Abstract
Purpose
To compare clinical and radiological outcomes, implant survivorship at a minimum of 1-year follow-up using metaphyseal trabecular cones with or without impaction grafting in a complex revision TKA.
Methods
A retrospective comparative matched analysis was performed and 15 patients who underwent revision surgery using the combination of porous trabecular metaphyseal cone and diaphyseal impaction grafting (MC–IBG) were matched with a group of 13 patients who also underwent revision surgery using metaphyseal cone (MC) without impaction grafting. All included patients presented severe bone defect (AORI 2,3) and a rotating-hinge prosthesis were implanted.
Results
Both groups were comparable regarding the baseline demographic and clinical data. Patients had previously undergone a mean of 4 (range, 2–12) and 3 (range, 2–5) previous procedures in the MC-IBG and MC groups, respectively. The indications for revision were aseptic loosening in 11 (73.3%) and 11 (84.6%) patients; prosthetic joint infection in 4 (26.7%) and 2 (15.4%) in the MC–IBG and MC groups, respectively. There was no significant difference in the mean postoperative Knee Society Score between the study groups (p = 0.806). Overall, 4 patients had further revision. Two patients were revised in the MC–IBG group, one patient for aseptic loosening and the second one after 2 episodes of instability. Two patients in the MC group presented prosthetic joint infection and underwent a two-stage reimplantation. No significant difference was observed between the study groups at comparison (p = 0.92).
Conclusion
Trabecular metal cones with diaphyseal impaction grafting provide an alternative technique in a complex revision TKA surgery with early clinical and radiographic success.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Over the last decade, there was a dramatic increase in expected revision total knee arthroplasty (rTKA) procedures because of the rapidly aging population [1]. Revision total knee arthroplasty with severe bone loss represents a challenging situation for many knee replacement surgeons. Several surgical options exist for those complex cases classified as Anderson Orthopaedic Research Institute (AORSI) [2] type 2 and 3, such as structural allografts [3,4,5], modular metal augmentations [6], distal femoral replacement megaprostheses [7], and highly porous metaphyseal cones.
The high complication and moderate survival rates were reported using structural allografts [8, 9] while highly porous titanium and tantalum metaphyseal cones have been shown significantly improved short- and long-term survival rates in the treatment of extensive bone loss [10, 11] compared with the structural allograft [12]. The improved survivorship of highly porous metaphyseal cones is attributed to their biocompatibility and high osseointegration capacity. However, rTKA is frequently associated with significant diaphyseal bone loss, especially after removal of the failed implants which can severely compromise the fixation and survivorship of future construct.
Impaction bone grafting (IBG) can optimally address substantial bone loss in a previously violated and sclerotic hots bone [13,14,15,16]. The technique is a modification that was originally described for the treatment of bone defects in total hip arthroplasty [17, 18]. However, the outcomes of isolated IBG in a complex rTKA have not been as successful as in complex revision hip surgeries [13, 15, 16, 19].
To the best of our knowledge, there is no comparative data in the literature between using highly porous metaphyseal cones with and without diaphyseal IBG in AORI 2 and 3 bone defects and this led us to conduct this comparative case–control study. The main purpose of the study was to report clinical, radiological outcomes, and implant survivorship in 2 matched therapeutic groups. We hypothesized that the use of MC associated with diaphyseal IBG can provide a stable and comparable fixation with the use of MC in isolation.
Material and methods
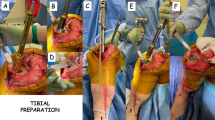
Between 2018 and 2021, we performed 31 complex rTKA using a hinged knee prosthesis (LINK Endo-model) in combination with metaphyseal cones (LINK, Hamburg, Germany). Three patients were lost to follow-up. All patients presented uncontained metaphyseal defect and in 15 patients extensive cancellous bone loss was observed intraoperatively with sclerotic diaphysis (Fig. 1). Diaphyseal impaction bone grafting was used in these patients in addition to metaphyseal cones and hinged knee prostheses. In all cases and just before the surgery a thorough radiographic analysis was performed to assess the severity of bone defect and for an image-based preoperative planning. In addition, bone defects were classified intraoperatively prior to impaction grafting and cone placement.
Patients were followed at 6 weeks, 6 months, 1 year, and then on a yearly basis. Serial standing AP and lateral plain radiographs of the knee were obtained preoperatively and postoperatively, at 6 weeks, 6 months, and at the latest follow-up. Radiolucent lines at the latest follow-up were documented according to the Knee Society total knee arthroplasty roentgenographic evaluation system [21]. The absence of radiolucent lines around the metaphyseal cone and prosthesis was interpreted as possible bone ingrowth. Bone graft incorporation was assessed according to the criteria established by de Waal Malefijt et al. [22]. Radiographs were assessed separately by two reviewers: an independent senior radiologist and by a treating senior surgeon. Postoperative functional evaluations were performed at the time of the latest follow-up using the Knee Society Score (KSS). The failure was defined if the prosthesis was removed or revised for any reason.
Surgical technique
The surgical technique was conducted as it was previously described [23] and was performed through a midline parapatellar approach. Briefly, failed implants are removed, fibrotic tissue around the bone and the sclerotic canals are carefully curetted, irrigated, and the severity of the bone defect is graded according to the AORI classification system [2]. Intramedullary canals are reamed, and joint surfaces are prepared for a relevant size new prosthesis. Morselized fresh frozen cancellous chips are carefully impacted into the canal and around the trial stem, after graft impaction the stem is carefully removed. Care must be taken to remove only the necessary metaphyseal bone. Once the size of the cone has been decided and preparation is complete, the final cone is impacted. Metaphyseal cone sizes are decided, and implants are cemented in a hybrid fashion. In all cases, we used a rotating hinged prosthesis and antibiotic-loaded cement is used in all procedures (Simplex P Tobramycin-Howmedica Stryker Osteonics, Mahwah, NJ, and Palacos R + G, Zimmer Orthopaedics, Warsaw, IN). Intraoperative tissue cultures are routinely taken in all patients and intravenous prophylaxis is given until negative tissue cultures are confirmed. Postoperative rehabilitation protocol included active ROM exercises and all patients were allowed full weight bearing as tolerated.
Statistical analysis
Qualitative variables were described by absolute and relative frequencies, and quantitative variables by mean and standard deviation. The chi-squared test was applied to compare qualitative variables, while the comparison of quantitative variables exhibiting a normal distribution versus dichotomous qualitative variables was carried out using the Student’s t-test. Before-after analyses were carried out using the student’s t-test for paired samples when analyzing quantitative variables, and Mc Nemar test for qualitative variables. The Kaplan–Meier survival analysis was performed to estimate implant survivorship with a 95% confidence interval (CI) using implant removal or revision as the endpoint. Statistical significance was considered when p < 0.05. All statistical analysis was performed using R-3.6.0 (R Core Team 2020, Vienna, Austria).
Results
The mean time of follow-up was 12.3 (SD, ± 6.31) and 12.4 (SD, ± 6.91) months in the MC–IBG and MC groups, respectively. The mean age of the patients was 73.9 ± 7.41 years in the MC–IBG and 74.2 ± 9.5 in the MC group. There were 10 females (66.7%) and 5 males (33.3%) in the MC–IBG group and 7 (53.8%) and 6 (46.2%) in the MC group. Overall, 24 metaphyseal cone-IBG were used (11 femoral and 13 tibial sides) in the MC–IBG group and 17 in the MC group (4 femoral and 13 tibial), and the difference was not significant between the 2 groups at comparison (p = 0.079). Table 1 summarizes the patient´s baseline demographic and clinical data with the indications for revision surgery.
Eleven knees (73.3%) in the MC–IBG group and 11 (84.6%) in the MC group were revised for aseptic loosening of the components as periprosthetic joint infection was ruled out in intraoperative cultures. In 4 (26.7%) and 2 (15.4%) patients in the MC–IBG and MC groups a two-staged revision was conducted due to periprosthetic infection.
In the MC–IBG group, the femoral and tibial canal at the site of impaction grafting presented a cavitary metaphyseal defect with sclerotic diaphyseal cortices in all revised cases (Fig. 1). According to the AORI classification, 11(73.3%) patients presented uncontained defect on the femoral side (F3), and 13 knees (86.6%) showed uncontained tibial defect (T3). Remaining patients revealed Type 2 AORI defects on both tibial and femoral side. On the other hand, in the MC group, tibial side T2B defect was observed in 9 (69.2%) patients and F2B defect was found in 4 (30.7%) cases.
Postoperatively, the mean KSS increased significantly in both groups and when the between-group compare was conducted no significant difference was found (Fig. 2).
Overall, 3 cases (20%) of nonprogressive radiolucency at the bone-cement interface were observed in at least one zone in the MC–IBG group. A total of 4 patients (36.3%) patients presented radiological signs of loosening in the MC group. These patients were satisfied with their results, and no impairment in their activities of daily living was reported. The difference between the study groups was not significant (p = 0.67).
Overall, four patients had further revision or removal of the construct. Two patients were revised in the MC–IBG group, one patient for aseptic loosening of the tibial component and the second one after 2 episodes of knee instability (Fig. 3). Both cases were managed with one-staged conversion to arthrodesis (WALDEMAR LINK® GmbH & Co.KG). Those patients were the most complex cases with severe bone loss and who had undergone 7 and 4 previous knee arthroplasty procedures, respectively. At the time of component removal, the trabecular metal tibial cone was fully incorporated with bone ingrowth into the pores of the cone. Two patients in the MC group presented prosthetic joint infection (PJI) and underwent a two-stage reimplantation. Thus, survival free from the revision of the construct for any reason was 86.6% and 84.6% in the TM-IG and TM groups and no significant difference was observed at comparison (Fig. 4).
A 75-year-old female patient with 7 prior surgeries and severe bone loss underwent revision surgery using metaphyseal cones and impaction grating. She was doing well until presenting 2 consecutive episodes of instability and was managed with conversion to arthrodesis (WALDEMAR LINK® GmbH & Co.KG). a Lateral X-ray control after 1-year of follow-up with no radiological signs of loosening. b Lateral X-ray showing dislocated rotating hinged knee prostheses. c Conversion to knee arthrodesis, still no signs of radiological loosening around the retained diaphyseal stems and bone graft
There were also 2 additional patients in the MC–IBG who underwent irrigation, debridement, and component retention in the early postoperative period for persistent postoperative drainage. However, no PJI was confirmed in routine intraoperative cultures.
We found no evidence of graft resorption in the remaining patients in the MC–IBG group. In 2 patients where impaction grafting was used in isolation no complications related to the graft were observed. The remaining metaphyseal cones were stable, and the diaphyseal impacted bone with no visible radiolucent lines around the components and no signs of graft resorption (Fig. 5).
Lateral radiographs of a 74-year-old male patient who underwent revision surgery for aseptic loosening using a metaphyseal cone with impaction grafting in the tibia and impaction grafting in the femur. a Postoperatively at 6 weeks of follow-up; b at 1-year of follow-up all grafts seemed to be incorporated
Discussion
So far, this is the first comparative study reported that evaluates clinical and radiological outcomes of using the combination of metaphyseal cones and diaphyseal IBG in a complex rTKA. The main finding of this study was that the use of metaphyseal cones combined with diaphyseal impaction grafting offers comparable clinical outcomes and survival rate with the use of metaphyseal cones in isolation at short follow-up in patients with substantial bone loss.
Reliable fixation methods are one of the main challenges in the replacement surgery era in which patients commonly present severe bone defect after multiple prior procedures. The results of the use of impaction grafting in a complex rTKA have not been as successful as in hip replacement surgeries, and relatively few clinical studies have reported on the outcomes of impaction bone grafting in revision TKA [13, 19, 20]
The main goal when using impaction grafting is to restore bone stock and provide lasting support for the construct. Lonner et al. [19] reviewed the results of 17 revision TKA in 14 patients after 3 years of follow-up in whom large uncontained defects were managed with impaction allografting and molded wire mesh. They described 1 case of acute infection developed within 6 weeks after surgery with no postoperative evidence of clinical recurrence. No patients required revision surgery, although, nonprogressive tibial radiolucency has been observed in 3 patients. This is in accordance with our findings as we observed 3 knees with radiolucency at the bone-cement interface in the MC–IBG group. However, no further revision was needed in these patients, and no functional impairment was reported.
Similarly, Lotke et al. [13] reported good mid-term results of 48 consecutive rTKA presenting both, contained and uncontained defects and treated with metaphyseal impaction grafting with an average follow-up of 3.8 years. The same technique was used as described by Lonner et al. [19] The authors found no mechanical failures and all radiographs have shown incorporation and remodeling of the bone graft. Steens et al. [16] reported implant survival of 76% at 5 years in 30 patients who underwent revision arthroplasty of the knee using hinge knee prostheses and impaction bone grafting without metaphyseal cones. No knees were revised beyond 5 years and no mechanical failures of the revisions were reported. All their cases showed incorporation and remodeling of the bone graft. This is in accordance with our findings as we observed a high rate of graft remodeling and incorporation.
Conversely, a recent study from the same institution in the same cohort [15] found a high revision rate in 29 patients with 12 (41%) of them requiring revision surgery due to mechanical failure after ten years of follow-up. The authors concluded that IBG alone is not a methodologically sound technique in the revision of rotational and hinged knee arthroplasties. One of the main explanations for this high failure rate at a longer follow-up may be the lack of a stable metaphyseal anchorage that is necessary to ensure proper and durable fixation and cement interdigitation.
The importance of metaphyseal fixation during rTKA, especially when dealing with substantial bone loss (AORI type 2 and 3 defects) is paramount. The high variability in clinical and radiological outcomes of structural allografts with high failure rate [9, 10] and their limited capacity for incorporation, led to the development of highly porous metaphyseal cones for the reconstruction of massive uncontained bone defects. Porous metaphyseal cones have shown durable long-term fixation in cases with the loss of the metaphyseal cancellous bone [11]. On the other hand, diaphyseal impaction grafting offers the possibility of restoring cancellous bone to the sclerotic femoral and tibial canals for improved cement interdigitation. It´s the combination of a stable metaphyseal anchorage and biological diaphyseal fixation that restores bone stock and pushes the worst AORI score cases to the less damaged scenario.
Denehy et al. [10] reported excellent short-term results with 90.2% all-cause survival and no cases of aseptic loosening with a mean follow-up of 27 months in 62 rTKAs using highly porous titanium metaphyseal cones. Potter et al. [24] documented outcomes of 159 tantalum metaphyseal femoral cones implanted in 157 patients with 5 years of follow-up. The authors found that aseptic failure of the femoral cone was associated with the use of a hinged TKA in a patient with Type 3 bone defects. In our series of metaphyseal cones and impaction grafting, 8 (53.3%) patients presented AORI F3 and T3 defect where a hinged prosthesis was implanted. We found one case of aseptic loosening during the follow-up in these patients. It is noteworthy that in patients with severe bone loss (AORI type 3 defect) and sclerotic diaphyseal cortices in addition to a stable metaphyseal anchorage provided by metaphyseal cones, diaphyseal impaction grafting ensures proper fixation for cement interdigitation.
To the best of our knowledge, only one study conducted by Bedard et al. [23] reported outcomes of using metaphyseal cones with diaphyseal IBG in 35 rTKA. They noted a satisfactory high rate of implant fixation with survival free of revision at 5 years. In our comparative analysis, we found a survival rate of 86.6% which is comparable to that reported by Bedard et al. [23]. In our cohort, all but one cone with impaction grafting (regarded as a failure for aseptic loosening and the patient underwent knee arthrodesis) showed signs of radiographic osseointegration at the latest follow-up. We did not document any stress shielding or early signs of radiographic loosening in the remaining knees.
This study has several limitations. First and foremost, a relatively short follow-up enables us to assess the long-term complications of these constructs. However, our results are promising and suggest that this technique may be useful for managing severe metaphyseal and diaphyseal bone loss in a complex rTKA. Second, inherent limitations due to its retrospective nature and small sample size. Nevertheless, this is the first reported matched comparative study including complex cases with severe bone defects that hopefully, are not frequently seen in clinical practice, and are only managed in highly specialized centers. Moreover, demographic data were retrieved from medical records, imaging data were collected on successive knee X-rays, and patient-reported outcomes were prospectively collected, not subjected to recall bias. Third, the combination of metaphyseal cones and diaphyseal impaction grafting was used in all patients who presented at least AORI type 2 and 3 bone loss either the tibial or femoral side. However, in 2 patients with type 1 tibial and femoral defect impaction grafting was used without metaphyseal cone implantation as the diaphyseal bone was sclerotic, and therefore, it was difficult to achieve sufficient stability for the cement interdigitation. It is noteworthy that these patients might have been treated in other ways in different facilities. Lastly, only one type of metaphyseal cone was used, and the outcomes may not be the same using a different design or material cone.
To sum up, the combination of trabecular metal cones and impaction grafting is a promising tool in the armamentarium of the reconstructive surgeon that ensures a stable construct by achieving biologic fixation in the context of large bone defects. The findings of this study can shape a future research to deal with these limitations and to focus on evaluating whether this type of fixation can allow us to use a short diaphyseal stems in the future. While longer-term follow-up is necessary, we found the early results encouraging, and further studies are warranted to clarify the specific indications to improve long standing clinical and radiological outcomes.
Conclusion
Trabecular metal cones with diaphyseal impaction grafting provide an alternative technique in a complex revision TKA surgery with early clinical and radiographic success.
References
Haidukewych GJ, Hanssen A, Jones RD (2011) Metaphyseal fixation in revision total knee arthroplasty: indications and techniques. J Am Acad Orthop Surg 19(6):311–318. https://doi.org/10.5435/00124635-201106000-00001
Engh GA, Ammeen DJ (1999) Bone loss with revision total knee arthroplasty: defect classification and alternatives for reconstruction. Instr Course Lect 48:167–175
Engh GA, Ammeen DJ (2007) Use of structural allograft in revision total knee arthroplasty in knees with severe tibial bone loss. J Bone Jt Surg Am 89(12):2640–2647. https://doi.org/10.2106/JBJS.F.00865
Ghazavi MT, Stockley I, Yee G, Davis A, Gross AE (1997) Reconstruction of massive bone defects with allograft in revision total knee arthroplasty. J Bone Jt Surg Am 79(1):17–25
Harris AI, Poddar S, Gitelis S, Sheinkop MB, Rosenberg AG (1995) Arthroplasty with a composite of an allograft and a prosthesis for knees with severe deficiency of bone. J Bone Jt Surg Am 77(3):373–386. https://doi.org/10.2106/00004623-199503000-00007
Haas SB, Insall JN, Montgomery W 3rd, Windsor RE (1995) Revision total knee arthroplasty with use of modular components with stems inserted without cement. J Bone Jt Surg Am 77(11):1700–1707. https://doi.org/10.2106/00004623-199511000-00009
Berend KR, Lombardi AV Jr (2009) Distal femoral replacement in nontumor cases with severe bone loss and instability. Clin Orthop Relat Res 467(2):485–492. https://doi.org/10.1007/s11999-008-0329-x
Bauman RD, Lewallen DG, Hanssen AD (2009) Limitations of structural allograft in revision total knee arthroplasty. Clin Orthop Relat Res 467(3):818–824. https://doi.org/10.1007/s11999-008-0679-4
Clatworthy MG, Ballance J, Brick GW, Chandler HP, Gross AE (2001) The use of structural allograft for uncontained defects in revision total knee arthroplasty. A minimum five-year review. J Bone Jt Surg Am 83(3):404–411. https://doi.org/10.2106/00004623-200103000-00013
Denehy KM, Abhari S, Krebs VE, Higuera-Rueda CA, Samuel LT, Sultan AA, Mont MA, Malkani AL (2019) Metaphyseal fixation using highly porous cones in revision total knee arthroplasty: minimum two year follow up study. J Arthroplast 34(10):2439–2443. https://doi.org/10.1016/j.arth.2019.03.045
Bonanzinga T, Gehrke T, Zahar A, Zaffagnini S, Marcacci M, Haasper C (2017) Are trabecular metal cones a valid option to treat metaphyseal bone defects in complex primary and revision knee arthroplasty? Joints 6(1):58–64. https://doi.org/10.1055/s-0037-1608950
Beckmann NA, Mueller S, Gondan M, Jaeger S, Reiner T, Bitsch RG (2015) Treatment of severe bone defects during revision total knee arthroplasty with structural allografts and porous metal cones-a systematic review. J Arthroplast 30(2):249–253. https://doi.org/10.1016/j.arth.2014.09.016
Lotke PA, Carolan GF, Puri N (2006) Impaction grafting for bone defects in revision total knee arthroplasty. Clin Orthop Relat Res 446:99–103. https://doi.org/10.1097/01.blo.0000214414.06464.00
Toms AD, Barker RL, Jones RS, Kuiper JH (2004) Impaction bone-grafting in revision joint replacement surgery. J Bone Jt Surg Am 86(9):2050–2060. https://doi.org/10.2106/00004623-200409000-00028
Hilgen V, Citak M, Vettorazzi E, Haasper C, Day K, Amling M, Gehrke T, Gebauer M (2013) 10-year results following impaction bone grafting of major bone defects in 29 rotational and hinged knee revision arthroplasties: a follow-up of a previous report. Acta Orthop 84(4):387–391. https://doi.org/10.3109/17453674.2013.814012
Steens W, Loehr JF, Wodtke J, Katzer A (2008) Morselized bone grafting in revision arthroplasty of the knee: a retrospective analysis of 34 reconstructions after 2–9 years. Acta Orthop 79(5):683–688. https://doi.org/10.1080/17453670810016713
Slooff TJ, Schimmel JW, Buma P (1993) Cemented fixation with bone grafts. Orthop Clin N Am 24(4):667–677
Gie GA, Linder L, Ling RS, Simon JP, Slooff TJ, Timperley AJ (1993) Impacted cancellous allografts and cement for revision total hip arthroplasty. J Bone Jt Surg Br 75(1):14–21. https://doi.org/10.1302/0301-620X.75B1.8421012
Lonner JH, Lotke PA, Kim J, Nelson C (2002) Impaction grafting and wire mesh for uncontained defects in revision knee arthroplasty. Clin Orthop Relat Res 404:145–151. https://doi.org/10.1097/00003086-200211000-00026
Boettner F, Bechler U, Springer B, Faschingbauer M, Jungwirth-Weinberger A (2020) Impaction bone grafting in revision total knee arthroplasty-using mesh and cone to contain the defect: a report of 3 cases. Arthroplast Today 6(3):578–584. https://doi.org/10.1016/j.artd.2020.07.001
Ewald FC (1989) The knee society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res 248:9–12
de Waal Malefijt MC, van Kampen A, Slooff TJ (1995) Bone grafting in cemented knee replacement. 45 primary and secondary cases followed for 2–5 years. Acta Orthop Scand 66(4):325–328. https://doi.org/10.3109/17453679508995554
Bedard NA, Cates RA, Lewallen DG, Sierra RJ, Hanssen AD, Berry DJ, Abdel MP (2020) Outcomes of a technique combining diaphyseal impaction grafting and metaphyseal cones for severe bone loss in revision total knee arthroplasty. Bone Jt J 102-B(6_Supple_A):116–122. https://doi.org/10.1302/0301-620X.102B6.BJJ-2019-1511.R1
Potter GD 3rd, Abdel MP, Lewallen DG, Hanssen AD (2016) Midterm results of porous tantalum femoral cones in revision total knee arthroplasty. J Bone Jt Surg Am. 98(15):1286–1291. https://doi.org/10.2106/JBJS.15.00874
Acknowledgements
We thank Dr Ignacio Mahillo Fernández, BS, for his contributions to the statistical analysis.
Funding
This is a retrospective research and was not supported by funds.
Author information
Authors and Affiliations
Contributions
Conceptualization: LD; material and preparation: LD, DS, EC. Data collection and analysis: LD, DS. The first draft of the manuscript was written by LD. All authors commented on the previous version of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
LD and DS declare that they have no conflict of interest. EC has received speaker and consultant honoraria from DePuy Synthes, Smith & Nephew, and Stryker.
Ethical approval
Ethical approval was waived by the local Ethics Committee.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
The authors affirm that human research participants provided informed consent for publication of the images in Figs. 1a, b and 3a, b, c.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dzidzishvili, L., Sáez, D. & Calvo, E. Metaphyseal cones combined with diaphyseal impaction grafting provide good outcomes and survival in a complex revision total knee arthroplasty: a matched comparative analysis. Eur J Orthop Surg Traumatol 34, 577–583 (2024). https://doi.org/10.1007/s00590-023-03659-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-023-03659-y