) Unrecognized anemia in patients with diabetes: a cross-sectional survey. Diabetes Care 26:1164–1169
Emerit J, Beaumont C, Trivin F (2001) Iron metabolism, free radicals, and oxidative injury. Biomed Pharmacother 55:333–339
Wolff SP (1993) Diabetes mellitus and free radicals. Free radicals, transition metals and oxidative stress in the aetiology of diabetes mellitus and complications. Br Med Bull 49:642–652
Messner DJ, Rhieu BH, Kowdley KV (2013) Iron overload causes oxidative stress and impaired insulin signaling in AML-12 hepatocytes. Dig Dis Sci 58:1899–1908
Acknowledgments
This research uses data from CHNS. We thank the National Institute of Nutrition and Food Safety, China Center for Disease Control and Prevention, Carolina Population Center, the University of North Carolina at Chapel Hill, the NIH (R01-HD30880, DK056350, and R01-HD38700) and the Fogarty International Center, NIH for financial support for the CHNS data collection and analysis files from 1989 to 2006 and both parties plus the China–Japan Friendship Hospital, Ministry of Health for support for CHNS 2009, and future surveys.
Conflict of interest
Yiqiang Zhan, Zheng Tang, and Jinming Yu declare that they have no conflict of interest.
Ethical standard
All the authors declare that there is no ethical problem associated with this manuscript.
Human and animal rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Informed consent
Informed consent was obtained from all patients for being included in the study.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Managed by Massimo Federici.
Yiqiang Zhan and Zheng Tang have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Zhan, Y., Tang, Z. & Yu, J. Serum ferritin, diabetes, diabetes control, and insulin resistance. Acta Diabetol 51, 991–998 (2014). https://doi.org/10.1007/s00592-014-0656-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-014-0656-1