Abstract
Introduction
Loosening and migration are common modes of aseptic failure following complex revision total knee arthroplasty (rTKA). Metaphyseal cones allow surgeons to negotiate the loss of femoral and tibial bone stock while obtaining stable bony fixation. This study examines the mid-term functional and radiographic outcomes in patients undergoing rTKA utilizing a novel metaphyseal cone system with stems of variable length and fixation methods.
Methods
This two-center retrospective study examined all patients who underwent rTKA with a novel porous, titanium tibial or femoral cone in combination with a stem of variable length and fixation who had a minimum follow-up of 2-years. Outcome analysis was separated into tibial and femoral cones as well as the stem fixation method (hybrid vs. fully cemented).
Results
Overall, 123 patients who received 156 cone implants were included (74 [60.2%] tibial only, 16 [13.0%] femoral only, and 33 [26.8%] simultaneous tibial and femoral) with a mean follow-up of 2.76 ± 0.66 years. At 2-years of follow-up the total cohort demonstrated 94.3% freedom from all-cause re-revisions, 97.6% freedom from aseptic re-revisions, and 99.4% of radiographic cone osteointegration. All-cause revision rates did not differ between stem fixation techniques in both the tibial and femoral cone groups.
Conclusion
The use of a novel porous titanium femoral and tibial metaphyseal cones combined with stems in patients with moderate to severe bone defects undergoing complex revision total knee arthroplasty confers excellent results independent of stem fixation technique.
Level of evidence
IV, case series.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The volume of revision total knee arthroplasty (rTKA) cases will continue to rise as primary TKA increases and risk factors for revision, such as obesity and old age, become increasingly more common in those with previous primary TKAs [1]. The most frequently reported causes of TKA failure include aseptic loosening, infection, instability, and polyethylene wear [2,3,4]. Mechanical aseptic loosening often results in subsidence, described as the downward migration or “sinking” of all or part of the tibial prosthesis, often requiring revision due to altered knee mechanics [1, 2]. Bone loss is present to some degree in all revision TKA secondary to implant removal and resultant bone resection. This challenge can be addressed using different techniques and implants; however, the optimal approach has not yet been identified because of insufficient long-term data [5].
Three anatomical zones around the femur and tibia are available to support revision implants (joint surface or epiphysis, metaphysis, and diaphysis). Solid fixation in two of the three zones is critical to achieving long-term durability of revision TKA constructs [2]. Given this, numerous augmentation strategies have been developed to offset the bone loss and to restore the structural support and kinematic functionality of the knee. These constructs include traditional allografts and modular components, such as metaphyseal cones and sleeves, which were developed to fill larger femoral and tibial bone defects [3,4,5]. To achieve metaphyseal fixation, cones are a viable alternative to structural allografts, as these augments can provide excellent osteointegration and freedom from aseptic loosening [6,7,8].
Stems, on the other hand, can achieve diaphyseal fixation while bypassing bony defects and unloading compromised epiphyseal and metaphyseal zones [9]. Different stems lengths and fixation methods can be utilized in rTKA. Historically, long press-fit stems have been preferred to optimize the implant alignment and offload the metaphysis. However, pain that rises by stress between the tip of the stem and the host bone has been reported [10]. Recent studies reported that the use of metaphyseal cones with short, cemented stems had a similar survival rate with better functional outcomes compared with the use of cones and long uncemented stems [11, 12]. Therefore, the biomechanical efficacy of the cementation technique, when combined with metaphyseal cones, remains unclear.
Given this, the purpose of the study was to compare the functional outcomes and survival of rTKA using a novel titanium cone design with stems of variable length and fixation at a minimum of a 2-year follow-up.
Methods
This two-center institution, multi-surgeon, retrospective study examined all patients undergoing rTKA who received a porous, titanium tibial or femoral cone at two large institutions. Porous titanium metaphyseal cones were used to augment reconstruction in cases with severe tibial and/or femoral bone defects during rTKA with Anderson Orthopedic Research Institute bone loss classification ≥ 2 [13]. The Legion Cone System (Smith&Nephew, Memphis, TN) was FDA approved on January 2017 and integrated for use in revision TKA in both centers in June 2017. After institutional review board approval, electronic medical records (EMR) from two independent health systems were reviewed to identify all revision total knee arthroplasties performed between July 2017 to April 2019. Data were collected and analyzed starting September 1st 2021. Inclusion criteria for this study were: patients who were 18 years or older who underwent revision TKA using Legion Cone System (Smith&Nephew, Memphis, TN). Exclusion criteria included: primary TKA cases, patients with pathologic lesions in the affected knee, and patients with less than 2-year follow-up since the index rTKA procedure. Of the 207 patients identified, seven primary TKA were excluded, two cases for pathologic lesions in the affected knee and 75 that did not complete a 2-year minimum follow-up. Patients who died with the implant in situ and patients who lost to follow-up were considered censored at the date of death and last follow-up, respectively. Finally, 123 patients met the inclusion criteria to be includes for analysis. All patients that underwent rTKA with a tibial cone were paced in the tibial cone cohort, and all patients that underwent rTKA with a femoral cone were paced in the femoral cone cohort.
Data search
The EMRs were reviewed for demographic data, including patient age, gender, BMI, American Society of Anesthesiologists (ASA) Classification, and smoking status. Surgical characteristics were collected from a review of operative reports, including operative time, bone loss, revision indication, implant constraint, stem length, coupler use, revised components, and femoral and tibial cone use. Tibial and femoral-sided bone loss was categorized per the Anderson Orthopaedic Research Institute bone defect classification on the basis of intraoperative assessment and preoperative X-ray findings [13, 14] (Table 1). Perioperative and clinical outcomes, such as operative time, hospital length of stay (LOS), 90-day readmissions, were also collected for this analysis. Re-revision including incidence, indications and cone explanation data was obtained from surgeries that were performed solely in the participating centers. Functional outcomes measured by knee flexion were collected from preoperative and the most recent postoperative reports. Re-revision surgery was defined as any case in which the femoral, tibial, polyethylene liner or all components were explanted or exchanged. LOS was evaluated in days spent in the hospital following surgery, and surgical time was derived by calculating the time difference between the initial skin incision and skin closure.
Radiographic follow-up and analysis
All patients were followed postoperatively at various time points, including 2 weeks, 6 weeks, 3 months, 6 months, 1 year and 2-year postoperatively. At the 2-year follow-up visit, patients were instructed to come for a follow-up visit should any symptoms occur or per surgeon request on a case to case basis. Thus some patients have longer follow-up visits which are reported in the figures. Pre and post-operative knee range of motion as well as knee stability were evaluated by the operating surgeon. Immediate postoperative anteroposterior and lateral knee radiographs were made and analyzed along with radiographs made at three months, twelve months, and annually thereafter. All radiographs were assessed by 2 orthopedic surgeons who did not perform the surgery. The radiographic assessment was performed based on the Knee Society total knee arthroplasty radiographic evaluation system for long-stemmed revision prostheses of the latest follow-up radiograph [15]. The interface between the cone and the host bone was also assessed for initial and progressive radiolucency as well as areas of initial radiolucency that had not changed or resolved with continued follow-up. As described by Fehring et al., femoral implants were classified as stable (≤ 8 radiolucencies), closely observe (9 to 19), or loose (≥ 20 radiolucencies). Tibial implants were classified as stable (≤ 9 radiolucencies), closely observe (10 to 22), and loose (≥ 23 radiolucencies) [16].
Surgical technique
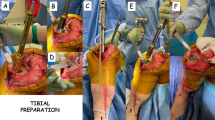
All procedures were performed by fellowship-trained, high-volume arthroplasty surgeons at their respective institutions. All patients underwent rTKA through the medial parapatellar approach. After explantation of the necessary components, the degree of femoral and tibial bone loss was assessed and a determination was made regarding the need for a metaphyseal cone by the operating surgeon. Porous metaphyseal titanium cones were utilized in all patients in this cohort. Decision regarding the type of fixation in the revised femoral and tibial components (hybrid vs fully cemented) and degree of constraint in polyethylene liner or use of hinge was made at the discretion of the operating surgeon based on patient-specific bone quality and morphology. In the hybrid cementation technique, cement was applied to the bone surface, metaphyseal bone, and the implant but avoiding cement on the majority of the stem (press fit stem) (Fig. 1) [17]. In the cemented technique, cement was applied to the bony surface and pressurized in the canal with a cement plug [18].
Statistical analysis
Binary variables were created to identify patients with femoral and tibial cones, and within those groups, patients with hybrid or fully cemented stems. Study participants' demographic and clinical baseline characteristics were described as means with standard deviations (SD) for continuous variables and frequencies with percentages for categorical variables. Survivorship was analyzed and presented graphically by using the Kaplan–Meier (KM) method. Differences in survivorship outcomes between groups were calculated using the log-rank test. Outcomes and survivorship data were calculated using the time of the latest follow-up. Following the patients’ 2-year follow-up visit, they are instructed to come in for a follow-up visit should any symptoms or complications occur or per surgeon’s request on a case to case basis. Hence, the number of patients at risk was low after 3-year follow-up. Given this, KM plots were truncated at the 3-year follow-up point.
A multivariablee binary logistic regression analysis was performed to control for the effect of confounding variables on outcomes. A p-value of less than 0.05 was considered statistically significant. All statistical analysis was performed using IBM SPSS software (IBM-SPSS-version 26, Armonk, NY, USA).
Results
Total cohort
Overall, 123 patients were included in this analysis who received 156 cone implants (74 [60.2%] tibial only, 16 [13.0%] femoral only, and 33 [26.8%] simultaneous tibial and femoral) with a mean follow-up of 2.76 ± 0.66 years. The mean age was 66.1 ± 8.2 years (Table 2).
The most common revision indications included aseptic loosening (58 cases [47.2%]), periprosthetic infection (PJI) (33 cases [26.8%]), and instability (20 cases [16.3%]). (Table 3). Surgical time did not differ between stem fixation methods both in the tibial and femoral groups. Sixteen (13.0%) rTKAs underwent re-revision surgery: 9 for PJI (eight acute and one chronic), three for instability, two for aseptic loosening, one for periprosthetic fracture, and one for liner failure. Notably, ten (62.5%) of the 16 re-revisions were liner exchanges (seven [43.8%] for acute PJI, and three [18.8%] for instability). At the most recent follow-up, knee flexion improved from 101.39 ± 15.58 degrees pre-operatively to 111.19 ± 16.19 degrees post-operatively (p < 0.001). At the most recent radiographic follow-up, one (0.6%) tibial cone with a fully cemented stem had evidence of subsidence. For the entire cohort, freedom from all-cause re-revision was 94.3%, freedom from aseptic re-revision was 97.6%, and freedom from re-revision due to aseptic loosening was 99.4% at 2-year (Fig. 2).
Tibial cones
The indications for revision did not significantly differ between groups (p = 0.599). The proportion of surgeries performed as index revisions (51.8% vs. 29.4, p = 0.019) and with long stems (92.9% vs 43.1%, p < 0.001) was higher in the hybrid cementation group. All-cause re-revision rates (p = 0.428) and indications (p = 0.502) did not differ between cohorts (Table 3).
In multivariate regression, all included baseline or surgical characteristics were not significantly associated with higher all-cause re-revision rates (Table 4). Eleven (10.3%) patients required re-revisions. Of these, four (3.7%) tibial cones were removed. In the hybrid group, three cones were explanted; one due to instability in which the entire construct was changed to a hinged design, one due to aseptic loosening of the tibial baseplate, and one due to PJI. In the cemented group, one cone was explanted due to the aseptic loosening of both the tibial base plate and the cone. Freedom from all-cause re-revision was 96.3% at 2-year (Fig. 3). Patients in the fully cemented group had numerically higher freedom from all-cause re-revision compared to the hybrid group at 2-year (98.0% vs 94.2%, p = 0.312) (Fig. 3). Freedom from tibial cone explanation due to aseptic loosening was 100% at 2-year (Fig. 5).
Femoral cones
The overall distribution of revision indications did not significantly differ between groups (p = 0.129), though the proportion of revisions performed for component malpositioning (12.5% vs. 0.0%, p = 0.024) was higher in the hybrid cementation group. All-cause re-revision rates (p = 0.544) and indications (p = 0.690) did not differ between cohorts. In multivariate regression, all included baseline and surgical characteristics were not associated with higher all-cause re-revision rates (Table 4). Ten (20.4%) patients required re-revisions. Of these, one (2%) cone from the cemented group was removed due to a periprosthetic fracture in which the entire femoral component was replaced. Freedom from all-cause re-revision was 89.8% at 2-year (Fig. 4). No differences in freedom from all-cause re-revision were found between the cemented and hybrid subgroups at 2-year (92.5% vs 85.7%, p = 0.539). Freedom from the explanation of femoral cones due to aseptic loosening was 100% at 2-year (Fig. 5).
Kaplan–Meier survivorship analysis for freedom from all-cause removal of cones. Tibial All-Cause Re-revision. 2-year: 99.1%, 3-year: 98.0%. Femoral All-Cause Re-revision. 2-year: 98.0%, 3-year: 98.0%. Tibial Aseptic Loosening Re-revision. 2-year: 100.0%, 3-year: 97.6%. Femoral Aseptic Loosening Re-revision. 2-year: 100.0%, 3-year: 100.0%
Discussion
In this study, we evaluated 123 rTKAs using 156 novel porous titanium metaphyseal cones with stems of variable length and fixation methods at a minimum of 2 years of follow-up. Our main findings at 2-years minimum follow-up included: (1) 94.3% freedom from all-cause re-revisions and 97.6% freedom from aseptic re-revisions; (2) excellent cone radiographic osteointegration (99.4%); (3) all-cause cone implant survivorship of 96.8%; and (4) all-cause re-revision rates did not differ between stem cementation techniques.
As the incidence of revision TKA continues to increase, implants and techniques to address commonly encountered challenges during revision surgery have become increasingly important [19]. One of the main challenges of rTKA remains the management of bone loss and long-term fixation, as this is a major risk factor for aseptic loosening after rTKA [20]. Cones and other metaphyseal augment systems were developed as a viable alternative to traditional allograft to address moderate tibial and femoral metaphyseal defects (AORI II and III) and to achieve improved long-term implant fixation [2, 19,20,21,22,23].
Previous studies reported excellent outcomes in rTKA using metaphyseal cones. All-cause re-revision rates varied from 86.0–95.4% [6, 8, 24], and multiple analyses reported 100% freedom from aseptic loosening [6, 11, 24]. Similar to these studies, our investigation demonstrated a high all-cause re-revision-free survivorship and excellent freedom from aseptic loosening. Notably, the majority of re-revisions in our cohort were related to PJI. Given that 30.8% of the patients who underwent index revision surgery had a history of PJI, these findings are not surprising and consistent with previously reported re-revision rates for PJI in complex patients undergoing revision TKA [25, 26]. Previous literature reported cone osteointegration rates of 98–100% at a minimum follow-up of 2 years [27, 28]. Our cohort had a single case of cone aseptic loosening, which coincides with these studies to validate the efficacy of this novel porous cone design.
Femoral cones
Majority of studies evaluating cones in rTKA present data about tibial cones [8, 21, 29, 30]. There is a paucity of data in the literature about the outcomes of femoral cones. In a cohort of 159 rTKA with trabecular metal femoral cones, Potter et al. reported 96% freedom from aseptic loosening and 84% freedom from all-cause cone explanations in 5-year follow-up time. Importantly, they did not specify the use of tibial or femoral cones in their cohort. Another study which included 68 3D-printed titanium femoral cones, demonstrated 95.6% freedom from aseptic loosening at the latest follow-up [8]. Our femoral cohort demonstrated similar rates of freedom from aseptic loosening at the latest follow-up. Finally, Tetraulet et al. reported two (2.9%) intraoperative fractures that have occurred when impacting the cone to the femur metaphysis. Our study reported no events of intraoperative fractures.
Stem fixation
Although stems improve mechanical stability, the optimal indications, proper lengths, diameters, and appropriate fixation methods for these constructs remain controversial [9]. There are two traditional stem fixation methods, including hybrid cementation with a cementless press-fit stem and total cementation [10]. In a meta-analysis comparing cemented and cementless stem fixation in revision TKA, Wang et al. found similar outcomes between groups [18]. Moreover, in a randomized trial, Kosse et al. found no differences in radiographic stability and patient-reported functional outcomes when comparing cemented and press-fit stems in patients with mild to moderate bone loss in rTKA at 6.5 years of follow-up [31]. Hence, the superior fixation method remains uncertain.
Despite the abundant literature comparing short cemented versus long uncemented stems in rTKA, limited literature is available examining stem fixation types with the use of metaphyseal cones [6, 8, 11]. In a retrospective cohort of 202 cones with fully cemented and hybrid fixation, Tetralaut et al. reported 100% survivorship of cones for aseptic loosening, 98% all-cause cone revision survival, and 90% freedom from re-revision at 2.4 years of follow-up [8]. However, no comparison of the stem fixation methods was made. In agreement with Kosse et al., our study found no differences in freedom from all-cause re-revision between the hybrid and fully cemented stem groups. In a computational study investigating whether fully cemented stems are required to augment metaphyseal cones in rTKA, Xie et al. compared different stem lengths and found that the highest micromotion was observed at the tip of a long stem, however, the motion was too small to effect osseointegration. In a small cohort of rTKA patients with rotating hinge implants comparing tibial cones with either short cemented stems or long press-fit stems, Jacquet et al. demonstrated that short cemented tibial stems combined with trabecular metal cones confer similar survivorship and better functional outcomes at a minimum of 5 years of follow-up [11]. In agreement with Jacquet et al., our tibial cohort demonstrated similar freedom from re-revisions and aseptic loosening. However, we found that the fully cemented stem-group had numerically superior freedom from all-cause re-revision compared to the hybrid group at latest follow-up. While abundant literature was published about outcomes of different cone designs, heterogeneity of surgical characteristics restricts the generalization of the results for other cone designs. Number of previous revisions to the same knee, different articulation designs and the use of stems of different fixation methods and lengths highly vary between each revision case.
Our study found a higher proportion of prior multiple revisions to the ipsilateral knee in the tibial cemented group. This finding is not surprising since multiple revisions might lead to higher metaphyseal bone loss that require bypassing the defect using fully cemented stems [9]. Interestingly, our regression model did not find lower re-revision risk for patients with index revisions suggesting that the use of cones with stems of different fixation methods provides a rigid structure in the present of moderate to severe bone loss in rTKA.
Our study results are novel since it is the first to report the use of a distinct regression model to account for patients’ baseline and surgical characteristics for both femoral and tibial cones. Both tibial and femoral cones demonstrated similar rates of freedom from aseptic re-revisions and explantation. These findings add to the efficacy of this novel porous cone design that can be used safely for both tibial and femoral bone loss. Moreover, the similar outcomes of different stem fixation methods both for femoral and tibial cones enable surgeons to choose the best modality on a case-by-case basis after evaluating the patient bone morphology and quality both pre and intra-operatively.
Limitations
Our study does have limitations. Given its retrospective nature, the results may be impacted by potential confounding variables and biases. Additionally, our analysis focused solely on outcomes of rTKA using a single cone system, so we were unable to compare this system to other cone systems. In the tibial cone cohort, a larger proportion of patients in the hybrid groups underwent their first revision surgery, contributing to selection bias. However, in multivariate regression, patients undergoing their first revision were not associated with lower re-revision rates. Overall, the number of included patients and outcomes event rates such as re-revisions that were examined in a binary logistic regression was too small to generate enough statistical power to yield statistical significance. Additionally, longer-term follow-up may be necessary to fully elucidate the effects of fixation selection on outcomes. Our analysis also may not have captured all revisions performed at outside institutions. While this raises the possibility that we underestimated the true revision rate, our findings are in line with previous studies, so missed cases were likely not to alter our findings. Finally, patient-reported outcomes questionnaires such as the Knee Society Score (KSS) and Knee Injury and Osteoarthritis Outcome Score (KOOS) were not available for analysis for a sufficient number of patients in this cohort.
Future work should focus on identifying if there is a difference in postoperative stability and complications between different systems. Although the present study represents, to our knowledge, the largest series of patients undergoing rTKA with the use of porous titanium metaphyseal cones, further studies should work towards generating larger databases to generate greater statistical power and to enable comparison with other augmentation systems for bone loss during rTKA.
Conclusions
The use of novel porous titanium femoral and tibial metaphyseal cones combined with stems in patients with moderate to severe bone defects undergoing complex revision total knee arthroplasty confers excellent results independent of stem fixation technique.
References
Vasso M, Beaufils P, Cerciello S, Schiavone Panni A (2014) Bone loss following knee arthroplasty: potential treatment options. Arch Orthop Trauma Surg 134:543–553. https://doi.org/10.1007/s00402-014-1941-8
Morgan-Jones R, Oussedik SIS, Graichen H, Haddad FS (2015) Zonal fixation in revision total knee arthroplasty. Bone Joint J 97:147–149. https://doi.org/10.1302/0301-620X.97B2.34144
Ponzio DY, Austin MS (2015) Metaphyseal bone loss in revision knee arthroplasty. Curr Rev Musculoskelet Med 8:361–367. https://doi.org/10.1007/s12178-015-9291-x
Malhotra R, Garg B, Kumar V (2011) Dual massive skeletal allograft in revision total knee arthroplasty. Indian J Orthop. https://doi.org/10.4103/0019-5413.82345
Anderson LA, Christie M, Blackburn BE et al (2021) 3D-printed titanium metaphyseal cones in revision total knee arthroplasty with cemented and cementless stems. Bone Jt J 103:150–157. https://doi.org/10.1302/0301-620X.103B6.BJJ-2020-2504.R1
Behery OA, Shing EZ, Yu Z et al (2021) Survivorship and radiographic evaluation of metaphyseal cones with short cemented stems in revision total knee arthroplasty. J Arthroplasty 37:330–335. https://doi.org/10.1016/j.arth.2021.10.027
Kamath AF, Lewallen DG, Hanssen AD (2015) Porous tantalum metaphyseal cones for severe tibial bone loss in revision knee arthroplasty. J Bone Jt Surg Am 97:216–223. https://doi.org/10.2106/JBJS.N.00540
Tetreault MW, Perry KI, Pagnano MW et al (2020) Excellent two-year survivorship of 3D-printed metaphyseal cones in revision total knee arthroplasty. Bone Jt J 102:107–115. https://doi.org/10.1302/0301-620X.102B6.BJJ-2019-1544.R1
Kang SG, Park CH, Song SJ (2018) Stem fixation in revision total knee arthroplasty: indications, stem dimensions, and fixation methods. Knee Surg Relat Res 30:187–192. https://doi.org/10.5792/ksrr.18.019
Patel AR, Barlow B, Ranawat AS (2015) Stem length in revision total knee arthroplasty. Curr Rev Musculoskelet Med 8:407–412. https://doi.org/10.1007/s12178-015-9297-4
Jacquet C, Ros F, Guy S et al (2021) Trabecular metal cones combined with short cemented stem allow favorable outcomes in aseptic revision total knee arthroplasty. J Arthroplasty 36:657–663. https://doi.org/10.1016/j.arth.2020.08.058
Denehy KM, Abhari S, Krebs VE et al (2019) Metaphyseal fixation using highly porous cones in revision total knee arthroplasty: minimum two year follow up study. J Arthroplasty 34:2439–2443. https://doi.org/10.1016/j.arth.2019.03.045
Engh GA, Ammeen DJ (1999) Bone loss with revision total knee arthroplasty: defect classification and alternatives for reconstruction. Instr Course Lect 48:167–175
Huten D (2013) Femorotibial bone loss during revision total knee arthroplasty. Orthop Traumatol Surg Res 99:S22-33. https://doi.org/10.1016/j.otsr.2012.11.009
Ewald (1989) The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res 2:2
Fehring TK, Odum S, Olekson C et al (2003) Stem fixation in revision total knee arthroplasty. Clin Orthop Relat Res 416:217–224. https://doi.org/10.1097/01.blo.0000093032.56370.4b
Bottner F, Laskin R, Windsor RE, Haas SB (2006) Hybrid component fixation in revision total knee arthroplasty. Clin Orthop Relat Res 446:127–131. https://doi.org/10.1097/01.blo.0000214418.36959.c5
Wang C, Pfitzner T, von Roth P et al (2016) Fixation of stem in revision of total knee arthroplasty: cemented versus cementless—a meta-analysis. Knee Surg Sport Traumatol Arthrosc 24:3200–3211. https://doi.org/10.1007/s00167-015-3820-4
Lei P, Hu R, Hu Y (2019) Bone defects in revision total knee arthroplasty and management. Orthop Surg 11:15–24. https://doi.org/10.1111/os.12425
Rodríguez-Merchán EC, Gómez-Cardero P, Encinas-Ullán CA (2021) Management of bone loss in revision total knee arthroplasty: therapeutic options and results. EFORT Open Rev 6:1073–1086. https://doi.org/10.1302/2058-5241.6.210007
Erivan R, Tracey R, Mulliez A et al (2021) Medium term clinical outcomes of tibial cones in revision knee arthroplasty. Arch Orthop Trauma Surg 141:113–118. https://doi.org/10.1007/s00402-020-03532-1
Suh C, Se L, Park J, Soo S (2013) The effect of simulated knee flexion on sagittal spinal alignment: novel interpretation of spinopelvic alignment. Eur Spine J. https://doi.org/10.1007/s00586-013-2661-4
Divano S, Cavagnaro L, Zanirato A et al (2018) Porous metal cones: gold standard for massive bone loss in complex revision knee arthroplasty? A systematic review of current literature. Arch Orthop Trauma Surg 138:851–863. https://doi.org/10.1007/s00402-018-2936-7
Chalmers BP, Malfer CM, Mayman DJ et al (2021) Early survivorship of newly designed highly porous metaphyseal tibial cones in revision total knee arthroplasty. Arthroplast Today 8:5–10. https://doi.org/10.1016/j.artd.2021.01.004
Geary MB, Macknet DM, Ransone MP et al (2020) Why do revision total knee arthroplasties fail? A single-center review of 1632 revision total knees comparing historic and modern cohorts. J Arthroplasty 35:2938–2943. https://doi.org/10.1016/j.arth.2020.05.050
Angerame MR, Jennings JM, Holst DC, Dennis DA (2019) Management of bone defects in revision total knee arthroplasty with use of a stepped, porous-coated metaphyseal sleeve. JBJS Essent Surg Tech 9:e14. https://doi.org/10.2106/JBJS.ST.18.00038
Brown NM, Bell JA, Jung EK et al (2015) The use of trabecular metal cones in complex primary and revision total knee arthroplasty. J Arthroplasty 30:90–93. https://doi.org/10.1016/j.arth.2015.02.048
Girerd D, Parratte S, Lunebourg A et al (2016) Total knee arthroplasty revision with trabecular tantalum cones: preliminary retrospective study of 51 patients from two centres with a minimal 2-year follow-up. Orthop Traumatol Surg Res 102:429–433. https://doi.org/10.1016/j.otsr.2016.02.010
Behery OA, Shing EZ, Yu Z et al (2021) Survivorship and radiographic evaluation of metaphyseal cones with short cemented stems in revision total knee arthroplasty. J Arthroplasty. https://doi.org/10.1016/j.arth.2021.10.027
Hernandez NM, Hinton ZW, Wu CJ et al (2021) Mid-term results of tibial cones. Bone Joint J 103:158–164. https://doi.org/10.1302/0301-620X.103B6.BJJ-2020-1934.R1
Kosse NM, van Hellemondt GG, Wymenga AB, Heesterbeek PJC (2017) Comparable stability of cemented vs press-fit placed stems in revision total knee arthroplasty with mild to moderate bone loss: 6.5-year results from a randomized controlled trial with radiostereometric analysis. J Arthroplasty 32:197–201. https://doi.org/10.1016/j.arth.2016.06.003
Funding
No funding was provided for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
I.S, C.O, J.W, P.H J.R have nothing to disclose. G.VH reports being a paid consultant for Smith&Nephew. S.M reports being a paid consultant for Zimmer and Intelijoint. R.S reports IP royalties from Smith & Nephew, being paid consultant for Smith & Nephew, Intelijoint, have stock options from Intelijoint, Gauss Surgical and receives research support from Smith & Nephew anddIntelijoint.
Ethical approval
The present study was exempt from human-subjects review by our Institutional Review Board (IRB).
Informed consent
N/A.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shichman, I., Oakley, C., Willems, J.H. et al. Novel metaphyseal porous titanium cones allow favorable outcomes in revision total knee arthroplasty. Arch Orthop Trauma Surg 143, 1537–1547 (2023). https://doi.org/10.1007/s00402-022-04645-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-022-04645-5