Abstract
Purpose
Interfragmentary strain influences whether a fracture will undergo direct and indirect fracture healing. Orthopedic trauma surgeons modulate strain and create optimal biomechanical environments for specific fracture patterns using fixation constructs. However, objective intraoperative interfragmentary strain measurement does not currently inform fixation strategy in common practice. This review identifies potential methods and technologies to enable intraoperative strain measurement for guiding optimal fracture fixation strategies.
Methods
PubMed, Scopus, and Web of Science were methodologically queried for manuscripts containing terms related to “bone fracture,” “strain,” “measurement,” and “intraoperative.” Manuscripts were systematically screened for relevance and adjudicated by three reviewers. Relevant articles describing methods to measure interfragmentary strain intraoperatively were summarized.
Results
After removing duplicates, 1404 records were screened initially. There were 49 manuscripts meeting criteria for in-depth review. Of these, four reports were included in this study that described methods applicable to measuring interfragmentary strain intraoperatively. Two of these reports described a method using instrumented staples, one described optical tracking of Kirschner wires, and one described using a digital linear variable displacement transducer with a custom external fixator.
Conclusion
The four reports identified by this review describe potential methods to quantify interfragmentary strain after fixation. However, further studies are needed to confirm the precision and accuracy of these measurements across a range of fractures and fixation methods. Additionally, described methods require the insertion and likely removal of additional implants into the bone. Ideally, innovations that measure interfragmentary strain intraoperatively would provide dynamic biomechanical feedback for the surgeon to proactively modulate construct stability.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fracture healing occurs either via direct (primary) or indirect (secondary) bone healing. Direct fracture healing, also known as intramembranous ossification, involves direct remodeling of the cellular structure of bone including lamellae, Haversian canals, and vessels [1]. Indirect fracture healing is a multistep process centered around cartilaginous callus formation and subsequent mineralization, resorption, and bone remodeling [1]. Healing mode is determined through the interplay of interfragmentary gapping and strain, with interfragmentary strain defined as the ratio of the fracture gap displacement after loading relative to the original fracture gap of the healing bone [2]. Depending on a variety of clinical factors, including fracture pattern, either direct or indirect fracture healing may be preferable. Direct fracture requires an interfragmentary gap of less than 0.01 mm [3] and interfragmentary strain of less than 2% [1, 4]. If direct healing criteria are not met, indirect fracture healing may occur at an interfragmentary strain of less than 10% [4] in accord with Perren’s strain theory with strains greater than 10% or large fracture gaps resulting in nonunion [5, 6].
Clinically, fixation strategy and construct stability determine the type of bone healing by controlling the interfragmentary gapping and strain. Often, direct fracture healing is achieved via direct anatomic reduction, compression, and absolute stability; conversely, fractures treated with a cast, bridge plate, intramedullary nail, or external fixator create an environment that favors indirect fracture healing [4]. However, in practice, direct and indirect healing can occur along a continuum as interfragmentary strain and displacement can vary throughout a fracture with comminution [7, 8].
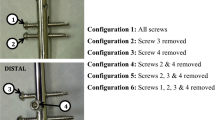
The approximate range of interfragmentary strain at which indirect fracture healing can occur is between 2 and 10%. However, it is unknown whether specific fracture types differ in their optimal strain environments for healing [7, 9]. For example, an in vivo ovine study concluded that with a larger fracture gap (2 mm or 6 mm) a more rigid fixation was preferable, while a smaller fracture gap (1 mm) achieved better healing under greater interfragmentary strain [10]; conversely, a more recent computational simulation study found that greater interfragmentary strain might be favorable for callus formation as part of indirect fracture healing for a larger, 3 mm, gap size but that same strain would cause excessive fibrous tissue differentiation and potentially lead to nonunion in a smaller, 1 mm, gap size [11]. One barrier to precisely determining optimal interfragmentary strain for the best fracture healing in clinical practice is the inability to dynamically measure interfragmentary strain intraoperatively as it is being modulated. The ability to measure interfragmentary strain intraoperatively would have both immediate clinical utility in objectively predicting which mode of fracture healing will occur and inform effective surgical strategies to direct the desired mode of healing, for example by guiding the number of screws affixing a bridge plate.
There is a long history of measuring the strain experienced by bone in the fields of orthopedics and biomechanics. There have been multiple studies describing how interfragmentary strain changes throughout fracture healing utilizing indirect measurements with strain gauges on external fixators [12,13,14,15,16,17,18]. Additionally, previous biomechanical work has directly measured in vivo strain in healthy bone, as has been systematically reviewed by Al Nazer et al. [19]. The techniques and sensors used to achieve direct strain measurements are highly varied including piezoresistive strain gauges, liquid metal strain gauge transducers, magnetic field-based sensors, and fiber optic sensors [20]. However, there is limited work identifying methods applicable to the operating room; therefore, the objective of this narrative review is to build upon prior evidence and specifically identify current methods, techniques, and technologies which could be applied to measuring interfragmentary strain intraoperatively to influence intraoperative decision making.
Methods
This narrative review was performed with influence from the Preferred Reporting Items for Systematic reviews and Meta-analyses (PRISMA) 2020 statement and checklist [21]. A search for relevant English language reports was performed in three databases: PubMed, Scopus, and Web of Science. The exact search strategy of each database is presented in Supplementary 1. In brief, records were included that contained the keywords “bone” and “fracture” anywhere, contained “strain” or an analogous terminology specifically in the title and “strain” anywhere, contained one of a list of keywords centered around “measure,” “assess,” or “gauge” anywhere, and contained some variation or analogous terminology in a list of keywords centered around “intraoperative,” “in vivo,” or “implant” anywhere. No restriction criteria were imposed on the search. The search was performed on August 11, 2022.
Records were manually screened for exclusion by title by one author trained in biomedical engineering, Author 1, and excluded if the title was clearly not related to the field of orthopedics or biomechanics. The abstracts of the remaining records were manually screened by Author 1 to exclude reports not describing measuring interfragmentary strain. Reports were retrieved for the remaining records along with additional reports from relevant citations of these reports and reviewed in full by Author 1 for methods with feasible applicability to direct, intraoperative interfragmentary strain measurement. These were subsequently reviewed by two addition authors (Author 2, Author 7) with consensus opinion determining final inclusion.
Given the qualitative nature of this review, a summary of the relevant portions of each included report is provided as the primary result of this review.
Results
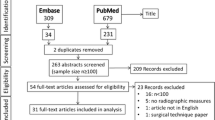
The results of the search and selection process are summarized in Fig. 1. Of the 44 reports that were assessed for eligibility from the initial databases search, 3 reports were included in this review. From 44 reviewed reports, 5 additional reports were identified and assessed of which 1 was ultimately included. Of the assessed reports that were excluded, the plurality (n = 16) was studies measuring the strain on the implants, which has a varying relationship with the actual interfragmentary strain and may occur only after significant interfragmentary strain causing fixation failure, as opposed to directly measuring interfragmentary strain. For example, a study by Gattiker et al. [22] described a novel wireless implantable passive strain sensor (WIPSS) that utilizes hydromechanical strain amplification which could be embedded in an orthopedic implant and read out by ultrasound. Another study by Greve et al. [23] developed and conducted in vitro tests on a prototype wireless surface acoustic wave strain sensor inserted into the entire length of a cannulated intramedullary nail for monitoring of bone healing. The second most common reason reports were excluded for utilizing methods only applicable in a benchtop study (n = 7). For example, Nabhani et al. [24] measured strain in a synthetic femur benchtop experiment using video tracking of visual surface markers, and Wongchai used a clip-type displacement transducer placed in the fracture gap of a plated, fractured synthetic femur in benchtop compression tests [2]. Less frequent reasons for exclusion are summarized in Fig. 1.
PRISMA 2020 style flow diagram summarizing results of search and report selection. Terminology is used as defined in the PRISMA 2020 statement [21]
The first included study described a method of measuring in vivo strain using staples affixed with resistance strain gauges wired into a Wheatstone bridge circuit by Buttermann et al. [25] in 1994. The goal of this study was to develop a method for long term in vivo strain measurement with less implantation time than cemented in vivo strain gauges [25]. Custom steel staples were manufactured, and strain gauges were epoxy bonded onto the top and bottom surfaces of the staple crown bridging between the two staple legs. The staples were first tested on the bench top in a steel beam by welding the staples onto the steel beam in comparison with strain gauges cemented directly onto the surface of the steel beam [25]. Additional bench top tests were performed with a bone beam of canine lateral femur to which the instrumented staples were impacted into predrilled holes and compared to a cemented strain gauge affixed parallel to the staple [25]. The staples were subsequently tested in vitro in canine lumbar vertebrae measuring facet joint strains in replication of and comparison to a previously described study using surface-mounted strain gauges [25]. Finally, in vivo testing was performed by implantation in the right L3 cranial articular process of 4 canines with verification of circuit at the time of implantation and formal testing during canine activities at 1 week and 4 weeks post-implantation. The instrumented staples were found to have a highly linear output with increasing loads, repeatable calibration within 5–10%, accuracy to within 10% for loads up to 100 N, and no measurable impact on the stiffness of bone as determined by the removal of redundant staples [25]. Buttermann et al. [25] concluded that one limitation of their study was determining the role of surgical artifact on the measurements of the staples.
The second study included, performed by Ekenman et al. [26] in 1998, also described a method of using staples affixed with resistance strain gauges in a Wheatstone bridge. The goal of this study was to demonstrate the validity of an instrumented staple strain measurement system for use in human tibiae. Titanium bone staples with two strain gauges mounted perpendicularly to the bottom of the staple crown were first compared to measurements by a digital micrometer in benchtop tests sheep cortical bone [26]. The staples were subsequently tested in vitro in whole sheep and pig tibiae four-point bending tests with strain gauges bonded to the bone surface serving as gold standards. This group’s results ultimately showed a direct linear relationship between strain measured by the staples and strain measured at the bone surface. They concluded that their method could be validly used to measure local bone strain in vivo (Table 1).
A study by Kaspar et al. [27] in 2005 examined the impact of interfragmentary movement on fracture healing following unreamed tibial nailing with an “angle stable” tibial nail created by modifying a commercially available tibial nail by adding threaded holes for 3.9-mm titanium locking bolts compared to “standard” unreamed tibial nailing with an unmodified tibial nail. This group measured interfragmentary movement using an infrared optical system to track percutaneously inserted 2.5-mm Kirschner wires inserted on either side of the fracture, mounted with reflective marker frames [27]. Initial calibration of the optical system was performed in vitro with an osteotomized cadaveric sheep tibia fixated with one of the two types of tibial nails and embedded in acrylate for axial compression, torsional, and bending tests with an accuracy of ± 0.1 mm in axial compression and shear displacements and ± 0.1° for torsional and bending angles [27]. The two tibial nails were then tested in vivo in 93 sheep osteotomized with a 3-mm gap. Interfragmentary movement measurements were recorded during ambulation starting on postop day 3 and up to 9 weeks. Using their optical system, this group was able to significantly differentiate the interfragmentary movement (reported as length of shear displacement or angle of torsional displacement as opposed to strain) of the two fixation methods in all dimensions tested [27]. They found that the angle stable tibial nail led to better functional outcomes which correlated with the significantly reduced interfragmentary movements compared to a standard unreamed tibial nail as measured by their optical system [27].
The final included study by Claes et al. [10] from 1997 evaluated the impact on fracture healing of interfragmentary gap size and movement in externally fixated metatarsi of sheep. Interfragmentary strain was measured intraoperatively using a digital linear variable displacement transducer (LVDT) placed between the two halves of a specially designed external fixator [10]. Subsequent weekly in vivo testing during ambulation was performed using the same LVDT-external fixator construct [10]. They found that different interfragmentary strain and gap size pairs set at the time of fixation consistently correlated with different trends of fracture healing over eight weeks and that the favorability of a 7% strain or 31% strain healing environment depended on the gap size comparing 1 mm, 2 mm, or 6 mm gaps [10]. They concluded that the higher interfragmentary strain with the smallest gap tested led to the greatest mechanical stiffness overall, while the lower interfragmentary strain was favorable for healing of the larger fracture gaps. However, this solution for strain measurement is not directly translatable to completely internal fixation.
Discussion
Current methods with applicability to measuring intraoperative interfragmentary strain were highlighted in this review. We were only able to identify four relevant articles, all of which were experimental. There remains a considerable unmet need to develop clinically relevant technology to measure intraoperative interfragmentary strain and guide the surgeon in constructing the desired biomechanical environment for fracture healing, particularly for indirect healing.
Among the four manuscripts identified, three distinct methodologies were identified. All three of these methods were tested in their respective studies and found to have acceptable accuracy and precision [10, 25,26,27]. However, in the reviewed studies, the instrumented staples were never tested specifically in a fractured bone, and the other two methods were only tested in idealized, controlled fracture models [10, 25,26,27]. Therefore, further study is needed to determine whether any of these methods could be applied in the intraoperative setting with a wide variety of fractures, particularly the more complex fracture patterns with significant commination or bone loss where interfragmentary strain measurements might have the largest impact on real-time treatment decisions.
Each of the three methods has significant potential limitations. All three methods require placement of additional implants in the bone. Clinically, the difficulty and additional surgical time of this may vary between the methods and depend on the complexity of the fracture pattern. Additionally, the utilization of these methods may necessitate varying degrees of soft tissue insult during insertion or from additional required exposure. The optical Kirschner wire method may be least limited by this if they are inserted percutaneously. Depending on the number, size, and location of bone fragments, the instrumented staples method may require minimal or entirely prohibitive additional exposure and tissue disruption. Due to the larger size of the additional implants, the digital LVDT method described by Claes et al. [10] may be most limited by additional tissue disruption as well as additional cost limitations due to the larger device. While the instrumented staples may not require removal given their compact size, additional hardware that provides no additional stability may present an unwarranted additional nidus of infection.
The instrumented staple methodologies potentially have the greatest advantage in efficiency as they are applied as a single piece of hardware [25, 26]. Additionally, this method may provide an advantage in accuracy and minimal need for calibration as measurements would always be performed in direct contact with the bone cortex. However, a limitation in the ease of use of this method relative to the other identified methods is the need for wires connecting to the staples at the fracture site to exit the sterile field to complete the circuit which necessitates the assistance of additional operating room staff beyond the surgical team to operate this system.
The method described by Claes et al. [10] as implemented in their included study is only immediately applicable to the use of an external fixator. However, with some modification, the same principles behind their technique could be used to temporarily fix a LVDT parallel to an interfragmentary gap. This method still may be limited by the invasiveness and additional bone injury caused by the temporary fixation. Additionally, significant calibration would be needed with this method based on the variation in the geometric relationship between the interfragmentary gap, hardware connecting the transducer to the bone, and the offset distance from the transducer to the bone. This method, like the instrumented staples method, may have the drawback of wires leaving the sterile field unless a wireless LVDT is used.
The optical tracking method described by Kaspar et al. [27] has a unique advantage over the other methods described in that it does not require any electrical components to span the sterile field. Also, this method only relies on components which surgeons already routinely use. Additionally, this technique is not limited to the measurement of strain in one dimension, as was demonstrated by Kaspar et al. [27] using this technique in axial compression, torsional rotation, and multidirectional bending tests. A drawback of this method is the need to calibrate the mechanical relationship between any strain on an interfragmentary gap and the resultant movement of the reflective markers on the Kirschner wires which will be technically dependent on the location with respect to the fracture gap, angle, and depth of placement of the Kirschner wires. Additionally, this method may be prohibited in some cases depending on the size of the unstable segment.
Regardless of the method used to measure the interfragmentary strain, a yet unstudied factor is how a surgeon applying force intraoperatively would test the interfragmentary strain allowed by a construct. If there is any instability in the fixation, whether intended or unintended, an initial stress–strain relationship will have an elastic modulus determined by the surrounding soft tissue envelope in the range of displacement where there is instability in the fixation and movement of the bone relative to the fixation hardware. Further displacement will necessitate force transmission from the bone to the implanted hardware. At this point, the overall stress–strain relationship of the construct will have a stepwise increase in stress with an orders of magnitude higher elastic modulus determined by the entire bone-fixation construct as opposed to the surrounding soft tissue envelope prior to transmission of force to the implanted hardware (Fig. 2). Therefore, the surgeon must understand which specific part of the overall stress–strain relationship they are testing when applying forces intraoperatively meant to simulate clinically relevant activities such as full or partial weightbearing.
Not-to-scale representation of the theoretical strain dependent changing elastic modulus in a nonrigid fixation where the initial stress–strain relationship is governed by surrounding soft tissue before the stress–strain relationship is governed by the bone-hardware unit. Figure generated in MATLAB R2022b (The MathWorks, Inc.)
Theoretically, an intraoperative strain gauge would have clinical utility even if intraoperatively applied forces were not quantitatively measured. Surgeons could readily determine whether they are testing any instability in the fixation of the implanted hardware or the elastic modulus of the entire bone-fixation construct by feeling the “step up” in the stress–strain relationship when force starts to be transmitted to the implanted hardware. In many cases, the most clinically relevant information is gained in measuring the allowed strain before force is transmitted to the implanted hardware. Furthermore, simulation of the forces caused by relevant activities such as weight-bearing should reasonably be able to be approximated by manual manipulation by a surgeon. Further testing of these hypotheses is warranted once a validated intraoperative interfragmentary strain gauge is developed.
Ultimately, the techniques reviewed here have the potential to meet many of the requirements for what we propose would be an ideal intraoperative, interfragmentary strain gauge. An ideal strain gauge must have minimized complexity both with respect to the implants and technique required to use. It must be generally applicable to a variety of fracture patterns and fixation techniques yet quick to apply and calibrate to the specific fracture. It must not significantly damage surrounding tissue, impair healing, or add unmitigated risk to the patient. Finally, it must provide precise, accurate, dynamic measurements, though thresholds for the accuracy required to have clinical impact will require further study to determine.
Conclusion
Three unique methods applicable to measuring interfragmentary strain intraoperatively were identified in this review. Each of these methods has advantages and disadvantages, with none of them currently being ready for implementation in the operating room. While these methods show promise, there remains relatively little research into addressing the ability of fracture surgeons to quantitatively measure interfragmentary strain intraoperatively. Addressing this unmet need would have immediate clinical and research applications.
References
Marsell R, Einhorn TA (2011) The biology of fracture healing. Injury 42:551–555. https://doi.org/10.1016/j.injury.2011.03.031
Wongchai B (2014) Study of the interfragmentary strain and the interfragmentary modulus with changing the distance between plate and femur. Am J Appl Sci 11:356–361. https://doi.org/10.3844/ajassp.2014.356.361
Shapiro F (1988) Cortical bone repair. The relationship of the lacunar-canalicular system and intercellular gap junctions to the repair process. J Bone Joint Surg Am 70:1067–1081
Hak DJ, Toker S, Yi C, Toreson J (2010) The influence of fracture fixation biomechanics on fracture healing. Orthopedics 33:752–755. https://doi.org/10.3928/01477447-20100826-20
Foster AL, Moriarty TF, Zalavras C et al (2021) The influence of biomechanical stability on bone healing and fracture-related infection: the legacy of Stephan Perren. Injury 52:43–52. https://doi.org/10.1016/j.injury.2020.06.044
Perren SM (2002) Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg Br 84:1093–1110. https://doi.org/10.1302/0301-620x.84b8.13752
Cheal EJ, Mansmann KA, DiGioia AM et al (1991) Role of interfragmentary strain in fracture healing: ovine model of a healing osteotomy. J Orthop Res 9:131–142. https://doi.org/10.1002/jor.1100090116
Claes LE, Heigele CA (1999) Magnitudes of local stress and strain along bony surfaces predict the course and type of fracture healing. J Biomech 32:255–266. https://doi.org/10.1016/s0021-9290(98)00153-5
Hente RW, Perren SM (2021) Tissue deformation controlling fracture healing. J Biomech 125:110576. https://doi.org/10.1016/j.jbiomech.2021.110576
Claes L, Augat P, Suger G, Wilke HJ (1997) Influence of size and stability of the osteotomy gap on the success of fracture healing. J Orthop Res 15:577–584. https://doi.org/10.1002/jor.1100150414
Miramini S, Zhang L, Richardson M et al (2016) The relationship between interfragmentary movement and cell differentiation in early fracture healing under locking plate fixation. Australas Phys Eng Sci Med 39:123–133. https://doi.org/10.1007/s13246-015-0407-9
Burny F, Donkerwolcke M, Bourgois R et al (1984) Twenty years experience in fracture healing measurement with strain gauges. Orthopedics 7:1823–1826. https://doi.org/10.3928/0147-7447-19841201-08
Grasa J, Gómez-Benito MJ, González-Torres LA et al (2010) Monitoring in vivo load transmission through an external fixator. Ann Biomed Eng 38:605–612. https://doi.org/10.1007/s10439-009-9889-5
Kristiansen B, Borgwardt A (1992) Fracture healing monitored with strain gauges. External fixation of 7 humeral neck fractures. Acta Orthop Scand 63:612–614. https://doi.org/10.1080/17453679209169719
Nishimura N (1984) Serial strain gauge measurement of bone healing in hoffmann® external fixation. Orthopedics 7:677–684. https://doi.org/10.3928/0147-7447-19840401-21
Cunningham JL, Evans M, Kenwright J (1989) Measurement of fracture movement in patients treated with unilateral external skeletal fixation. J Biomed Eng 11:118–122. https://doi.org/10.1016/0141-5425(89)90120-9
Ogrodnik PJ, Moorcroft CI, Thomas PB (2001) A fracture movement monitoring system to aid in the assessment of fracture healing in humans. Proc Inst Mech Eng H 215:405–414. https://doi.org/10.1243/0954411011535984
Jenkins P, Nokes L (1994) The use of strain gauges to measurebone fracture healing—a review. Curr Orthop 8:116–118. https://doi.org/10.1016/S0268-0890(05)80065-9
Al Nazer R, Lanovaz J, Kawalilak C et al (2012) Direct in vivo strain measurements in human bone-a systematic literature review. J Biomech 45:27–40. https://doi.org/10.1016/j.jbiomech.2011.08.004
Roriz P, Carvalho L, Frazão O et al (2014) From conventional sensors to fibre optic sensors for strain and force measurements in biomechanics applications: a review. J Biomech 47:1251–1261. https://doi.org/10.1016/j.jbiomech.2014.01.054
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. https://doi.org/10.1136/bmj.n71
Gattiker F, Umbrecht F, Neuenschwander J et al (2008) Novel ultrasound read-out for a wireless implantable passive strain sensor (WIPSS). Sens Actuators, A 145–146:291–298. https://doi.org/10.1016/j.sna.2007.09.003
Greve DW, Oppenheim IJ, Chen AF (2012) An instrumented intramedullary implant to monitor strain in fracture healing. In: 2012 IEEE international Ultrasonics symposium. IEEE, p 1220–1223
Nabhani F, Bradley EJ, Hodgson S (2010) Comparison of two tools for the measurement of interfragmentary movement in femoral neck fractures stabilised by cannulated screws. Robot Comput Integr Manuf 26:610–615. https://doi.org/10.1016/j.rcim.2010.06.014
Buttermann GR, Janevic JT, Lewis JL et al (1994) Description and application of instrumented staples for measuring in vivo bone strain. J Biomech 27:1087–1094. https://doi.org/10.1016/0021-9290(94)90225-9
Ekenman I, Halvorsen K, Westblad P et al (1998) The reliability and validity of an instrumented staple system for in vivo measurement of local bone deformation. An in vitro study. Scand J Med Sci Sports 8:172–176. https://doi.org/10.1111/j.1600-0838.1998.tb00188.x
Kaspar K, Schell H, Seebeck P et al (2005) Angle stable locking reduces interfragmentary movements and promotes healing after unreamed nailing. Study of a displaced osteotomy model in sheep tibiae. J Bone Joint Surg Am 87:2028–2037. https://doi.org/10.2106/JBJS.D.02268
Funding
No funds, grants, or other support was received.
Author information
Authors and Affiliations
Contributions
JH, AR, and MDB contributed to methodology; AR, JH, and MDB contributed to formal analysis and investigation; AR contributed to writing-original draft preparation; AR, JH, MB, AP, SC, and CP contributed to writing—review and editing; and MDB contributed to supervision.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or nonfinancial interests to disclose.
Consent to participate
The authors declare that this work complies with all the laws of the country in which it was performed.
Ethical approval
This is a narrative, literature review study deemed exempt by the Duke University IRB.
Informed consent
This review study of previously published literature did not involve any participants and therefore did not require any consenting.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rechenmacher, A.J., Helmkamp, J., Brown, M. et al. Interfragmentary strain measurement post-fixation to guide intraoperative decision making: a narrative review. Eur J Orthop Surg Traumatol 33, 3299–3305 (2023). https://doi.org/10.1007/s00590-023-03605-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-023-03605-y