Abstract
Purpose
The purpose of this prospective randomized controlled trial was to compare the clinical outcome and the survival rate of total knee arthroplasty between CT- and MRI-based patient-specific instrumentation 5 years after initial surgery.
Methods
At a mean follow-up of 5.8 years (SD 0.3), 98 patients (64% women, loss to follow-up 28%) were included in this analysis. To assess the differences in clinical outcome, patients fulfilled PROMs preoperatively and at each follow-up moment. At final follow-up, the Forgotten Joint Score was adjusted.
Results
At final follow-up, no new patients underwent revision surgery in both groups. Regarding the clinical outcome, no statistically significant difference between the groups was found. The Forgotten Joint Score was only performed at final follow-up and showed no significant difference between both groups.
Conclusion
At mid-term follow-up, survival rates between CT- and MRI-based patient-specific instrumentation did not show a significant difference. Regarding clinical outcome, only the EQ-5D-VAS (p < 0.040) showed a statistically significant difference over time, in favor of the MRI-group.
Level of evidence
Level I.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In the treatment of advanced osteoarthritis of the knee joint, total knee arthroplasty (TKA) is the most commonly performed method [1]. Multiple techniques are developed for the optimization of pre-operative planning of TKA. Patient-specific instrumentation (PSI) is one of these methods [2, 3]. This technique uses computed tomography (CT) scans or magnetic resonance imaging (MRI) preoperatively to create patient specific jigs. These jigs are used during surgery and have one possible position on the native anatomy of the knee joint [2].
The method of image acquisition is not standardized among the different PSI manufacturers. Previous studies with only short-term outcomes suggest that MRI-based PSI shows less radiological outliers. No differences in the clinical outcome or survival of the prosthesis were found [4,5,6,7,8,9]. A recent systematic literature review and meta-analysis confirmed this finding [10]. To our knowledge, no randomized controlled trial (RCT) described the differences between CT- and MRI-based PSI concerning the clinical outcome and survival with mid-term follow-up.
This RCT is a continuation of previously published studies that compared 137 patients who underwent TKA with either CT- or MRI-based PSI [5, 9]. These same patients have now been followed up 5 years postoperatively. We hypothesized that there would be no statistically significant difference in implant survival rate and clinical outcome between CT- and MRI-based PSI at 5-year follow-up.
Material and method
This single-center, prospective, randomized, single-blind controlled trial was conducted from June 2014 till February 2015. A total of 137 knees in 137 patients were analyzed in this study, randomized with an allocation of 1:1 and underwent TKA with either CT- or MRI-based PSI. Patients’ recruitment, baseline characteristics, randomization, surgical procedure, peri-operative data and postoperative radiological outliers were described in detail in the first article [9]. Subsequently, differences regarding clinical outcome and survival of the prosthesis at 2-year follow-up were defined in another article [5].
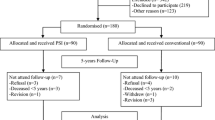
At a mean follow-up of 5.8 years (SD 0.3, 95% CI 5.71–5.88), 98 patients (64% women, 28% loss to follow-up) were included in this analysis. Eleven patients (MRI = 6, CT = 5) died of causes unrelated to the TKA surgery. Between the 2- and 5-year follow-up, 21 patients (MRI = 10, CT = 11) refused to participate any further, mostly since they did not want to fulfill the questionnaires. An overview of the number of patients at the latest follow-up analyzed in this study is presented in Fig. 1.
Due to the SARS-CoV-2 pandemic, collecting patients’ data was performed differently compared to previous follow-up moments. Most patients were not able to, or allowed to visit the outpatient clinic. Therefore, no X-rays were obtained and no physical examination was performed. As an alternative all patients were contacted by phone to ask if revision surgery was performed. In addition, they received an envelope containing the different PROMs with the request to complete and return these forms. The PROMs used were: the 12-item Oxford Knee Score (OKS; 12–60, 12 being the highest score) [11], the Western Ontario and McMaster University Index (WOMAC; 0–100, 100 being the highest score) [12], a Visual Analog Scale for pain (VAS; 0–100, 100 being the highest) [13], the Forgotten Joint Score (FJS-12; 0–100, 100 being the highest) [14] and the EuroQol (EQ-5D; 1,000 being the highest score). For the EQ-5D, a single summary index was calculated using the value set for the Netherlands [15]. Scores on the PROMs were compared between both groups at the different follow-up visits.
This study was approved by the Independent Review Board (IRB Zuyd Heerlen, the Netherlands; IRB-Nr. 13T14) and registered online at the Dutch Trial Register (Nr. NTR4734). Written informed consent was obtained from all individual participants included in the study.
Statistical analysis
The statistical analysis was performed using SPSS software version 26.0 (SPSS Inc., Chicago, Illinois). The primary study was powered with a two-sided 5% significance level and a power of 80%. Based on this calculation, 70 patients per group were included. Since no new patients underwent revision surgery, we did not perform a new survival analysis.
A generalized linear mixed model (GLMM) was used to assess clinical outcome using PROMs with repeated-measures. For each item, the mean, 95%-CI and SD as well as the p value for the latest follow-up and the p value over time were calculated. A p value was considered to be statistically significant when p ≤ 0.05.
Results
At the final follow-up, one patient in the CT-group who already underwent revision surgery at 2-year follow-up underwent a new revision due to dissatisfying results caused by a continuance of experiencing pain and instability. No other revisions were performed in both groups.
Regarding clinical outcome, only the EQ-5D-VAS (p < 0.040) showed a statistically significant difference over time, in favor of the MRI-group (Table 1). The Forgotten Joint Score was only performed at the 5-year follow-up and showed no significant difference between both groups (Table 2).
Discussion
The most important finding of the present study was that at 5-year follow-up patients’ satisfaction was comparable between those operated with use of CT- and MRI-based PSI for TKA. Only the EQ-5D-VAS showed a statistically significant difference between the groups in favor of the MRI-group. Baseline characteristics between both groups did not differ in the primary study. Possibly patients developed new comorbidities disproportionately between both groups, what could explain this difference. No new patients underwent revision surgery between 2- and 5-year follow-up.
In the primary article, differences between both groups regarding adequate positioning of the prosthesis in the coronal and sagittal plane were described [9]. In the current literature, these differences in postoperative alignment between comparable groups are well known [10, 16]. Published mid- or long-term clinical results on PSI comparing CT- and MRI-based PSI are scarce. To our knowledge, there is only one other available study by Kang et al. that studied clinical outcome at 2 years follow-up between CT- and MRI-based PSI in a prospective RCT besides the previous study of this paper [17]. Although this study reported similar outcomes to those in the present study, it reported on a posterior stabilized cemented total knee system, while we used a cruciate retaining total knee system. To our knowledge, there are no previous articles describing differences in survival of the prosthesis at mid-term between both groups at any follow-up moment.
Regarding the clinical outcome, we used multiple PROMs and at 5-year follow-up the FJS-12 was added. This scoring system assesses how natural the prosthesis feels after TKA and thus on what grade patients have “forgotten” they’ve had a joint replacement [14]. The FJS-12 is already increasingly reported as a PROM in the current literature. Recently, a validation study confirmed adequate measurement properties. This study shows the increased reliability of the measurement instrument, and therefore, it is a valuable addition to the present study [18, 19]. Much discussion remains on whether PROMs are the most adequate measurement tool to assess clinical outcome after TKA [20,21,22]. The main reason for this discussion is that the majority of the commonly used PROMs after TKA only meet the minimal requirements for psychometric validity. Therefore, further validation studies are required to ensure a more reliable use of PROMs in the evaluation of TKA [23, 24]. Besides PROMs, wearable motion sensors are increasingly used to assess the clinical outcome following TKA. These are believed to improve the understanding of recovery after surgery. At this moment, studies regarding wearable motion sensors lack consistency [25]. Further research is necessary and may consist of a combination of PROMs and wearable motion sensors for optimal evaluation of clinical outcome after TKA.
At 5-year follow-up, no new patients underwent revision surgery. The primary article described significantly fewer outliers for only tibial slope with the MRI-based PSI [9]. A deviation of > 3° from preoperatively planned (for the Biomechanical-axis and the individual components) was considered an outlier. The current study suggests that a significant difference in outliers for tibial slope does not influence a difference in revision surgery at mid-term follow-up. In 2013, Kim et al. found that sagittal alignment of the tibial component between 0° and 7° leads to better survival of the prosthesis [26]. The article described a mean time to failure of 9.8 years (range 8–12.6). This suggests that continued follow-up of our patient cohort is warranted to assess differences in the survival rate of the prosthesis at long-term. For better prediction of the survival of the femoral and tibial components, radio stereometric analysis (RSA) can be used to early detect migration of the components. This could lead to a more accurate comparison of two surgical techniques with both favorable outcomes regarding survival of the prosthesis. RSA can be considered in future studies comparing two surgical techniques.
The strength of this study lies in the prospective randomized design with a response rate of 70% at mid-term follow-up. Furthermore, a GLMM was used to analyze the data and is considered to be the appropriate method for assessing outcome over time [27].
Since to our knowledge, this study is the first randomized trial to access the differences between MRI- and CT-based PSI from the same manufacture with mid-term follow-up, our results suggest that both methods are reliable and can be used in TKA surgery.
A limitation of this study could be found in the fact that the power and sample size calculation was done for the clinical outcome at 2 years follow-up. Probably, this present study was underpowered to detect a significant difference regarding survival of the prosthesis. Another noteworthy limitation is the fact that due to the pandemic, patients did not visit the outpatient clinic. Therefore, no radiological X-rays were taken and physical examination was not performed. It also led to an increased number of patients (n = 21) that refused further participation and this may have increased the loss to follow-up. This information should be taken into account at the 10-year follow-up.
Conclusion
At mid-term follow-up, survival rates between CT- and MRI-based patient-specific instrumentation did not show a significant difference. Regarding clinical outcome, only the EQ-5D-VAS (p < 0.040) showed a statistically significant difference over time, in favor of the MRI-group. This suggests that both scan modalities are suitable for use in daily practice resulting in satisfied outcome.
References
Price AJ, Alvand A, Troelsen A, Katz JN, Hooper G, Gray A et al (2018) Knee replacement. Lancet 392(10158):1672–1682. https://doi.org/10.1016/S0140-6736(18)32344-4
Mattei L, Pellegrino P, Calò M, Bistolfi A, Castoldi F (2016) Patient specific instrumentation in total knee arthroplasty: a state of the art. Ann Transl Med 4(7):126. https://doi.org/10.21037/atm.2016.03.33
Nguyen LL, Lehil MS, Bozic KJ (2015) Trends in total knee arthroplasty implant utilization. J Arthroplast 30(5):739–742. https://doi.org/10.1016/j.arth.2014.12.009
Ensini A, Timoncini A, Cenni F, Belvedere C, Fusai F, Leardini A et al (2014) Intra- and post-operative accuracy assessments of two different patient-specific instrumentation systems for total knee replacement. Knee Surg Sports Traumatol Arthrosc 22(3):621–629. https://doi.org/10.1007/s00167-013-2667-9
Thijs E, Theeuwen D, Boonen B, van Haaren E, Hendrickx R, Vos R et al (2020) Comparable clinical outcome and implant longevity after CT- or MRI-based patient-specific instruments for total knee arthroplasty: a 2-year follow-up of a RCT. Knee Surg Sports Traumatol Arthrosc 28(6):1821–1826. https://doi.org/10.1007/s00167-019-05616-x
Pfitzner T, Abdel MP, von Roth P, Perka C, Hommel H (2014) Small improvements in mechanical axis alignment achieved with MRI versus CT-based patient-specific instruments in TKA: a randomized clinical trial. Clin Orthop Relat Res 472(10):2913–2922. https://doi.org/10.1007/s11999-014-3784-6
Asada S, Mori S, Matsushita T, Nakagawa K, Tsukamoto I, Akagi M (2014) Comparison of MRI- and CT-based patient-specific guides for total knee arthroplasty. Knee 21(6):1238–1243. https://doi.org/10.1016/j.knee.2014.08.015
Silva A, Pinto E, Sampaio R (2016) Rotational alignment in patient-specific instrumentation in TKA: MRI or CT? Knee Surg Sports Traumatol Arthrosc 24(11):3648–3652. https://doi.org/10.1007/s00167-014-3394-6
Schotanus MGM, Sollie R, van Haaren EH, Hendrickx RPM, Jansen EJP, Kort NP (2016) A radiological analysis of the difference between MRI- and CT-based patient-specific matched guides for total knee arthroplasty from the same manufacturer: a randomized controlled trial. Bone Jt J 98-B(6):786–92. https://doi.org/10.1302/0301-620X.98B6.36633
Wu XD, Xiang BY, Schotanus MGM, Liu ZH, Chen Y, Huang W (2017) CT- versus MRI-based patient-specific instrumentation for total knee arthroplasty: a systematic review and meta-analysis. Surgeon 15(6):336–348. https://doi.org/10.1016/j.surge.2017.06.002
Haverkamp D, Breugem SJM, Sierevelt IN, Blankevoort L, van Dijk CN (2005) Translation and validation of the dutch version of the oxford 12-item knee questionnaire for knee arthroplasty. Acta Orthop 76(3):347–352. https://doi.org/10.1080/00016470510030814
Roorda LD, Jones CA, Waltz M, Lankhorst GJ, Bouter LM, van der Eijken JW et al (2004) Satisfactory cross cultural equivalence of the Dutch WOMAC in patients with hip osteoarthritis waiting for arthroplasty. Ann Rheum Dis 63(1):36–42. https://doi.org/10.1136/ard.2002.001784
Freyd M (1923) The graphic rating scale. J Educ Psychol 14(2):83–102. https://doi.org/10.1037/h0074329
Shadid MB, Vinken NS, Marting LN, Wolterbeek N (2016) The dutch version of the forgotten joint score: test-retesting reliability and validation. Acta Orthop Belg 82(1):112–18
Lamers LM, McDonnell J, Stalmeier PFM, Krabbe PFM, Busschbach JJV (2006) The Dutch tariff: results and arguments for an effective design for national EQ-5D valuation studies. Health Econ 15(10):1121–1132. https://doi.org/10.1002/hec.1124
Schotanus MGM, Thijs E, Heijmans M, Vos R, Kort NP (2018) Favourable alignment outcomes with MRI-based patient-specific instruments in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 26(9):2659–2668. https://doi.org/10.1007/s00167-017-4637-0
Kang Dong-Geun, Bae Jung-Kwon, Kim Kang-II (2021) MRI-based or CT-based patient-specific instrumentation in total knee arthroplasty: how do the two systems compare? Arthroplasty. https://doi.org/10.1186/s42836-019-0020-6
Clement ND, Scott CEH, Hamilton DF, MacDonald D, Howie CR (2021) Meaningful values in the forgotten joint score after total knee arthroplasty. Bone Jt J 103-B(5):846–54. https://doi.org/10.1302/0301-620X.103B5.BJJ-2020-0396.R1
Carlson VR, Post ZD, Orozco FR, Davis DM, Lutz RW, Ong AC (2018) When does the knee feel normal again: a cross-sectional study assessing the forgotten joint score in patients after total knee arthroplasty. J Arthroplast 33(3):700–703. https://doi.org/10.1016/j.arth.2017.09.063
Wang Y, Yin M, Zhu S, Chen Xi, Zhou H, Qian W (2021) Patient-reported outcome measures used in patients undergoing total knee arthroplasty. Bone Jt Res 10(3):203–217
Eckhard L, Munir S, Wood D, Talbot S, Brighton R, Walter B et al (2021) The ceiling effects of patient reported outcome measures for total knee arthroplasty. Orthop Traumatol Surg Res 107(3):102758. https://doi.org/10.1016/j.otsr.2020.102758
Alviar MJ, Olver J, Brand C, Hale T, Khan F (2011) Do patient-reported outcome measures used in assessing outcomes in rehabilitation after hip and knee arthroplasty capture issues relevant to patients? results of a systematic review and ICF linking process. J Rehabil Med 43(5):374–381. https://doi.org/10.2340/16501977-0801
Rolfson O, Malchau H (2015) The use of patient-reported outcomes after routine arthroplasty: beyond the whys and ifs. Bone Jt J 97-B(5):578–81. https://doi.org/10.1302/0301-620X.97B5.35356
Ramkumar PN, Harris JD, Noble PC (2015) Patient-reported outcome measures after total knee arthroplasty: a systematic review. Bone Jt Res 4(7):120–127. https://doi.org/10.1302/2046-3758.47.2000380
Small SR, Bullock GS, Khalid S et al (2019) Current clinical utilization of wearable motion sensors for the assessment of outcome following knee arthroplasty: a scoping review. BMJ Open 9(12):e033832. https://doi.org/10.1136/bmjopen-2019-033832
Kim YH, Park JW, Kim JS, Park SD (2014) The relationship between the survival of total knee arthroplasty and postoperative coronal, sagittal and rotational alignment of knee prosthesis. Int Orthop 38(2):379–385. https://doi.org/10.1007/s00264-013-2097-9
DeSouza CM, Legadza ATR, Sankoh AJ (2009) An overview of practical approaches for handling missing data in clinical trials. J Biopharm Stat 19(6):1055–1073. https://doi.org/10.1080/10543400903242795
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. DT and IH collected the data and performed the statistical analysis. DT wrote and coordinated the manuscript. BB, RH and EH performed the surgery’s and gave feedback on the manuscript. MS participated in the design of the study and gave feedback on the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors did not receive support from any organization for the submitted work. The authors have no relevant financial of non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Theeuwen, D.M.J., Haveman, I., Boonen, B. et al. No differences in mid-term survival and clinical outcome between CT- and MRI-based patient-specific instrumentation for total knee arthroplasty, a randomized controlled trial. Eur J Orthop Surg Traumatol (2023). https://doi.org/10.1007/s00590-023-03680-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00590-023-03680-1