Abstract
Aims
We aimed to evaluate the inflammatory profile of individuals with prediabetes defined by HbA1c levels, according to the new American Diabetes Association criteria, and to determine the ability of HbA1c to identify individuals with subclinical inflammation independently of the contribution of other metabolic parameters such as fasting, 1- or 2-h post-load glucose (PG) levels.
Methods
High sensitivity C-reactive protein (hsCRP), erythrocyte sedimentation rate (ESR), fibrinogen, white blood cells (WBC) count and complement C3 (C3) were assessed, and oral glucose tolerance test (OGTT) was performed in 711 adults.
Results
Subjects were stratified into three groups according to their HbA1c levels. Poor agreement existed between HbA1c and 2-h PG criteria for identification of individuals with prediabetes (κ coefficient = 0.300). As compared with subjects having HbA1c <5.7 % (39 mmol/mol), individuals with prediabetes (HbA1c 5.7–6.4 %, [39–46 mmol/mol]) exhibited a significant increase of the concentration of five inflammatory markers (hsCRP, ESR, fibrinogen, WBC count, C3) as well as of a cluster of inflammatory markers, as measured by an inflammatory score after adjusting for sex, age, smoking, fasting, 1- and 2-h PG levels. In multiple regression models including sex, age, body mass index, smoking habit, fasting, 1- and 2-h PG levels, and HOMA index, HbA1c levels were significant independent contributors to each of the five inflammatory markers examined.
Conclusions
These data suggest that HbA1c is a reliable marker of glucose homeostasis, and may identify individuals at increased risk of diabetes with unfavorable inflammatory profile independently from fasting and 2-h PG levels.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence and incidence of type 2 diabetes (T2D) continue to escalate worldwide mainly as consequence of the unceasingly increasing prevalence of obesity [1]. Early identification of subjects at risk of T2D is fundamental not only because the disease is preventable through lifestyle and/or pharmacologic interventions [2–5], but also to prevent or delay the associated cardiovascular complications [6, 7]. Impaired glucose tolerance (IGT) and impaired fasting glucose (IFG) are two glucose metabolism disorders that have been referred to as categories of increased risk of T2D (the so-called prediabetes) as well as for cardiovascular disease [8, 9]. Similarly, several prospective studies that utilize glycated hemoglobin A1c (HbA1c) levels to predict the progression to diabetes have shown a strong, continuous association between HbA1c values and subsequent T2D [10]. In 2010, the American Diabetes Association (ADA) proposed that HbA1c should be used as a diagnostic test for T2D and prediabetes [9]; a HbA1c value of 5.7–6.4 % (39–46 mmol/mol) was identified as a new indicator of prediabetes in addition to IFG and IGT [9]. However, while fasting and post-load glucose, thresholds for the diagnosis of prediabetes have been established in relation to microvascular complications risk, prediabetes thresholds for HbA1c levels have been defined only in relation to the risk of progression to T2D [8, 9]. In addition, the three metabolic parameters employed as measures of dysglycemia, i.e., fasting plasma glucose (FPG), 2-h post-load glucose (PG), and HbA1C reflect different aspects of glucose metabolism with FPG being an indicator of steady-state glucose metabolism, 2-h PG being an indicator of response to glycemic stress, and HbA1c being an indicator of average blood glucose levels over the previous 2–3 months. As a consequence poor concordance between the groups identified by FPG, 2-h PG and HbA1C has been reported in different ethnic groups [11–16]. There is compelling evidence supporting low-grade inflammation as a key component in the pathophysiology of both T2D and cardiovascular disease [17–19]. Among markers of inflammation, the most reliable for clinical practice is high-sensitivity C-reactive protein (hsCRP), but other markers such as white blood cells (WBC) count, complement C3, and fibrinogen have been associated with T2D [20–24]. Associations of prediabetes with low-grade inflammation have been assessed, with IGT robustly associated with inflammatory markers but with less consistent associations among those with prediabetes defined by IFG [25–28]. Therefore, we designed the present study to evaluate the inflammatory profile of individuals with prediabetes defined by HbA1c levels and to determine the ability of HbA1c to identify individuals with low-grade inflammation independently of the contribution of other metabolic parameters in a group of adult white individuals.
Materials and methods
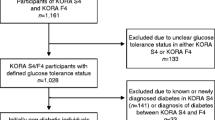
The study sample comprised 711 white individuals participating to the CATAnzaro MEtabolic RIsk factors (CATAMERI) study, a cross-sectional study assessing cardio-metabolic risk factors in subjects carrying at least one risk factor including overweight/obesity, elevated blood pressure (BP), dyslipidemia, dysglycemia, and family history for T2D [16, 27, 29]. Exclusion criteria are specified in the electronic supplementary material. After a 12-h fasting, all individuals underwent anthropometrical evaluation including assessment of body mass index (BMI), waist circumference (WC), and readings of clinic BP obtained in the sitting position, after 5 min of quiet rest. A 75 g oral glucose tolerance test (OGTT) was performed as previously described [16, 27, 29]. Individuals were classified as having normal glucose tolerance (NGT) when FPG was <100 mg/dl and 2-h PG was <140 mg/dl, IGT when FPG was <126 mg/dl and 2-h PG was 140–199 mg/dl, and T2D when FPG was >126 mg/dl and/or 2-h PG> 200 mg/dl or HbA1c> 6.5 % (>48 mmol/mol) [9].
The protocol was approved by the Hospital ethical committee (Comitato Etico Azienda Ospedaliera “Mater Domini”), and written informed consent was obtained from all participants.
Calculations
The homeostasis model assessment (HOMA) index was calculated as fasting insulin × FPG/22.5 [30]. To quantify the inflammatory state, a modification of the inflammatory score proposed by Duncan et al. [17] was generated by attributing one point for a value greater than the median of the study sample for each of the five measured inflammation markers (hsCRP, WBC count, fibrinogen, ESR, and complement C3), and ranged from 0 (lowest median value for each of the four inflammatory markers) to 5 (highest median value for each of the five inflammatory markers).
Statistical analysis
Variables with skewed distribution including triglycerides, hsCRP, ESR, FPG, 1- and 2-h insulin were natural log-transformed for statistical analyses. Continuous data are expressed as mean ± SD. Categorical variables were compared by χ2 test. The κ statistic was calculated as a measure of agreement between HbA1c and 2-h PG diagnoses for individuals at high risk of T2D. Differences in anthropometric, cardio-metabolic, and inflammatory variables between groups were tested after adjusting for age, sex, smoking habit, and BMI using a general linear model with post hoc Bonferroni correction for multiple comparisons. A multivariable linear regression analysis was performed in order to evaluate the independent contribution of the glycemic parameters and other cardio-metabolic risk factors for inflammation. A multivariate logistic regression analysis was used to determine the association between the study groups and the highest values of the inflammatory score. A P value <0.05 was considered statistically significant. All analyses were performed using SPSS software programme version 16.0 for Windows.
Results
The 711 subjects participating to the study were stratified into three groups on the basis of their HbA1c levels, according to the ADA recommendation [9]. Of the individuals who were classified as at increased risk of T2D based on HbA1c levels, 108 (50 %) had NGT, 76 (35.2 %) had IGT, and 32 (14.8 %) had T2D according to the OGTT results. Poor agreement existed between HbA1c and 2-h PG criteria for identification of individuals with prediabetes (κ coefficient = 0.300), with 52.3 % of individuals not having prediabetes by both HbA1 and 2-h PG criteria, and 10.7 % classified as having prediabetes by both HbA1 and 2-h PG criteria.
The characteristics of the subjects stratified by metabolic status based on HbA1c levels are shown in Table 1. Significant differences between the three groups were observed with respect to sex, age, and smoking habit, and therefore, all analyses were adjusted for these variables.
Individuals at increased risk of diabetes (HbA1c 5.7–6.4 %, [39–46 mmol/mol]) had a metabolic risk profile which was intermediate between the one observed in the control group and the one of subjects with T2D (Table 1). After adjusting for age, sex, and smoking habit, individuals at increased risk of diabetes exhibited significantly higher values of all the five inflammatory markers measured, i.e., hsCRP, ESR, fibrinogen, WBC count, and complement C3 as compared with control subjects. The differences between groups in hsCRP, fibrinogen, ESR, WBC count, and complement C3 remained statistically significant (F = 3.93, P = 0.02; F = 3.58, P = 0.009; F = 6.73, P = 0.001; F = 11.46, P < 0.0001; F = 3.45, P = 0.03; and F = 3.45, P = 0.04, respectively) after further adjustment for FPG, 1- and 2-h PG levels in addition to age, sex, and smoking habit.
Adjusting for BMI in addition to age, gender, and smoking habit abolished the association between groups for hsCRP, and fibrinogen (P = 0.24, and P = 0.10, respectively), while the differences between groups for ESR, WBC count, and complement C3 remained statistically significant (F = 5.38, P = 0.005; F = 8.73, P < 0.0001; and F = 6.73, P = 0.001, respectively).
As compared with individuals at increased risk of diabetes, subjects with newly diagnosed T2D exhibited significantly higher FPG, 1- and 2-h PG, HOMA index, and values of hsCRP, fibrinogen, and complement C3, but not of ESR and WBC count.
After adjusting for age, sex, and smoking habit, individuals at increased risk of diabetes (HbA1c 5.7–6.4 %, [39–46 mmol/mol]) exhibited significantly higher values of Inflammation Score as compared with control subjects (Table 1). The difference between groups in Inflammation Score values remained statistically significant after further adjustment for BMI, FPG, 1- and 2-h PG levels, and HOMA index in addition to age, sex, and smoking habit (F = 3.92; P = 0.02).
Furthermore, in multiple regression analysis performed to estimate the contribution of the glycemic parameters and other metabolic risk factors to inflammatory markers, we found that HbA1c levels were significant independent contributors to each of the five inflammatory markers examined (electronic supplementary material).
Next, in order to compare the ability of OGTT and HbA1c criteria to identify subjects with an unfavorable inflammatory profile, we stratified the study population according to OGTT-based glucose tolerance status and HbA1c levels in five groups: NGT and HbA1c < 5.7 % (39 mmol/mol) (control group); NGT and HbA1c 5.7–6.4 % (39–46 mmol/mol); IGT and HbA1c < 5.7 % (39 mmol/mol) (isolated IGT), IGT and HbA1c 5.7–6.4 % (39–46 mmol/mol) and T2D. As shown in Table 2, significant differences between the five groups were observed with respect to sex, age, and smoking habit; therefore, all analyses were adjusted for these variables. As compared to control subjects, both NGT individuals having HbA1c 5.7–6.4 % (39–46 mmol/mol) and individuals with isolated IGT had higher BMI, WC, FPG, 1-h, 2-h PG, fasting and 2 h post-load insulin levels, HOMA index, triglycerides, hsCRP, complement C3, and Inflammation Score after adjusting for sex, age, and smoking habit. By contrast, as compared to control subjects, only NGT individuals having HbA1c 5.7–6.4 % (39–46 mmol/mol), but not individuals with isolated IGT exhibited higher levels of fibrinogen, WBC, and ESR. In addition, as compared to individuals with isolated IGT, those with NGT and HbA1c 5.7–6.4 % (39–46 mmol/mol) had higher WBC and ESR, while levels of fibrinogen, hsCRP and complement C3 were not significantly increased.
A logistic regression model adjusted for age, sex, and smoking habit was used to determine the risk of NGT subjects having HbA1c 5.7–6.4 %, individuals with isolated IGT or combined IGT/HbA1c 5.7–6.4 % and subjects with T2D to have the highest values of the inflammatory score as compared with the NGT and HbA1c < 5.7 % (39 mmol/mol) group (the reference category) (Table 3). The inflammatory score was generated by attributing one point for a value greater than the median of the study sample for each of the five measured inflammation markers (hsCRP, WBC count, fibrinogen, ESR, and complement C3), and ranged from 0 (lowest median value for each of the four inflammatory markers) to 5 (highest median value for each of the five inflammatory markers). For reasons of homogeneity, subjects with an Inflammation Score from 0 to 3 and from 4 to 5 were grouped. Individuals with NGT and HbA1c 5.7–6.4 % and subjects with isolated IGT had a 3.14- and 2.35-fold, respectively, increased risk of having the highest values of the inflammatory score as compared with control subjects. Individuals with combined IGT/HbA1c 5.7–6.4 % had a 2.0-fold increased risk of having the highest values of the inflammatory score, while subjects with T2D exhibited the highest risk (4.38-fold).
Discussion
There is considerable evidence indicating that chronic subclinical inflammation plays a role in the development of both T2D and cardiovascular disease [17–24]. By contrast, whether HbA1c diagnostic thresholds for individuals at increased risk of T2D (prediabetes) (HbA1c 5.7–6.4 % [39–46 mmol/mol]) recently proposed by ADA associate with chronic subclinical inflammation independently from adiposity and other glucose homeostasis parameters is presently less certain [28]. Therefore, in this study, we investigated the impact of ADA new diagnostic criteria for prediabetes on inflammatory profile in 711 subjects without a previous history of diabetes. In agreement with previous studies on adults from different ethnic populations [11–16], we observed a low agreement between diagnoses of high risk of T2D (prediabetes) made by HbA1c and 2-h PG ADA criteria, with 50.0 % of the individuals with HbA1c 5.7–6.4 % (39–46 mmol/mol) classified as not being at high risk by the 2-h PG criterion and 50.9 % of the individuals at high risk by the 2-h PG criterion classified as not being at high risk by the HbA1c criterion.
Additionally, we provide evidence that adults at increased risk of T2D by HbA1c criterion have an unfavorable inflammatory profile as compared with control subjects. Individuals at increased risk of diabetes (HbA1c 5.7–6.4 %, [39–46 mmol/mol]) exhibited a significant increase of five inflammatory markers (hsCRP, ESR, fibrinogen, WBC count, and complement C3) as well as of a cluster of inflammatory markers, as measured by the inflammatory score [17, 27]. By contrast, a recent study focused mainly on assessing leukocyte subtypes in subjects with prediabetes according to HbA1c criterion did not find any difference in hsCRP, and WBC levels between subjects with normal HbA1c values (<5.6 %) and patients with a (pre-)diabetic (>5.6 %) value of HbA1c. The ability to detect significant differences in this former study could have been limited by its small sample size (n = 133) and by the fact that a greater proportion of subjects with HbA1c > 5.6 % was affected by diabetes and treated with pharmacological agents, such as aspirin and statins, which may affect hsCRP levels and WBC [31]. The relationship between FPG and/or 2-h PG with chronic subclinical inflammation has been well established [17–28], but which among the glucose homeostasis parameters (FPG, 1- or 2-h PG, and/or HbA1c) could be a greater independent contributor to chronic subclinical inflammatory state in prediabetic individuals remains elusive. We found that subjects at increased risk of diabetes by HbA1c criterion showed increased values of both individual inflammatory markers and values of the inflammatory score after adjusting for sex, age, smoking habit, FPG, 1- and 2-h PG levels. These data combined with the observation that 50 % of the individuals with HbA1c 5.7-6.4 % (39–46 mmol/mol) were classified as NGT by 2-h PG criterion indicate that HbA1c-based diagnosis of prediabetes may capture at-risk individuals with unfavorable inflammatory profile even when other parameters of glucose metabolism are considered within the normal range. The pathophysiological mechanisms explaining the associations between subclinical inflammation and HbA1c levels are still undefined. Hyper-reaction of the innate immune system may be one of the potential mechanisms underlying the associations observed in the present study because hyperglycemia is sensed by the inflammasome, which functions as a sensor for metabolic stress and induces an inflammatory response by releasing a broad array of cytokines [32]. In fact, hyperglycemia acting through intracellular activation of different metabolic pathways and the accumulation of reactive oxygen species may induce the synthesis and the release of several inflammatory molecules [33]. On the other hand, several studies have reported that higher circulating levels of cytokines such us TNFα may impair insulin signaling and promote hyperglycemia, suggesting that subclinical inflammation plays an important role in the development of diabetes and prediabetes conditions [34–36].
It is well known that the chronic inflammatory state is closely related to obesity. Adipose tissue of overweight/obese subjects produces and releases a number of pro-inflammatory cytokines that may play a role in the development of insulin resistance and glucose intolerance [37, 38]. We observed that adjustment for BMI attenuated the association between HbA1c-based diagnosis of prediabetes and hsCRP, and fibrinogen, two acute-phase response proteins whose expression is induced by interleukin-6 (IL-6). By contrast, the association between HbA1c-based diagnosis of prediabetes and nonspecific markers of inflammation such as ESR, WBC count, and complement C3 remained significant after adjustment for BMI. The marked variation in magnitude of these associations and the effect of confounder such as adiposity highlight the difficulty of characterizing chronic inflammatory state on the basis of a single marker [17, 27, 39]. We have thus chosen to characterize the inflammatory state of individuals at increased risk of diabetes by employing an inflammatory score. This score combines acute-phase reactants such as hsCRP, and fibrinogen with nonspecific markers of inflammation such as ESR, WBC count, and complement C3. We found that individuals at increased risk of diabetes (HbA1c 5.7–6.4 %, [39–46 mmol/mol]) exhibited significantly higher values of Inflammation Score as compared with control subjects even after adjusting for several confounders including sex, age, BMI, smoking habit, FPG, 1- and 2-h PG levels, and HOMA index. Assuming that multiple pathways are likely involved in the relationship between glucose homeostasis and the innate immune system, the use of an integrated measure of several markers conceptually makes sense.
The present study has some strengths including the relatively large sample size encompassing both sexes, the detailed anthropometric and metabolic data collected by trained staff, the simultaneous assessment of FPG, plasma glucose during OGTT, and HbA1c, the centralization of laboratory analyses including a rigorously standardized HbA1c measurement, the assay of biochemical metabolites in fresh blood samples, the exclusion of individuals with conditions that affect red cell turnover, and the exclusion of confounding conditions characterized by elevation in inflammatory markers.
However, our study has potential limitations that merit comment. First, each metabolic test (FPG, A1C, and OGTT) was only performed once. Although such an approach reflects clinical practice and is common in epidemiological studies, the day-to-day variability of FPG and 2-h PG cannot be taken into account and this may have introduced some imprecision in the classification of participants into the glucose tolerance categories. Additionally, analyses of inflammatory markers were performed on fasting samples, and therefore, we may not have fully captured the effects of post-load hyperglycemia on inflammation leading to an underestimation of the strength of the true associations. Furthermore, the use of BMI as a marker of adiposity do not allow us to fully characterize the role of adiposity in determining the levels of the assessed inflammation markers, as would have been possible with detailed body composition data. Moreover, the cross-sectional design of the present study precludes us to draw any conclusions on the role of HbA1c 5.7–6.4 % (39–46 mmol/mol) and related inflammatory status in occurrence of overt T2D, and therefore, a cause–effect relationship cannot be firmly established. Finally, the present findings are only based on white Europeans and should not be extended to other ethnic groups that have been shown to have higher levels of HbA1c likely due to differences in hemoglobin glycation or red cell survival among ethnic groups [40, 41]. Additional studies should thus be performed in other ethnicities and in patients following a different dietary regimen and lifestyle in order to confirm our results.
In conclusion, the present data suggest that HbA1c is a reliable marker of glucose homeostasis and may be of help in the identification of individuals at increased risk of diabetes with unfavorable inflammatory profile independently from other glucose homeostasis parameters.
References
International Diabetes Federation (2011) Global Burden: prevalence and projections, 2011 and 2030. http://www.diabetesatlas.org/content/diabetes-and-impaired-glucose-tolerance
Tuomilehto J, Lindström J, Eriksson JG, Valle TT, Hämäläinen H, Ilanne-Parikka P, Keinänen-Kiukaanniemi S, Laakso M, Louheranta A, Rastas M, Salminen V, Uusitupa M, Finnish Diabetes Prevention Study Group (2001) Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 344:1343–1350
Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, Nathan DM, Diabetes Prevention Program Research Group (2002) Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 346:393–403
Chiasson JL, Josse RG, Gomis R, Hanefeld M, Karasik A, Laakso M, STOP-NIDDM Trail Research Group (2002) Acarbose for prevention of type 2 diabetes mellitus: the STOP-NIDDM randomised trial. Lancet 359:2072–2077
DeFronzo RA, Tripathy D, Schwenke DC, Banerji M, Bray GA, Buchanan TA, Clement SC, Henry RR, Hodis HN, Kitabchi AE, Mack WJ, Mudaliar S, Ratner RE, Williams K, Stentz FB, Musi N, Reaven PD, ACT NOW Study (2011) Pioglitazone for diabetes prevention in impaired glucose tolerance. N Engl J Med 364:1104–1115
Chiasson JL, Josse RG, Gomis R, Hanefeld M, Karasik A, Laakso M, STOP-NIDDM Trial Research Group (2003) Acarbose treatment and the risk of cardiovascular disease and hypertension in patients with impaired glucose tolerance: the STOP-NIDDM trial. JAMA 290:486–494
Ratner R, Goldberg R, Haffner S, Marcovina S, Orchard T, Fowler S, Temprosa M, Diabetes Prevention Program Research Group (2005) Impact of intensive lifestyle and metformin therapy on cardiovascular disease risk factors in the diabetes prevention program. Diabetes Care 28:888–894
Nathan DM, Davidson MB, DeFronzo RA, Heine RJ, Henry RR, Pratley R, Zinman B, American Diabetes Association (2007) Impaired fasting glucose and impaired glucose tolerance: implications for care. Diabetes Care 30:753–759
American Diabetes Association (2014) Standards of medical care in diabetes-2014. Diabetes Care 37(Suppl 1):S14–S81
Selvin E, Steffes MW, Zhu H, Matsushita K, Wagenknecht L, Pankow J, Coresh J, Brancati FL (2010) Glycated hemoglobin, diabetes, and cardiovascular risk in nondiabetic adults. N Engl J Med 362:800–811
Mann DM, Carson AP, Shimbo D, Fonseca V, Fox CS, Muntner P (2010) Impact of HbA1c screening criterion on the diagnosis of pre-diabetes among US adults. Diabetes Care 33:2190–2195
Mohan V, Vijayachandrika V, Gokulakrishnan K, Anjana RM, Ganesan A, Weber MB, Narayan KM (2010) A1C cut points to define various glucose intolerance groups in Asian Indians. Diabetes Care 33:515–519
Olson DE, Rhee MK, Herrick K, Ziemer DC, Twombly JG, Phillips LS (2010) Screening for diabetes and pre-diabetes with proposed A1C-based diagnostic criteria. Diabetes Care 33:2184–2189
James C, Bullard KM, Rolka DB, Geiss LS, Williams DE, Cowie CC, Albright A, Gregg EW (2011) Implications of alternative definitions of prediabetes for prevalence in U.S. adults. Diabetes Care 34:387–391
Lorenzo C, Wagenknecht LE, Hanley AJ, Rewers MJ, Karter AJ, Haffner SM (2010) A1C between 5.7 and 6.4% as a marker for identifying pre-diabetes, insulin sensitivity and secretion, and cardiovascular risk factors: the Insulin Resistance Atherosclerosis Study (IRAS). Diabetes Care 33:2104–2109
Marini MA, Succurro E, Castaldo E, Cufone S, Arturi F, Sciacqua A, Lauro R, Hribal ML, Perticone F, Sesti G (2012) Cardiometabolic risk profiles and carotid atherosclerosis in individuals with prediabetes identified by fasting glucose, postchallenge glucose, and hemoglobin A1c criteria. Diabetes Care 35:1144–1149
Duncan BB, Schmidt MI, Pankow JS, Ballantyne CM, Couper D, Vigo A, Hoogeveen R, Folsom AR, Heiss G, Atherosclerosis Risk in Communities Study (2003) Low-grade systemic inflammation and the development of type 2 diabetes. The Arteriosclerosis risk in communities study. Diabetes 52:1799–1805
Perticone F, Maio R, Sciacqua A, Andreozzi F, Iemma G, Perticone M, Zoccali C, Sesti G (2008) Endothelial dysfunction and CRP are risk factors for diabetes in essential hypertension. Diabetes 57:167–171
Collaboration Emerging Risk Factors, Kaptoge S, Di Angelantonio E et al (2012) C-reactive protein, fibrinogen, and cardiovascular disease prediction. N Engl J Med 367:1310–1320
Ridker PM, Wilson PW, Grundy SM (2004) Should C-reactive protein be added to metabolic syndrome and to assessment of global cardiovascular risk? Circulation 109:2818–2825
Schmidt MI, Duncan BB, Sharrett AR, Lindberg G, Savage PJ, Offenbacher S, Azambuja MI, Tracy RP, Heiss G (1999) Markers of inflammation and prediction of diabetes mellitus in adults (Atherosclerosis Risk in Communities study): a cohort study. Lancet 353:1649–1652
Ford ES (2002) Leukocyte count, erythrocyte sedimentation rate, and diabetes incidence in a national sample of US adults. Am J Epidemiol 155:57–64
Engstrom G, Hedblad B, Eriksson KF, Janzon L, Lindgärde F (2005) Complement C3 is a risk factor for the development of diabetes: a population-based cohort study. Diabetes 54:570–575
Twig G, Afek A, Shamiss A, Derazne E, Tzur D, Gordon B, Tirosh A (2013) White blood cells count and incidence of type 2 diabetes in young men. Diabetes Care 36:276–282
Festa A, D’Agostino R Jr, Tracy RP, Haffner SM (2002) C-reactive protein is more strongly related to post-glucose load glucose than to fasting glucose in non-diabetic subjects; the Insulin Resistance Atherosclerosis Study. Diabet Med 19:939–943
Cardellini M, Andreozzi F, Laratta E, Marini MA, Lauro R, Hribal ML, Perticone F, Sesti G (2007) Plasma interleukin-6 levels are increased in subjects with impaired glucose tolerance but not in those with impaired fasting glucose in a cohort of Italian Caucasians. Diabetes Metab Res Rev 23:141–145
Sesti G, Fiorentino TV, Succurro E, Perticone M, Arturi F, Sciacqua A, Perticone F (2014) Elevated 1-hour post-load plasma glucose levels in subjects with normal glucose tolerance are associated with unfavorable inflammatory profile. Acta Diabetol [Epub ahead of print]
Sabanayagam C, Shankar A, Lim SC, Lee J, Tai ES, Wong TY (2011) Serum C-reactive protein level and prediabetes in two Asian populations. Diabetologia 54:767–775
Succurro E, Arturi F, Lugarà M, Grembiale A, Fiorentino TV, Caruso V, Andreozzi F, Sciacqua A, Hribal ML, Perticone F, Sesti G (2010) One-hour postload plasma glucose levels are associated with kidney dysfunction. Clin J Am Soc Nephrol 5:1922–1927
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Flammer AJ, Gössl M, Li J, Matsuo Y, Reriani M, Loeffler D, Simari RD, Lerman LO, Khosla S, Lerman A (2012) Patients with an HbA1c in the prediabetic and diabetic range have higher numbers of circulating cells with osteogenic and endothelial progenitor cell markers. J Clin Endocrinol Metab 97:4761–4768
Schroder K, Zhou R, Tschopp J (2010) The NLRP3 inflammasome: a sensor for metabolic danger? Science 327:296–300
Fiorentino TV, Prioletta A, Zuo P, Folli F (2013) Hyperglycemia-induced oxidative stress and its role in diabetes mellitus related cardiovascular diseases. Curr Pharm Des 19:5695–5703
Hotamisligil GS, Shargill NS, Spiegelman BM (1993) Adipose expression of tumor necrosis factor-alpha: direct role in obesity-linked insulin resistance. Science 259:87–91
Federici M, Hribal ML, Menghini R, Kanno H, Marchetti V, Porzio O, Sunnarborg SW, Rizza S, Serino M, Cunsolo V, Lauro D, Mauriello A, Smookler DS, Sbraccia P, Sesti G, Lee DC, Khokha R, Accili D, Lauro R (2005) Timp3 deficiency in insulin receptor-haploinsufficient mice promotes diabetes and vascular inflammation via increased TNF-alpha. J Clin Invest 115:3494–3505
Tripathy D, Daniele G, Fiorentino TV, Perez-Cadena Z, Chavez-Velasquez A, Kamath S, Fanti P, Jenkinson C, Andreozzi F, Federici M, Gastaldelli A, Defronzo RA, Folli F (2013) Pioglitazone improves glucose metabolism and modulates skeletal muscle TIMP-3-TACE dyad in type 2 diabetes mellitus: a randomised, double-blind, placebo-controlled, mechanistic study. Diabetologia 56:2153–2163
Hotamisligil GS, Arner P, Caro JF, Atkinson RL, Spiegelman BM (1995) Increased adipose tissue expression of tumor necrosis factor-alpha in human obesity and insulin resistance. J Clin Invest 95:2409–2415
Mohamed-Ali V, Goodrick S, Rawesh A, Katz DR, Miles JM, Yudkin JS, Klein S, Coppack SW (1997) Subcutaneous adipose tissue releases interleukin-6, but not tumor necrosis factor-alpha, in vivo. J Clin Endocrinol Metab 82:4196–4200
Daniele G, Guardado Mendoza R, Winnier D, Fiorentino TV, Pengou Z, Cornell J, Andreozzi F, Jenkinson C, Cersosimo E, Federici M, Tripathy D, Folli F (2014) The inflammatory status score including IL-6, TNF-α, osteopontin, fractalkine, MCP-1 and adiponectin underlies whole-body insulin resistance and hyperglycemia in type 2 diabetes mellitus. Acta Diabetol 51(1):123–131
Herman WH, Ma Y, Uwaifo G, Haffner S, Kahn SE, Horton ES, Lachin JM, Montez MG, Brenneman T, Barrett-Connor E, Diabetes Prevention Program Research Group (2007) Differences in A1C by race and ethnicity among patients with impaired glucose tolerance in the Diabetes Prevention Program. Diabetes Care 30:2453–2457
Herman WH, Cohen RM (2012) Racial and ethnic differences in the relationship between HbA1c and blood glucose: implications for the diagnosis of diabetes. J Clin Endocrinol Metab 97:1067–1072
Conflict of interest
T. V. Fiorentino, M. L. Hribal, M. Perticone, F. Andreozzi, A. Sciacqua, F. Perticone, G. Sesti declare that they have no conflict of interest.
Human and Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Informed Consent
Informed consent was obtained from all patients for being included in the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Managed by Massimo Porta.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Fiorentino, T.V., Hribal, M.L., Perticone, M. et al. Unfavorable inflammatory profile in adults at risk of type 2 diabetes identified by hemoglobin A1c levels according to the American Diabetes Association criteria. Acta Diabetol 52, 349–356 (2015). https://doi.org/10.1007/s00592-014-0647-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-014-0647-2