Abstract
Purpose
Compare the outcomes of randomized clinical trials of cervical disc arthroplasty (CDA) versus anterior cervical discectomy with fusion (ACDF), with a minimum follow-up of 7 years.
Methods
Nine randomized clinical trials were selected. The clinical, radiological, and surgical outcomes were analyzed, including functional and pain scores, range of motion, adjacent segment degeneration, adverse events, and need for reoperation.
Results
2664 patients were included in the study. Pooled results indicated that the CDA group had a significantly higher overall success rate (p < 0.001), a higher improvement in the neck disability index (NDI) (p = 0.002), less VAS arm pain (p = 0.01), and better health questionnaire SF-36 physical component (p = 0.01) than ACDF group. Likewise, the pooled results indicated a significantly higher motion rate (p < 0.001), less adjacent syndrome (p < 0.05), and a lower percentage of reoperation (p < 0.001) in the CDA group. There were no significant differences between the CDA and ACDF groups in the neck pain scale (p = 0.11), the health questionnaire SF-36 mental component (p = 0.10), and in adverse events (p = 0.42).
Conclusion
In long-term follow-up, CDA showed a better overall success rate, better improvement in NDI, less VAS arm pain, better health questionnaire SF-36 physical component, a higher motion rate, less adjacent syndrome, and less reoperation rate than ACDF. No significant differences were found in the neck pain scale, SF-36 mental component, and in adverse events.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cervical disc disease (CDD) is an illness entailing degenerated and protruded discs of the cervical spine, causing neck pain, with or without radicular pain in arms, myelopathy, and alteration of the overall cervical spine biomechanics [1, 2]. Symptomatic CDD is considered one of the main causes of incapacity for work [1]. Published studies indicate an increase in the trend of cervical surgery in the coming years, above all, in the population between 45 and 54 years old [2, 3].
Since Robinson and Smith first reported in 1958, anterior cervical discectomy with fusion (ACDF) has been widely used for treating CDD, including cervical disc herniation (CDH), and has been classically the gold standard procedure. In this technique, anterior direct decompression and physical sagittal alignment restore are performed with the use of a cage inserted into the intervertebral space [4]. Many studies have found ACDF to be a successful procedure; and is reported to provide excellent symptom relief and significant improvement in quality of life [5,6,7] For this reason, it has been reported that 84.3% of orthopedic surgeons performed ACDF as the standard technique for CDD and CDH [6]. However, ACDF has also presented some well-characterized complications like pseudoarthrosis or nonunion, instrumentation failure, and the most problematic, causing patients to undergo secondary surgery: a solid bony fusion in this procedure can change the range of motion (ROM) and the mechanical load of adjacent segments, which can cause subsequent adjacent segment disease (ASD) [8, 9]. Hilibrand et al., found that symptomatic adjacent segment disease may affect more than a quarter of all patients within ten years after an ACDF [10]. Lee et al., found that after ACDF, secondary surgery in adjacent segments occurred at a relatively constant rate of 2.4% per year (95% confidence interval (CI), 1.9–3.0). Kaplan–Meier analysis predicted that 22.2% of patients would require reintervention in adjacent segments at 10 years postoperatively [11].
To avoid these risks, an alternative treatment, cervical disc arthroplasty (CDA), emerged in 1990’s, with the introduction of a mobile division between the vertebrae [12]. The CDA has the advantage of preserving physiological motion, maintaining the disc height and segmental lordosis, and the biomechanical properties of the cervical spine. It can also prevent the need for future reoperations [13,14,15]. Based on these advantages the use of CDA has increased, in the last years [3]. However, CDA also presents some drawbacks, the most common being heterotopic ossification, implant failure, and bone loss [16, 17]. Several previous meta-analyses have compared the advantages and disadvantages of ACDF and CDA with inconclusive results, mostly related to short-term follow-up (2 years of follow-up) [7, 14,15,16, 18,19,20,21], with few studies analyzing the mid-term efficacy (5 years of follow-up) [22]. With the hypothesis that differences can be seen at long-term follow-up, the purpose of this meta-analysis was to examine the long-term efficacy between ACDF and CDA by comparing clinical, radiological, and surgical outcomes, in randomized clinical trials with a minimum follow-up of 7 years.
Material and methods
Literature search strategy
The present meta-analysis was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement [23] and the systematic review following the Cochrane Handbook for Systematic Reviews of Interventions recommendations [24]. An electronic search was performed on PubMed, EMBASE, and Cochrane Collaboration Library up to 30 November 2020, for randomized trials of ACDF versus CDA. The following keywords were used in the search strategy: ¨anterior cervical discectomy and fusion¨ or ¨ACDF¨, and ¨cervical disc arthroplasty¨ or ¨CDA¨, and ¨randomized controlled trial¨. The bibliographic search was restricted to the English language.
Eligibility criteria
Inclusion criteria for study identification were as follows: (1) randomized controlled trials (RCTs), (2) comparison between two surgical procedures (CDA and ACDF), (3) follow-up time of more than 84 months, (4) reporting at least one surgery-related outcome and (5) full-text reports in English. Those studies with (1) lack of comparative data, (2) insufficient follow-up, (3) biomechanical or in vitro studies, and (4) conference presentations, editorials, and abstracts were excluded from the meta-analysis.
Study selection
Two authors assessed the search results for eligibility. Intensive reading of the full text was performed when the studies met the inclusion criteria. If there was a conflict between the two reviewers, a third reviewer was consulted to reach a decision.
Data extraction
Data were extracted from the main texts and supplementary appendices of the trials. The data extracted from the enrolled studies were performed as follows: (I) General characteristics such as first author, year of publication, number of clinical trial (NCT), enrolled patients, age, sex, surgical levels, type of prosthesis, and follow-up duration were extracted. (II) Clinical outcome measures, including clinical overall success rate, neck disability index (NDI), neck pain, arm radicular pain, 36-item Short Form (SF-36) Health Survey (summary of physical and mental components). (III) Radiological outcome measures, include fusion rate, heterotopic ossification rate, range of motion (ROM), superior adjacent syndrome, and inferior adjacent syndrome. (IV) Surgical outcome measures, such as adverse events rate and reoperation rate.
Quality assessment
RCTs quality was assessed according to Review Manager (RevMan) version 5.3 software (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, 2014) to assess the risk of bias. Assessment methods consisted of the following steps: random sequence generation, allocation concealment, blinding, incomplete outcome data, and selective outcome reporting. Scores in these domains are distilled into an overall assessment of the overall risk of bias for a given RCT: (I) “low risk of bias”; (II) “some concerns”; or (III) “high risk of bias”.
Statistical analysis
Descriptive statistics were mean and standard deviation (SD) for continuous variables and count and percentage for categorical variables. Meta-analysis was performed using Review Manager software (Version 5.3) from the Cochrane community. For binary variables, the odds ratio (OR) was used for evaluation, while for continuous variables, the standard mean difference (SMD) with a 95% confidence interval (CI) was applied. The heterogeneity of the studies was estimated using the I2 test. The random-effects inverse variance model was applied. Statistical significance was defined as a two-tailed p-value of < 0.05.
Results
Literature review
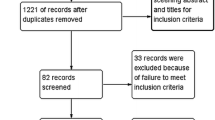
The initial database search identified 2834 articles (PubMed: 1452, Embase: 1020, Cochrane Collaboration Library: 362) and the detailed literature selection is described in the flowchart in Fig. 1. A total of 1231 studies were removed because they were duplicates, 1553 studies were excluded based on their titles and abstracts, and 41 studies were excluded for other reasons. As a result, 9 studies were included for further evaluation [25,26,27,28,29,30,31,32,33]. Figure 2 provides the summary of the risk of bias.
Study characteristics
The general characteristics of each study are shown in Table 1. The meta-analysis included a total of 2664 patients, with 1464 patients undergoing CDA while 1200 underwent ACDF [25,26,27,28,29,30,31,32,33]. The mean age was 44.2 (SD 1.8) in CDA and 44.8 (SD 1.6) in ACDF, there were no statistically significant differences (SMD = − 0.08, 95% CI: − 0.18–0.02, p = 0.12) [26, 28,29,30, 33]. There were 674 men and 746 women in the CDA group, and 552 men and 601 women in the ACDF group, there were no statistically significant differences (OR = 1.02, 95% CI: 0.87–1.19, p = 0.85) [25, 26, 28,29,30, 32, 33]. Eight studies compared CDA and ACDF at one level replacement [25,26,27, 29,30,31,32,33]; and two studies compared at 2 levels replacement [28, 30]. Three studies used the BRYAN® Cervical Disc (Medtronic, Minneapolis, MN) [29, 31, 32]; 2 studies used Prestige® Cervical Disc (Medtronic, Minneapolis, MN) [25, 28], 2 studies used ProDisc-C® (Depuy-Synthes Spine, Raynham, MA) [26, 27], 1 study used Mobi-C® Cervical Disc (Zimmer Biomet, Warsaw, IN) [30], and one study used SECURE-C (Globus Medical, Audubon, Pennsylvania) Cervical Disc [33]
Clinical outcomes
The CDA group had a significantly higher overall success rate (p < 0.001), a higher improvement in the neck disability index (NDI) (p = 0.002), less VAS arm pain (p = 0.01), and better health questionnaire SF-36 physical component (p = 0.01) than ACDF group. There were no significant differences between the CDA and ACDF groups in the neck pain scale (p = 0.11), and the health questionnaire SF-36 mental component (p = 0.10).
The overall success rate was reported in 6 studies that included 1370 patients in the CDA group and 1106 patients in the ACDF group [25, 26, 28, 30, 32, 33]. Pooled results showed that the overall success rate in the CDA group was significantly higher than in the ACDF group (OR = 1.98, 95% CI: 1.57–2.49, p < 0.001) with moderate heterogeneity (I2 = 36%, p = 0.16) (Fig. 3a). The NDI, data were provided in 4 studies that included 790 patients in the CDA group and 579 patients in the ACDF group [25,26,27, 30]. Significant differences in the NDI in favor of CDA were found (SMD = − 0.21, 95% CI: − 0.38 to − 0.04, p = 0.02), with substantial heterogeneity (I2 = 51%, p = 0.08) (Fig. 3b).
a Forest plot of overall success rate. b Forest plot of neck disability index (NDI). c Forest plot of VAS neck pain. d Forest plot of VAS arm pain. e Forest plot of SF-36 physical component. f Forest plot of SF-36 mental component. 95% CI: indicates 95% confidence interval; ACDF: anterior cervical discectomy and fusion; CDA: cervical disc arthroplasty; Std: standard; OR, odds ratio
Neck pain and arm pain scales were found to be analyzed in the same 5 studies, with 941 patients in the CDA group and 719 patients in the ACDF group [25,26,27, 30, 33]. Pooled results showed no significant differences in the neck pain scale between the 2 groups (SMD = − 0.17, 95% CI: − 0.37–0.04, p = 0.11) with high heterogeneity (I2 = 74%, p = 0.002) (Fig. 3c). Pooled results showed that the arm pain scale was significantly in favor in the CDA group (SMD = − 0.16, 95% CI: − 0.29 to − 0.04, p = 0.01) with moderate heterogeneity (I2 = 31%, p = 0.20) (Fig. 3d). Regarding the 36-item Short Form health questionnaire (SF-36) (physical and mental components), 4 studies included the analysis of the physical component [25, 26, 30, 33], and 3 studies included the analysis of the mental component [26, 30, 33], with a total of 919 patients in the CDA group and 697 in the ACDF group for the former, and 643 and 432 respectively for the latter. Pooled results showed that the physical SF-36 component was significantly in favor in the CDA group (SMD = 0.13 95% CI: 0.03–0.23, p = 0.01) with very low heterogeneity (I2 = 1%, p = 0.40) (Fig. 3e). No significant differences were found between the 2 groups in the mental SF-36 component (SMD = 0.19, 95% CI: − 0.03–0.41, p = 0.10), with substantial heterogeneity (I2 = 69%, p = 0.02) (Fig. 3f).
Radiological outcomes
A heterotopic ossification rate of 10.3% was observed in the CDA group. A fusion rate of 94.06% was found in the ACDF group. The pooled results indicated a significantly higher motion rate (p < 0.001), and less adjacent syndrome (p < 0.05), in the CDA group. The motion rate with SD was reported in 2 studies that included 267 patients in the CDA group and 187 patients in the ACDF group [26, 30]. Pooled results showed that the motion rate in the CDA group was significantly higher (SMD = 1.86, 95% CI: 1.63–2.08, p < 0.001) with inconspicuous heterogeneity (I2 = 0%, p = 0.52) (Fig. 4a). Pooled rates of the superior adjacent syndrome were reported in 4 studies (with a total of 832 patients in the CDA group and 594 in the ACDF group) [29, 30, 32, 33]. Less superior adjacent syndrome was reported in the CDA group (OR = 0.33, 95% CI: 0.17–0.65, p = 0.001), with substantial heterogeneity (I2 = 81%, p < 0.001) (Fig. 4b). Only one study reported the rate of the inferior adjacent syndrome [30]. Less inferior adjacent syndrome was reported in the CDA group (OR = 0.31, 95% CI: 0.15–0.66, p = 0.002), with substantial heterogeneity (I2 = 75.1%, p = 0.05) (Fig. 4c).
Surgical outcomes
The pooled results indicated no significant differences in adverse events (p = 0.42) between both groups and a significantly lower percentage of reoperation (p < 0.001) in the CDA group. Adverse events were reported in 7 studies that included 1420 patients in the CDA group and 11,153 patients in the ACDF group [25, 26, 28,29,30, 32, 33]. There was no difference in the rate of adverse events between CDA (33.1%) and ACDF (38.9%) (OR = 0.84, 95% CI: 0.56–1.27, p = 0.42), with moderate heterogeneity (I2 = 37%, p = 0.13). For reoperation rate, 7 studies documented it, with 1172 patients in the CDA group and 932 in the ACDF group. [25,26,27,28, 30, 31, 33]. Reoperations occurred in 4.4% of CDA patients, a significantly lower rate compared with 15.6% of the ACDF group (OR = 0.26, 95% CI: 0.19–0.37, p < 0.001), with inconspicuous heterogeneity (I2 = 0.0%, p = 0.97). Figure 5 summarizes the adverse events and the reoperation rate.
Discussion
Numerous meta-analyses in recent years have compared the clinical and radiological results of ACDF and CDA, trying to find the advantages and disadvantages of each, most of them have inconclusive results and are related to short or medium-term follow-ups [7, 14,15,16, 18,19,20,21,22]. In this meta-analysis, we aimed to compare both treatments (CDA and ACDF) for CDD at long-term follow-up. Our main findings were that with a minimum follow-up of 7 years, CDA showed a statistically better overall success rate, better improvement in NDI, less VAS arm pain, better SF-36 physical component, better motion rate, less adjacent syndrome, and less reoperation than ACDF. No significant differences were found in adverse events, neck pain scale, or mental SF-36 component.
Some limitations of the present study should be taken into account. First, the number of included studies was small, which may lead to insufficient evidence. However, only RCT was included, which is stronger. Second, as all RCT, there are inclusion and exclusion criteria, for that reason the patients analyzed were able to have either CDA or ACDF. However, patients suitable for ACDF but not for CDA were excluded. Third some results have moderate heterogeneity, which can introduce bias. And fourth, although the ACDF and CDA groups suffered from CDD, the intervention of the two groups was not the same. Some studies were surgery at one level and others at two levels. In addition, the ACDF group selection fusion tools are also different: interbody graft with bone graft (autograft vs. allograft) or implants. On the other hand, the ADC groups used different types of artificial intervertebral discs, including Mobi-C, Bryan, Prestige, SECURE-C, and Prodisc-C. Different interventions can affect the accuracy of the conclusion. Further high-quality, large-sample studies with strong evidence are needed to verify our results.
In the terms of age (p = 0.12) and sex (p = 0.85) no statistically significant differences were found between both groups. This is important because can limit demographic bias. Study selection and study homogeneity play an important role in quality control when performing a meta-analysis. RCTs can optimize follow-up and data quality, with low selection bias and confounding [34]. For example, Saifi et al., after a retrospective analysis of a national database, found that CDA's review burden was more than double that of ACDF's review burden (5.9% vs 2.3%), which was not taken into account in the initial patient demographics [3]. Regarding clinical outcomes, no significant differences were found between CDA and ACDF for neck pain and the SF-36 mental component. In contrast, NDI, radicular pain, and SF-36 physical component were reported significantly better in the CDA group, as well as the surgical overall success. These findings are similar to some meta-analyses [14, 15, 18], however, they also differ from other meta-analyses, like Luo et al. [21], and Gao et al. [7], they found lower cervical and arm pain scores in the CDA group than in the ACDF group (p < 0.05); and similar NDI in both groups (p > 0.05). Gendreu et al., in their meta-analysis, they did not find statistically significant difference between NDI (p = 0.37), VAS neck pain (p = 0.79), neither VAS arm pain (p = 0.66) [35]. Zhang et al., found that in short-term and midterm follow-up, patients treated with CDA had improved NDI and had higher NDI success rates than those treated with ACDF. Regarding pain relief, they found CDA group had lower neck pain scores and lower arm pain scores in short-term follow-up and in midterm follow-up. Furthermore, they found higher overall success rates in the CDA group [15]. This discrepancy in the results may be due to the heterogeneity of the groups [7, 14,15,16, 18, 21, 35]. The result may indicate, as Zhang et al. said, that different types of cervical arthroplasties might have different efficacy [15]. Due to the limited number of included articles, subgroup analyses stratified by prosthesis types cannot be performed for the other outcomes. However, taking into account all these data, this may indicate that both techniques may be useful for improving pain management and improving quality-of-life health.
A significantly higher motion rate and less adjacent syndrome in the CDA group were found in our study. The higher range of motion is a constant finding in other metanalyses, which means that the CDA movement persists despite time [7, 15, 16, 18, 20,21,22, 36]. Regarding adjacent syndrome, Zhu Y et al., in a meta-analysis of 14 RCTs showed that there were significantly fewer adjacent segment reoperations in the CDA groups (hazard ratio 0.47) compared with the ACDF groups with a follow-up of 2 to 7 years [20]. Luo et al. found that CDA had a significantly lower incidence of AS (OR = 0.57, 95% CI: 0.44–0.73, p < 0.00001) with no obvious heterogeneity (I2 = 17%, p = 0.26) [37]. Dong et al., also found that the rate of adjacent segment in the CDA group was significantly lower compared with ACDF (p < 0.01), and that the advantage of CDA in reducing adjacent segment reoperation increase with increasing of follow-up time (p < 0. 01) [36]. Xu et al., also found a decrease in the rates of adjacent segment degeneration and reoperation in CDA compared with ACDF, and the superiority may become more apparent over time [38]. AS rates were significantly lower in the CDA group than in the ACDF group, which altogether may suggest that CDA reduces or prevents adjacent syndrome [7, 18, 20,21,22, 36,37,38]. Although, the assumption that adjacent segment disease arises from ACDF with iatrogenic motion restriction is currently under debate. Some investigators have hypothesized that adjacent segment disease signifies natural history progression of spinal segmental degeneration [39].
No significant differences were found in adverse events, however CDA have less reoperation rate than ACDF. When talking about adverse events, no significant difference was found in adverse events between CDA and ACDF (OR = 0.84, 95% CI: 0.56–1.27, p = 0.42), results that are consistent with previous studies [22, 40]. In our meta-analysis reoperations occurred in 4.4% of CDA patients, a significantly lower rate compared to 15.6% in the ACDF group (OR = 0.26, 95% CI: 0.19–0.37, p < 0.001). This finding is similar to other randomized clinical trials or meta-analyses [7, 18,19,20, 22, 35, 37, 41]. Zhu R et al. [41] and Zhang et al. [22], in their respective meta-analysis showed that the rate of index-level secondary surgery in the CDA group was significantly lower than in the ACDF group (RR, 0.47; 95%CI, 0.36–0.63; p < 0.05) and (OR = 0.41, 95% CI: 0.25–0.69, p = 0.001), respectively. Also, Luo et al., found a lower incidence of reoperations (OR = 0.43, 95% CI 0.29 to 0.64, p < 0.0001). Xu et al. and Dong et al., also found a decrease in the rates of reoperation in CDA compared with ACDF, and the superiority may become more apparent over time [36, 38]. Despite, reoperation rates were significantly lower in the CDA group than in the ACDF group in most studies [7, 18,19,20, 22, 35,36,37,38, 41], some meta-analyses have not found a statistically significant differences [4].
In conclusion, for the treatment of CDD, in patients suitable for ACDF or CDA, CDA is superior to ACDF in terms of a better overall success rate, better improvement in NDI, less VAS arm pain, better health questionnaire SF-36 physical component, a higher motion rate, less adjacent syndrome, and less reoperation rate. No significant differences were found in the neck pain scale, SF-36 mental component, and in adverse events between both treatments.
References
Hoy D, March L, Woolf A, Blyth F, Brooks P, Smith E, Vos T, Barendregt J, Blore J, Murray C, Burstein R, Buchbinder R (2014) The global burden of neck pain: estimates from the global burden of disease 2010 study. Ann Rheum Dis 73:1309–1315. https://doi.org/10.1136/annrheumdis-2013-204431
Neifert SN, Martini ML, Yuk F, McNeill IT, Caridi JM, Steinberger J, Oermann EK (2020) Predicting trends in cervical spinal surgery in the United States from 2020 to 2040. World Neurosurg 141:e175–e181. https://doi.org/10.1016/j.wneu.2020.05.055
Saifi C, Fein AW, Cazzulino A, Lehman RA, Phillips FM, An HS, Riew KD (2018) Trends in resource utilization and rate of cervical disc arthroplasty and anterior cervical discectomy and fusion throughout the United States from 2006 to 2013. Spine J 18:1022–1029. https://doi.org/10.1016/j.spinee.2017.10.072
Zhang D, Liu B, Zhu J, Li C, Wei F, Yuan Y, Zhu D (2019) Comparison of clinical and radiologic outcomes between self-locking stand-alone cage and cage with anterior plate for multilevel anterior cervical discectomy and fusion: a meta-analysis. World Neurosurg 125:e117–e131. https://doi.org/10.1016/j.wneu.2018.12.218
Buttermann GR (2018) Anterior cervical discectomy and fusion outcomes over 10 Years: a prospective study. Spine 43:207–214. https://doi.org/10.1097/BRS.0000000000002273
Chin-See-Chong TC, Gadjradj PS, Boelen RJ, Harhangi BS (2017) Current practice of cervical disc arthroplasty: a survey among 383 AO spine International members. Neurosurg Focus 42:1–9. https://doi.org/10.3171/2016.11.FOCUS16338
Gao F, Mao T, Sun W, Guo W, Wang Y, Li Z, Abhinav P (2015) An updated meta-analysis comparing artificial cervical disc arthroplasty (CDA) versus anterior cervical discectomy and fusion (ACDF) for the treatment of cervical degenerative disc disease (CDDD). Spine 40(23):1816–1823. https://doi.org/10.1097/BRS.0000000000001138
Eck JC, Craig Humphreys S, Lim TH, Jeong ST, Kim JG, Hodges SD, An HS (2002) Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine 27(22):2431–2434. https://doi.org/10.1097/00007632-200211150-00003
Park DH, Ramakrishnan P, Cho TH, Lorenz E, Eck JC, Humphreys SC, Lim TH (2007) Effect of lower two-level anterior cervical fusion on the superior adjacent level. J Neurosurg Spine 7:336–340. https://doi.org/10.3171/SPI-07/09/336
Hilibrand AS, Carlson GD, Palumbo MA et al (1999) Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am 81:519–528. https://doi.org/10.2106/00004623-199904000-00009
Lee JC, Lee SH, Colleen Peters K, Riew D (2015) Adjacent segment pathology requiring reoperation after anterior cervical arthrodesis: the influence of smoking, sex, and number of operated levels. Spine 40(10):E571–E577. https://doi.org/10.1097/BRS.0000000000000846
Chang CC, Huang WC, Jau-Ching W, Mummaneni PV (2018) The Option of motion preservation in cervical spondylosis: cervical disc arthroplasty update. Neurospine 15(4):296–305. https://doi.org/10.14245/ns.1836186.093
Duggal N, Pickett GE, Mitsis DK, Keller JL (2004) Early clinical and biomechanical results following cervical arthroplasty. Neurosurg Focus 17:62–68. https://doi.org/10.3171/foc.2004.17.3.9
Zhao H, Duan LJ, Gao YS, Yang YD, Tang XS, Zhao DY, Xiong Y, Hu ZG, Li CH, Yu X (2018) What is the superior surgical strategy for bi-level cervical spondylosis-anterior cervical disc replacement or anterior cervical decompression and fusion? Medicine 97:1–11. https://doi.org/10.1097/MD.0000000000010005
Zhang Y, Liang C, Tao Y, Zhou X, Li H, Li F, Chen Q (2015) Cervical total disc replacement is superior to anterior cervical decompression and fusion: A meta-analysis of prospective randomized controlled trials. PLoS ONE 10:1–18. https://doi.org/10.1371/journal.pone.0117826
Shangguan L, Ning GZ, Tang Y, Wang Z, Luo ZJ, Zhou Y (2017) Discover cervical disc arthroplasty versus anterior cervical discectomy and fusion in symptomatic cervical disc diseases: a metaanalysis. PLoS ONE 12:1–15. https://doi.org/10.1371/journal.pone.0174822
Kim JS, Dowdell J, Cheung ZB, Arvind V, Sun L, Jandhyala C, Ukogu C, Ranson W, Jacobs S, McAnany S, Cho SK (2018) The seven-year cost-effectiveness of anterior cervical discectomy and fusion versus cervical disc arthroplasty: a Markov analysis. Spine 43:1543–1551. https://doi.org/10.1097/BRS.0000000000002665
Zou S, Gao J, Xu B, Lu X, Han Y, Meng H (2017) Anterior cervical discectomy and fusion (ACDF) versus cervical disc arthroplasty (CDA) for two contiguous levels cervical disc degenerative disease: a meta-analysis of randomized controlled trials. Eur Spine J 26:985–997. https://doi.org/10.1007/s00586-016-4655-5
Zhong ZM, Zhu SY, Zhuang JS, Wu Q, Chen JT (2016) Reoperation after cervical disc arthroplasty versus anterior cervical discectomy and fusion: a meta-analysis. Clin Orthop Relat Res 474:1307–1316. https://doi.org/10.1007/s11999-016-4707-5
Zhu Y, Zhang B, Liu H, Yuntao W, Zhu Q (2016) Cervical disc arthroplasty versus anterior cervical discectomy and fusion for incidence of symptomatic adjacent segment disease: a meta-analysis of prospective randomized controlled trials. Spine 41(19):1493–1502. https://doi.org/10.1097/BRS.0000000000001537
Luo J, Huang S, Gong M, Dai X, Gao M, Yu T, Zhou Z, Zou X (2015) Comparison of artificial cervical arthroplasty versus anterior cervical discectomy and fusion for one-level cervical degenerative disc disease: a meta-analysis of randomized controlled trials. Eur J Orthop Surg Traumatol 25:115–125. https://doi.org/10.1007/s00590-014-1510-4
Zhang Y, Lv N, He F, Pi B, Liu H, Chen AC, Yang H, Liu M, Zhu X (2020) Comparison of cervical disc arthroplasty and anterior cervical discectomy and fusion for the treatment of cervical disc degenerative diseases on the basis of more than 60 months of follow-up: a systematic review and meta-analysis. BMC Neurol 20:1–12. https://doi.org/10.1186/s12883-020-01717-0
Page MJ, Moher D (2017) Evaluations of the uptake and impact of the preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement and extensions: a scoping review. Syst Rev 6:1–14. https://doi.org/10.1186/s13643-017-0663-8
Cumpston M, Li T, Page MJ, Chandler J, Welch VA, Higgins JP, Thomas J (2019) Updated guidance for trusted systematic reviews: a new edition of the Cochrane handbook for systematic reviews of interventions. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.ED000142
Burkus JK, Traynelis VC, Haid RW, Mummaneni PV (2014) Clinical and radiographic analysis of an artificial cervical disc: 7-year follow-up from the Prestige prospective randomized controlled clinical trial. J Neurosurg Spine 21:516–528. https://doi.org/10.3171/2014.6.SPINE13996
Janssen ME, Zigler JE, Spivak JM, Delamarter RB, Darden BV 2nd, Kopjar B (2015) ProDisc-C total disc replacement versus anterior cervical discectomy and fusion for single-level symptomatic cervical disc disease: seven-year follow-up of the prospective randomized U.S. food and drug administration investigational device exemption study. J Bone Joint Surg Am 97:1738–1747. https://doi.org/10.2106/JBJS.N.01186
Loumeau TP, Darden BV, Kesman TJ, Odum SM, Van Doren BA, Laxer EB, Murrey DB (2016) A RCT comparing 7-year clinical outcomes of one level symptomatic cervical disc disease (SCDD) following ProDisc-C total disc arthroplasty (TDA) versus anterior cervical discectomy and fusion (ACDF). Eur Spine J 25:2263–2270. https://doi.org/10.1007/s00586-016-4431-6
Lanman TH, Burkus JK, Dryer RG, Gornet MF, McConnell J, Hodges SD (2017) Long-term clinical and radiographic outcomes of the prestige LP artificial cervical disc replacement at 2 levels: results from a prospective randomized controlled clinical trial. J Neurosurg Spine 27:7–19. https://doi.org/10.3171/2016.11.SPINE16746
Donk RD, Verbeek ALM, Verhagen WIM, Groenewoud H, Hosman AJF, Bartels RHMA (2017) What’s the best surgical treatment for patients with cervical radiculopathy due to single-level degenerative disease? A randomized controlled trial. PLoS ONE 12:1–17. https://doi.org/10.1371/journal.pone.0183603
Radcliff K, Davis RJ, Hisey MS, Nunley PD, Hoffman GA, Jackson RJ, Bae HW, Albert T, Coric D (2017) Long-term evaluation of cervical disc arthroplasty with the Mobi-C© cervical disc: a randomized, prospective, multicenter clinical trial with seven-year follow-up. Int J Spine Surg 11(4):31. https://doi.org/10.14444/4031
Sasso WR, Smucker JD, Sasso MP, Sasso RC (2017) Long-term clinical outcomes of cervical disc arthroplasty: a prospective, randomized, controlled trial. Spine 42(4):209–216. https://doi.org/10.1097/BRS.0000000000001746
Lavelle WF, Daniel Riew K, Levi AD, Florman JE (2019) Ten-year outcomes of cervical disc replacement with the BRYAN Cervical disc: results from a prospective, randomized, controlled clinical trial. Spine 44(9):601–608. https://doi.org/10.1097/BRS.0000000000002907
Vaccaro A, Beutler W, Peppelman W, Marzluff J, Mugglin A, Ramakrishnan PS, Myer J, Baker KJ (2018) Long-term clinical experience with selectively constrained SECURE-C cervical artificial disc for 1-level cervical disc disease: results from seven-year follow-up of a prospective, randomized, controlled investigational device exemption clinical trial. Int J Spine Surg 12(3):377–387
Kocher MS, Zurakowski D (2004) Clinical epidemiology and biostatistics: a primer for orthopaedic surgeons. J Bone Joint Surg Am 86:607–620
Gendreau JL, Kim LH, Prins PN, D’Souza M, Rezaii P, Pendharkar AV, Sussman ES, Ho AL, Desai AM (2020) Outcomes after cervical disc arthroplasty versus stand-alone anterior cervical discectomy and fusion: a meta-analysis. Glob Spine J 10:1046–1056. https://doi.org/10.1177/2192568219888448
Dong L, Xu Z, Chen X, Wang D, Li D, Liu T, Hao D (2017) The change of adjacent segment after cervical disc arthroplasty compared with anterior cervical discectomy and fusion: a meta-analysis of randomized controlled trials. Spine J 17:1549–1558. https://doi.org/10.1016/j.spinee.2017.06.010
Luo J, Wang H, Peng J, Deng Z, Zhang Z, Liu S, Wang D, Gong M, Tang S (2018) Rate of adjacent segment degeneration of cervical disc arthroplasty versus fusion meta-analysis of randomized controlled trials. World Neurosurg 113:225–231. https://doi.org/10.1016/j.wneu.2018.02.113
Shuai X, Liang Y, Zhu Z, Qian Y, Liu H (2018) Adjacent segment degeneration or disease after cervical total disc replacement: a meta-analysis of randomized controlled trials. J Orthopaed Surg Res. https://doi.org/10.1186/s13018-018-0940-9
Pesce A, Wierzbicki V, Piccione E, Frati A, Raco A, Caruso R (2017) Adjacent segment pathology: natural history or effect of anterior cervical discectomy and fusion? A 10-year follow-up radiological multicenter study using an evaluation scale of the ageing spine. Eur J Orthop Surg Traumatol 27:503–511. https://doi.org/10.1007/s00590-017-1936-6
Zhao G-S, Zhang Q, Quan Z-X (2017) Mid-term efficacy and safety of cervical disc arthroplasty versus fusion in cervical spondylosis: A systematic review and meta-analysis. Biomed Rep 6:159–166. https://doi.org/10.3892/br.2016.823
Zhu RS, Kan SL, Cao ZG, Jiang ZH, Zhang XL, Hu W (2018) Secondary surgery after cervical disc arthroplasty versus fusion for cervical degenerative disc disease: a meta-analysis with trial sequential analysis. Orthop Surg 10:181–191. https://doi.org/10.1111/os.12401
Acknowledgements
We want to express our gratitude to the MBA Institute for their help and methodological support in the realization of this study.
Funding
No funds were received in support of this work. No relevant financial activities outside the submitted work.
Author information
Authors and Affiliations
Contributions
JH Nuñez, JMP, BE and FAG. wrote the main manuscript text and JHN and FAG and MS prepared figures. BE, JMP, MS and DB prepared tables. All authors reviewed the manuscript. The manuscript has been read and approved by all the authors, the requirements for authorship have been met, and all authors believes that the manuscript represents honest work.
Corresponding author
Ethics declarations
Conflict of interest
No, I declare that the authors have no competing interests that might be perceived to influence the results and/or discussion reported in this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Núñez, J.H., Escudero, B., Omiste, I. et al. Outcomes of cervical arthroplasty versus anterior cervical arthrodesis: a systematic review and meta-analysis of randomized clinical trials with a minimum follow-up of 7-year. Eur J Orthop Surg Traumatol 33, 1875–1884 (2023). https://doi.org/10.1007/s00590-022-03365-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-022-03365-1