Abstract
Purpose
To describe the surgical technique and the outcome of a case series of nonunion and malunion of distal femur fractures treated with an endosteal medial plate combined with a lateral locking plate and with autogenous bone grafting.
Methods
We retrospectively analyzed a series of patients with malunion or nonunion of the distal femur treated with a medial endosteal plate in combination with a lateral locking plate, in a period between January 2011 and December 2019, Database from chart review was obtained including all the clinical relevant available baseline data (demographics, type of fracture, mechanism of injury, time from injury to surgery, number of previous surgical procedures, type of bone graft, and type of lateral plate). Time to bone healing, limb alignment at follow-up and complications were documented.
Results
Ten patients were included into the study: 7 male and 3 female with mean age of 48.3 years (range 21–67). The mechanism of trauma was in 8 cases a road traffic accident and in 2 cases a fall from height. According to AO/OTA classification 5 fractures were 33 A3, 3 were 33 C1, 1 was 33 C2 and 1 was 33 C3. The average follow up was 13.5 months. In all cases but one bony union was achieved. Bone healing was observed in average 3.3 months after surgery. No intraoperative or postoperative complications were reported.
Conclusion
A medial endosteal plate is a useful augmentation for lateral plate fixation in nonunion or malunion following distal femur fractures, particularly in cases of medial bone loss, severe comminution, or poor bone quality.
Level of evidence
Level IV (retrospective case series).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Distal femoral fractures represent 3–6% of all femoral fractures [1]. Surgical treatment consistently demonstrated better outcomes compared to nonoperative management [2]. Several surgical techniques are available, such as lateral buttress plating, lateral fixed-angle plating, retrograde intramedullary nailing, association of nail and plate or the combination of a lateral and medial plate, external fixation and primary total knee arthroplasty [3]; however, the ideal treatment for this type of fracture is still controversial [4]. Indeed, distal femur fractures are in most of cases difficult to treat [5, 6], especially in cases with extensive medial cortical bone loss. Nonunions and malunions of the distal femur after surgical fixation are rare but potentially catastrophic complications that result in significant loss of function and severe disability [7, 8].
Nonunion is the most frequent complication and can occur from 5 to 19% of cases [4, 9, 10]. The principal causes of nonunion include inadequate fracture fixation, infection, excessive separation of soft tissue during the procedure, which undermines vascular supply at the fracture site, and patient-related factors, such as advanced age, smoking, diabetes, vascular disease, non-steroidal anti-inflammatory drugs and steroid use [11,12,13,14]. Although the use of fixed angle implants provides rigid construct that better withstands bending forces, implant failure is still possible because of significant eccentric load [6, 14].
Malunions are mainly related to improper metalwork and surgeon’s experience [15]. Comminution at the fracture site and particularly medial bone loss are a common problem, that quite often leads to secondary screw loosening, varus collapse, and subsequent hardware failure [16].
Nonunions and malunions can be addressed by several methods [17], depending on the pathological findings and surgeon’s confidence with specific implants. The mostly used fixation technique consists of fixed angle implants with cancellous autograft [17]. Recently, composite fixation or augmented fixation that foresee the association of nails and plates [18], both medial and lateral plates [19], or an endosteal plate associated with lateral plate [20, 21], are becoming more common. The original description of the technique by Mast et al. [22] consisted of a medial contoured intra-medullary plate to augment standard lateral plate fixation; this technique was originally used for distal femur nonunion, and for pathologic fractures [23]. Biomechanical studies [24] showed superiority of composite fixation respect to traditional lateral fixation.
The aim of the present study was to evaluate the efficacy of a modified Mast’s technique for the treatment malunion and nonunion of the distal femur. The hypothesis of the study was that combination of an endosteal plate associated with a lateral plate is effective in promoting healing of malunion and nonunion of distal femur fractures.
Materials and methods
Study design
The study was designed as an observational retrospective study without control group (case series).
Participants
All the patients with a malunion or nonunion of the distal femur treated by combination of an endosteal plate and a lateral plate between January 2011 and December 2019 were considered eligible for the study. Nonunion was defined as an unhealed fracture with no clinical or radiographic signs of progression to healing, believed to have no chance for further healing without additional surgical intervention. Nonunion was confirmed by plain radiographs, CT, or by a combination of modalities, defined as an unhealed fracture with no radiographic signs of osseous union. Instead malunion was defined as fractured healed in an abnormal position, which can lead to impaired function of the bone or limb. Inclusion criteria were nonunion, or malunion of the distal femur associated with functional disability in daily activities. Exclusion criteria were septic nonunions, presence of growth nuclei and previously non deambulatory patients.
Most of the patients in our cohort had atrophic nonunion with insufficient medial bone support. This was the key factor for the choice for this type of surgical intervention because endosteal plating is able to provide medial column support and adequate alignment of the distal femoral metaphysis.
Surgical technique
All the surgical procedures were performed by three of the senior authors (M.O, E.J., A.C).
A standard lateral approach, with preservation of the soft-tissue sleeve and debridement of avascular bone, was used in all patients. A tibial tuberosity osteotomy was performed if severe knee joint stiffness was present to allow better articular reduction. At the end of the procedure the tuberosity was fixed in a more proximal position to achieve greater knee flexion.
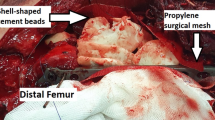
An endosteal plate (DCP or LCP 4.5 mm plate; DePuy Synthes, West Chester, PA, USA) was introduced through the bone defect at the nonunion or osteotomy site, first in a retrograde direction inside the femoral canal until it overlapped the bone gap and reached the midshaft; then it was impacted distally into the epiphyseal fragment, inverting the insertion direction. The length of the medial endosteal plate is assessed by keeping it in front of the femur while doing AP fluoroscopic images at the knee and at then at the most proximal aspect of the plate, making sure that it bypasses the nonunion or malunion site. The plate is then contoured until it matches the endosteal surface on AP fluoroscopy. The endosteal plate was adequately shaped into the femoral canal in order to match the medial cortex, ending on the medial condyle [25]. The endosteal plate modelling was achieved with plate bending press (DePuy Synthes, West Chester, PA, USA) (Fig.1).
A “picador” (ball spike pusher) was used to advance the endosteal plate and once it was centered on the fracture defect a lateral plate was positioned. For the lateral support we used a condylar blade-plate (CBP, DePuy Synthes) or an LCP Condylar Plate (LCP–CP, DePuy Synthes).
The intramedullary plate should be maintained as close as possible to the endosteal portion of the medial cortex, to act as a support. At this aim, Mast et al. [22] utilized the schüli nut (DePuy Synthes), a device designed to lock a 4.5 mm cortical screw at a 90° angle, thus preventing toggling in the non-locking hole of the CBP. As the Schüli device was not available in our country, we overcame this issue using nuts that engaged cortical screws and buttressed the endosteal plate towards the medial cortex. Using the LCP–CP plate, nuts are not necessary and the endosteal plate can be pushed towards the medial cortex by a locking screw of appropriate length that pushes the endosteal plate. Cortical screws of 4.5 mm were placed through holes in both plates in a quadrilateral implant configuration. Screws were positioned using the method described by Matelic et al. [26], in which the lateral cortex is drilled and a k-wire is used to guide the direction of the drill and screw through a hole in the intramedullary plate. These screws must not be placed straight across but should be positioned on an angle so that they barely fit through the screw hole, blocking the plate itself, thus preventing torsion or shortening between the two plates. To avoid shortening, the endosteal plate was further supported by a proximal screw at the end of the construct and by the blade plate distally.
Autologous bone graft was harvested from the contralateral femur, as a separate procedure, or from the same femur with the Reamer–Irrigator–Aspirator (RIA) and placed into the bone defect to induce bone formation.
Antero-posterior and lateral radiographs were obtained after surgery to confirm reduction and the correct position of the implants.
In all patients, continuous passive motion of the knee was started the day after surgery. Partial weight-bearing was allowed in the early postoperative period and progressively increased depending on radiographic findings during the following 8 weeks.
Outcome measures
The primary outcome for this study was to assess radiographic bone union in distal femur nonunions or malunions with the association of a medial endosteal plate to a lateral plate.
For all patients included into the study, medical records and preoperative radiographs were reviewed to identify fracture patterns according to AO/OTA fracture classification, previous surgical procedures, time to surgery, and implant type. Postoperative radiographs were evaluated to assess coronal and sagittal alignment. No Postoperative complications were recorded including loss of reduction, infection and reoperation rate. Union rate was determined by radiographic evidence of healing in 3 of 4 cortices and by clinical evidence of weight-bearing without pain as reported at follow-up visits. Limb alignment was assessed at the last follow-up radiological exam.
Data analysis
Descriptive statistics were reported as means and standard deviations for normally distributed data as assessed by Shapiro–Wilk test. Otherwise, medians and ranges were used. Categorical variables were expressed as frequencies and percentages.
Results
A total of 10 patients were included. There were 7 men and 3 women. The mean age was 48.3 years (range, 21–67 years) (Table 1).
The mechanism of injury was motor vehicle accident in 8 patients and in 2 patients a fall from height. Five patients had associated fractures. According to AO/OTA classification the initial fractures were 5 fractures 33A3, 3 were 33C1, 1 was 33C2 and 1 was 33C3. One patient, who had a concomitant neoplastic disease, suffered from an open Gustilo C2. Patients have undergone a median of 2 (range, 1 to 7) previous unsuccessful surgical procedures to fix the initial fracture or to correct the nonunion or malunion without success. All the malunions and nonunions were associated with severe deformities on the sagittal and coronal planes.
The intramedullary plate (4.5 mm tibial DCP or Locking Compression Plate De Puy Synthes) was associated on the lateral side with a CBP in 8 patients, with a LISS plate in 1, and with a LCP Condylar Plate 4.5/5.0 in another. Bone graft was obtained using RIA (reamer-irrigator-aspirator; De Puy Synthes) from the contralateral femur in 9 patients, while 1 patient had bone grafting from posterior iliac crest.
The mean follow-up was 13.5 months.
Fracture union occurred at an average 3.3 months from the surgery. Treatment was unsuccessful on the patient with the C2 open fracture who also had a concomitant colon adenocarcinoma with hepatic metastasis that died 12 months after the initial treatment. In this case, the blade plate failed at six months after surgery, but function was maintained. All the patients but one had a range of motion from full extension to more than 90° of flexion, including the patient with unsuccessful fracture union. In three patients the pre-operative shorthening was not completely corrected and a residual shortening of 1–2 cm persisted (Table 2). No patient needed reoperation.
Example are shown in Figs. 2, 3, 4 and 5.
Male patient 56 years old; road traffic injury, A lateral x-ray views of a 33 A 3 fracture of distal femur, B DCO with external fixation. C Treatment with circular external fixator 1 month after DCO. D, E 6 months after the trauma and 45 days after the removal of circular external fixator x-rays and CT-3D shows a non unon with severe medial cortex deficit
Male patients 56 years old; road traffic injury. A AP postoperative x-ray view (surgery was performed 8 months after the car injury). B Lateral post op view. C AP x-ray view at 6 months; (Notice that tibial tuberosity was elevated to gain access to the distal femur). D Lateral x ray view at 6 months showing healing in 3 of 4 cortices; patient was able to bear weight without pain
Women 50 years old; road traffic injury. A Long leg view (notice the deformity of the left lower limb and rigth foot; patient was not able to walk from 6 months). B Ap x-ray view of the left distal femur. Pin tracts of external fixator that was the only fixation performed in this case. C CT scan at 8 months showing malunion of the distal femur
Discussion
Bone healing in distal femur fractures can be challenging to achieve. Local factors including metaphyseal bone loss, compromised bone vascular supply, mechanical issues, infections and patient-related factors like diabetes, obesity and smoking may lead to nonunion of the supracondylar femur fracture [27, 28]. This is a severe complication that can be associated with varus deformity, pain, loss of function and severe disability for the patient.
Treatment strategy in malunions and nonunions of distal femur is based on the achievement of medial cortex stability. Single lateral locked plate does not always provide adequate stability and is burdened with a high failure rate [17, 29]. In reason of this, the combination of an endosteal and a lateral plate is a versatile and successful technique to treat distal femur malunions and nonunions, where medial cortical bone loss makes standard plating insufficient to maintain adequate stability to reach bone healing [30].
The endosteal plate technique was first described in 1989 by Mast et al. [22], in an effort to diminish the eccentric loads on the lateral plate and to sustain the insufficient medial cortex. This implant combination creates a construct that temporarily supplies the bone loss of the medial cortex. This construct, ideally, is able to better resists to bending and torsional forces, especially if interlocked [8, 24, 26,27,28]. These statements were validated and confirmed by a biomechanical study, which showed that the use of an endosteal 4.5 mm plate combined with a lateral plate provides increased axial and rotational stability with lower gap motion, and decreased displacement at the fracture site [25].
According to our experience, the endosteal plate, once it reaches the distal epiphyseal fragment, automatically corrects the hyperextension and the varus or valgus malalignment of the distal fragment Table 1. Another advantage of this technique is the possibility to obtain an enhanced support through the same lateral surgical approach, without further dissection.
Matelic et al. [26], in a case series, treated 7 distal femoral nonunions with the endosteal plate technique and achieved a complete bone healing in all cases. Similar results were reported by Bergin et al. [21] in 7 patients with distal femur nonunions treated with the Mast’s technique.
The association of an endosteal plate to a lateral plate is a construct that better withstand the forces because the plates are interlocked by screws that traverse both plates and by the blocking screws or nuts that push the endosteal plate against the medial cortex. The association of a medial endosteal plate to a lateral plate could appear apparently very sophisticated, but is not so demanding for the surgeon [25].
There are other technical solutions to treat distal femur nonunions with deficiency of the medial cortex support. One of these is the addition of a medial plate by a second surgical approach. However, an additional medial approach may add a vascular insult on the medial aspect of distal femur, a more aggressive periosteal devascularization on the bony fragment and above all the medial plate has not any mechanical effect on correcting the femoral axis. The use of an intramedullary nail, as endosteal substitute for a deficient medial cortex, combined with a lateral locked plate in the distal femur, was described by Spitler et al. [20], who reported good results in the treatment of acute fractures and nonunions of the distal femur. Despite this, intramedullary nails in femoral epiphyseal regions are not canal-filling, do not align the distal segment as plates do and can lead to some degree of malreduction due to secondary axial and torsional deforming forces [25]. Further, retrograde intramedullary nail has the disadvantage of violating the knee joint. In addition to the other issues, in the presence of other implants, such as some total knee or hip arthroplasties and comminuted condyle femoral fractures, retrograde nailing technique is not always possible.
Ilizarov bone transport and tumoral total knee arthroplasties are other possible treatment options [31, 32]. Ilizarov external fixation presents some advantages including minimal soft tissue disruption, stable fixation and early weight-bearing. This technique is particularly effective in patients with infection, limb shortening or deformity. Nevertheless, Ilizarov external fixation technique has a long learning curve and requires strict patient compliance with frequent follow-up [33, 34].
Arthroplasty for distal femoral nonunion gained popularity related to good pain relief and return to ambulation and is considered a suitable option, especially as a salvage procedure in elderly patients [35]. Despite good results, this surgical procedure is very challenging, because of difficult exposure due to previous scars and fibrosis, and the standard landmarks for assessing axial and rotational alignment of components may be distorted after fracture; furthermore, the durability of these implants remains inferior to that of primary TKA implanted for other conditions [36]. What is more, massive surgical exposure, long operative time, and compromised soft tissues might lead to an increased risk of postoperative infection.
The present study has some limitations, mainly related to the retrospective design and the small sample size. Indeed, further studies with larger sample size and comparative biomechanical and clinical studies would be necessary to confirm the efficacy of this technique.
Conclusions
The combination of an endosteal plate with a lateral plate associated with bone graft is an efficient technique for the treatment of distal femur nonunions or malunions. The endosteal plate, adequately shaped, aligns and stabilizes the distal segment, improves stability of the lateral plate and provides adequate support to the deficient medial cortex, thus offering a viable solution for these challenging situations.
References
Court-Brown CM, Caesar B (2006) Epidemiology of adult fractures: a review. Injury 37(8):691–697. https://doi.org/10.1016/j.injury.2006.04.130
Kregor PJ, Stannard J, Zlowodzki M, Cole PA, Alonso J (2001) Distal femoral fracture fixation utilizing the Less Invasive Stabilization System (L.I.S.S.): the technique and early results. Injury 32:32–47. https://doi.org/10.1016/S0020-1383(01)00182-6
Griffin XL, Parsons N, Zbaeda MM, Mcarthur J (2015) Interventions for treating fractures of the distal femur in adults. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD010606.pub2
Koso RE, Terhoeve C, Steen RG, Zura R (2018) Healing, nonunion, and re-operation after internal fixation of diaphyseal and distal femoral fractures: a systematic review and meta-analysis. Int Orthop 42(11):2675–2683. https://doi.org/10.1007/s00264-018-3864-4
Dar GN, Tak SR, Kangoo KA, Halwai MA (2009) Bridge plate osteosynthesis using dynamic condylar screw (DCS) or retrograde intramedullary supracondylar nail (RIMSN) in the treatment of distal femoral fractures: comparison of two methods in a prospective randomized study. Ulus Travma Ve Acil Cerrahi Derg Turk J Trauma Emerg Surg TJTES 15(2):148–153
Henderson CE, Kuhl LL, Fitzpatrick DC, Marsh JL (2011) Locking plates for distal femur fractures: is there a problem with fracture healing? J Orthop Trauma 25(Supplement 1):S8–S14. https://doi.org/10.1097/BOT.0b013e3182070127
Brinker MR, Trivedi A, O’Connor DP (2017) Debilitating effects of femoral nonunion on health-related quality of life. J Orthop Trauma 31(2):e37–e42. https://doi.org/10.1097/BOT.0000000000000736
Lynch JR, Taitsman LA, Barei DP, Nork SE (2008) Femoral nonunion: risk factors and treatment options. J Am Acad Orthop Surg 16(2):88–97. https://doi.org/10.5435/00124635-200802000-00006
Ricci WM, Streubel PN, Morshed S, Collinge CA, Nork SE, Gardner MJ (2014) Risk factors for failure of locked plate fixation of distal femur fractures: an analysis of 335 cases. J Orthop Trauma 28(2):83–89. https://doi.org/10.1097/BOT.0b013e31829e6dd0
Zlowodzki M, Bhandari M, Marek J, Cole PA, Kregor PJ (2006) Operative treatment of acute distal femur fractures: systematic review of 2 comparative studies and 45 case series (1989 to 2005). J Orthop Trauma 20(5):366–371. https://doi.org/10.1097/00005131-200605000-00013
Castillo RC, Bosse MJ, MacKenzie EJ, Patterson BM (2005) Impact of smoking on fracture healing and risk of complications in limb-threatening open tibia fractures. J Orthop Trauma 19(3):151–157. https://doi.org/10.1097/00005131-200503000-00001
Murnaghan M, Li G, Marsh R (2006) Nonsteroidal anti-inflammatory drug-induced fracture nonunion an inhibition of angiogenesis? J Bone Jt Surg 88(suppl_3):140–147. https://doi.org/10.2106/JBJS.F.00454
Bhandari M, Fong K, Sprague S, Williams D, Petrisor B (2012) Variability in the definition and perceived causes of delayed unions and nonunions: a cross-sectional, multinational survey of orthopaedic surgeons. J Bone Jt Surg 94(15):e109. https://doi.org/10.2106/JBJS.K.01344
Henderson CE, Lujan TJ, Kuhl LL, Bottlang M, Fitzpatrick DC, Marsh JL (2010) Mid-America Orthopaedic Association Physician in Training Award: healing complications are common after locked plating for distal femur fractures. Clin Orthop 469(6):1757–1765. https://doi.org/10.1007/s11999-011-1870-6
Agrawal A, Kiyawat V (2017) Complex AO type C3 distal femur fractures: results after fixation with a lateral locked plate using modified swashbuckler approach. Indian J Orthop 51(1):18. https://doi.org/10.4103/0019-5413.197516
Moloney GB, Pan T, Van Eck CF, Patel D, Tarkin I (2016) Geriatric distal femur fracture: Are we underestimating the rate of local and systemic complications? Injury 47(8):1732–1736. https://doi.org/10.1016/j.injury.2016.05.024
Ebraheim NA, Martin A, Sochacki KR, Liu J (2013) Nonunion of distal femoral fractures: a systematic review: nonunion distal femoral fractures. Orthop Surg 5(1):46–50. https://doi.org/10.1111/os.12017
Attum B, Douleh D, Whiting PS et al (2017) Outcomes of distal femur nonunions treated with a combined nail/plate construct and autogenous bone grafting. J Orthop Trauma 31(9):e301–e304. https://doi.org/10.1097/BOT.0000000000000926
Sain A, Sharma V, FarooqueMuthukumaranPattabiraman KVK (2019) Dual plating of the distal femur: indications and surgical techniques. Cureus. https://doi.org/10.7759/cureus.6483
Spitler CA, Bergin PF, Russell GV, Graves ML (2018) Endosteal substitution with an intramedullary rod in fractures of the femur. J Orthop Trauma 32(1):S25–S29. https://doi.org/10.1097/BOT.0000000000001094
Bergin PF, Weber TG, Gerow DE, Spitler CA, Graves ML, Russell GV (2018) Intraosseous plating for the management of cortical defects. J Orthop Trauma 32(1):S12–S17. https://doi.org/10.1097/BOT.0000000000001095
Mast J, Jakob R, Ganz R (1989) Planning and reduction technique in fracture surgery. Springer, Berlin. https://doi.org/10.1007/978-3-642-61306-7
Ganz R, Isler B, Mast J (1984) Internal fixation technique in pathological fractures of the extremities. Arch Orthop Trauma Surg 103(2):73–80. https://doi.org/10.1007/BF00389575
Park KH, Oh CW, Park IH, Kim JW, Lee JH, Kim HJ (2019) Additional fixation of medial plate over the unstable lateral locked plating of distal femur fractures: a biomechanical study. Injury 50(10):1593–1598. https://doi.org/10.1016/j.injury.2019.06.032
Prayson MJ, Datta DK, Marshall MP (2001) Mechanical comparison of endosteal substitution and lateral plate fixation in supracondylar fractures of the femur. J Orthop Trauma 15(2):96–100. https://doi.org/10.1097/00005131-200102000-00004
Matelic TM, Monroe MT, Mast JW (1996) The use of endosteal substitution in the treatment of recalcitrant nonunions of the femur: report of seven cases. J Orthop Trauma 10(1):1–6. https://doi.org/10.1097/00005131-199601000-00001
Zura R, Mehta S, Della Rocca GJ, Steen RG (2016) Biological risk factors for nonunion of bone fracture. JBJS Rev. https://doi.org/10.2106/JBJS.RVW.O.00008
Pearson RG, Clement RGE, Edwards KL, Scammell BE (2016) Do smokers have greater risk of delayed and non-union after fracture, osteotomy and arthrodesis? A systematic review with meta-analysis. BMJ Open 6(11):e010303. https://doi.org/10.1136/bmjopen-2015-010303
Tank JC, Schneider PS, Davis E et al (2016) Early mechanical failures of the synthes variable angle locking distal femur plate. J Orthop Trauma 30(1):e7–e11. https://doi.org/10.1097/BOT.0000000000000391
Cole PA (2003) Endosteal allograft plating for the treatment of recalcitrant nonunions. Tech Orthop 18(4):344–355. https://doi.org/10.1097/00013611-200312000-00008
Saridis A, Panagiotopoulos E, Tyllianakis M, Matzaroglou C, Vandoros N, Lambiris E (2006) The use of the Ilizarov method as a salvage procedure in infected nonunion of the distal femur with bone loss. J Bone Joint Surg Br 88:232–237. https://doi.org/10.1302/0301-620X.88B2.16976
Haidukewych GJ, Springer BD, Jacofsky DJ, Berry DJ (2005) Total knee arthroplasty for salvage of failed internal fixation or nonunion of the distal femur. J Arthroplasty 20(3):344–349. https://doi.org/10.1016/j.arth.2004.03.026
Cavusoglu AT, Ozsoy MH, Dincel VE, Sakaogullari A, Basarir K, Ugurlu M (2009) The use of a low-profile Ilizarov external fixator in the treatment of complex fractures and non-unions of the distal femur. Acta Orthop Belg 75(2):209–218
Marsh DR, Shah S, Elliott J, Kurdy N (1997) The Ilizarov method in nonunion malunion and infection of fractures. J Bone Joint Surg Br 79:273–279. https://doi.org/10.1302/0301-620X.79B2.0790273
Davila J, Malkani A, Paiso JM (2001) supracondylar distal femoral nonunions treated with a megaprosthesis in elderly patients: a report of two cases. J Orthop Trauma 15(8):574–578. https://doi.org/10.1097/00005131-200111000-00009
Springer BD, Hanssen AD, Sim FH, Lewallen DG (2001) The kinematic rotating hinge prosthesis for complex knee arthroplasty. Clin Orthop 392:283–291. https://doi.org/10.1097/00003086-200111000-00037
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Oransky, M., Galante, C., Cattaneo, S. et al. Endosteal plating for the treatment of malunions and nonunions of distal femur fractures. Eur J Orthop Surg Traumatol 33, 2243–2251 (2023). https://doi.org/10.1007/s00590-022-03458-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-022-03458-x