Abstract
Objective
Pediatric proximal femur fracture is extremely rare trauma comparing to other fractures. The proximal femur fracture is 1% of all pediatric fractures. The aim of current study is to compare the incidence of early complications and outcomes of pediatric proximal femur fractures regarding fracture types retrospectively.
Design
Our study includes 35 cases which are criticized by Delbet classification system, modalities of treatment, duration of waiting for surgery, duration of follow-up and also complications. Our inclusion criteria are age below 16 years old, proximal femur fractures with no evidence of tumoral, romathologic and methabolic conditions. Age, sex and surgery type (open-closed) were noted, and the data were statistically assessed. Assessment of the final outcome was made at the last follow-up visit using the Ratliff’s method.
Results
The mean of age of patients in our study is 9.5 ± 5.06 years. The average follow-up was 25.6 ± 13.2 months. 15 patients (42.9%) are type 2 Delbet fracture, 5 patients (14.2%) are Delbet type 3 and 15 patients (42.9%) are Delbet type 4 fracture. Using the Ratliff’s method, 25 patients (71.4%) had satisfactory outcomes. Ten patients (28.6%) had unsatisfactory outcomes. The complications as AVN, coxa vara and premature closure of physis, non-union and postoperative infections have been detected in this study. AVN was seen in four (11.4%) patients. In addition, coxa vara was seen in six (17.2%) patients.
Conclusion
Pediatric femoral neck fractures are extremely rare fractures and can be treated with low complication rates in cases with early treatment and anatomic reduction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Objective
Pediatric proximal femur fracture is extremely rare trauma comparing to other fractures. The proximal femur fracture is 1% of all pediatric fractures [1]. In addition, the pediatric proximal femur fracture accompanies usually with other traumatic conditions which are neurologic conditions, abdominal trauma, head and neck and thorax trauma [2]. The pediatric proximal femur fracture is highly linked to complications because of the diffrence of blood supply and high-energy falls. The pediatric proximal femur has less anastomosis and collateral blood circulation. In this condition, the pediatric proximal femur is imperilment [3]. The pediatric proximal femur fracture is emergency, so diagnosis, treatment and follow-up are critical. The modalities of treatment are pelvic spica cast, closed reduction and pin fixation, closed reduction and screw fixation, open reduction and internal fixation and also dynamic hip screws [4]. Nevertheless, the rate of avascular necrosis is 20%, coxa vara is 20–30%, the rate of premature physeal closure is 28% and non-union rate is 7%. The aim of current study is to compare the incidence of early complications and outcomes of pediatric proximal femur fractures regarding fracture types retrospectively.
Design
The study was approved by the institutional review board and perfomed in accordance with the ethical standards laid down in the Declaration of Helsinki. All patients provided written informed consent before their inclusion in the study. Our inclusion criteria are age below 16 years old, proximal femur fractures with no evidence of tumoral, romathologic and methabolic conditions. Our study includes 35 cases which are criticized by Delbet classification system, modalities of treatment, duration of waiting for surgery, duration of follow-up and also complications.
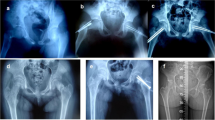
The fractures were classified according to the Delbet system as popularized by Colonna (Fig. 1) [5]. The treatment modalities used were conservative management, open reduction and internal fixation, or closed reduction and internal reduction depending on the patient and the fracture pattern [4].
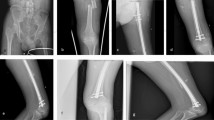
Surgical decisions of the patients were made by the senior attending physician responsible from the emergency cases of that day, and they were operated by two senior surgeons. All cases were operated under general anesthesia and in supine position. At first, closed reduction was applied to each case, and open reduction was applied in cases where sufficient reduction could not be achieved. In cases under 5 years old age with closed reduction application, reduction was achieved under fluoroscopy; afterward, hip spica was applied. Furthermore, in cases over 5 years of age with closed reduction, 4 mm or 6.5 mm cannulated screws were applied percutaneously (Fig. 2). In cases where closed reduction could not be achieved, open reduction was applied with anterolateral approach. Proximal femoral plate, dynamic hip screw, cannulated screw or proximal femoral nail were used for fracture fixation, depending on the pattern of fracture.
Age, sex and surgery type (open-closed) were noted, and the data were statistically assessed. Assessment of the final outcome was made at the last follow-up visit using the Ratliff’s method [6]. A good outcome was rated as a ‘satisfactory outcome’ and fair and poor outcomes or the presence of complications were rated as an ‘unsatisfactory outcome’. Radiographs were evaluated neck-shaft angle and avascular necrosis (AVN) which was further classified according to the Ratliff classification system [6]. Preoperative and postoperative radiographic measures were taken by imaging software used in our hospital named INFINITT PACS (Picture Archiving and Communication Systems) version 3.0.11.4 (BN13).
Statistical analyses were performed with SPSS version 25.0 software. The descriptive analyses were presented using mean, standard deviation, median and interquartile range (IQR) values. The compliance of the variables with normal distribution was examined with histogram graphs and the Kolmogorov–Smirnov test. The independent group t test was used when evaluating the normally distributed (parametric) variables between the groups, and the Mann–Whitney U test and Kruskal Wallis H test were used when evaluating the non-normally distributed (non-parametric) variables between the groups. The Chi-square and likelihood ratio tests were used when evaluating the categorical data. Cases where P value was under 0.05 were found as statistically significant.
Results
The mean of age of patients in our study is 9.5 ± 5.06 years. Our study consists of 20 boys (57.1%) and 15 girls (42.9%). The duration of waiting for surgery is averagely 7 h (IQR, 11 h). The average follow-up was 25.6 ± 13.2 months. There is no patient which is type1 Delbet fracture. 15 patients (42.9%) are type 2 Delbet fracture, 5 patients (14.2%) are Delbet type 3 and 15 patients (42.9%) are Delbet type 4 fracture. The data of the patients are shown in detail in Table 1.
Using the Ratliff’s method, 25 patients (71.4%) had satisfactory outcomes. Ten patients (28.6%) had unsatisfactory outcomes. The complications as AVN, coxa vara and premature closure of physis, non-union and postoperative infections have been detected in this study. AVN was seen in four (11.4%) patients. three of these patients were Delbet type 2; the remaining patient is also type 3. In addition, coxa vara was seen in six (17.2%) patients (Fig. 3). When the relationship between complications and fracture types was examined, no statistically significant difference was observed (p 0.14, p 0.62). Other complications were not reported in our study. The complications of the patients included in the study are shown in detail in Table 2. Complications were observed in a total of 10 patients in the study, and none of them had satisfactory outcomes.
Conclusion
Femoral neck fractures are very rare in the pediatric age group. Although there are orthopedists who have not encountered these cases throughout their professional life, it has been observed in a few studies in the literature that the number of patients is higher than our study [4, 7,8,9]. Considering the studies in the literature in the last decade, it is the study with the highest number of cases as far as we know. When these studies were compared with the AVN rates, it was observed that our results were better (Table 3).
Femur neck fractures were initially classified according to the four-part classification system described by Delbet and popularized by Colonna [5]. Most of the studies on femoral neck fractures in children reported Delbet type 2 fractures as the most common, followed by type 3 (both types constitute about 65–85% of all cases of pediatric fractures of the femoral neck) and type 4 (12%). Type 1 fractures (transepiphyseal) are extremely rare in the literature [3, 4, 6, 7]. In our study, type 1 fracture was not observed in accordance with the literature; type 2 and 4 were the most common type of fracture.
Avascular necrosis is the most common complication following femoral neck fracture in children. The risk of avascular necrosis depends on several factors, including age, degree of initial displacement, type of fracture and time to surgery [6, 7, 10,11,12,13,14,15]. The most important factor is the severity of vascular damage sustained at the time of trauma [16]. A meta-analysis of 360 pediatric femoral neck fractures [14] demonstrated that osteonecrosis in type 1, 2 and 3 fractures were 15, 6 and 4 times more frequent than in type 4 fractures. Furthermore, osteonecrosis was 1.14 times more frequent in older children for each year of increasing age. This occurs because these patients lack the ability to revascularize the femoral head. Furthermore, due to their attitude, type 1, 2 and 3 fractures occur more often than in younger children. Considering the distribution of fracture types in our study, it is seen that type 4 fractures are at the same rate as type 2 fractures. However, type 2 is the most common type in the literature and it has been seen that it is significantly more than type 4. In this case, the same rate of type 2 and type 4 fractures in our study may have caused our AVN rate to be lower.
Femur neck fractures in children are always a result of high-energy trauma for the reason that the femoral neck of children is dense and hard compared to adult femoral neck. As a result, these fractures are usually associated with other injuries which should be addressed [4]. In our study, it was observed that 77% of these rare fractures were due to traffic accidents and fall from height.
Coxa vara is also an important complication. Varus deformity is usually not a primary complication, but secondary to AVN, non-union, or premature physeal closure or a combination of these complications [13]. Severe coxa vara can shorten the extremity and cause a Trendelenburg lurch. In our study, it was seen at a rate of 17.1%, which is lower than the literature.
The main limitations of our study are that the research was conducted retrospectively and the surgical treatments of the patients included in the study could not be performed by a single surgeon. The small sample size can be considered as a limitation due to the rare fractures. In addition, the fact that the distribution of fracture types is not compatible with the literature may have caused the difference in terms of results.
In conclusion, pediatric femoral neck fractures are extremely rare fractures and can be treated with low complication rates in cases with early treatment and anatomic reduction.
References
Patterson JT, Tangtiphaiboontana J, Pandya NK (2018) Management of pediatric femoral neck fracture. J Am Acad Orthop Surg 26:411–419
Sankar WS, Mehlman CT (2019) The community orthopaedic surgeon taking trauma call:pediatric femoral neck fracture pearls and pitfalls. J Orthop Trauma 33:22–26
Pavone V, Testa G (2019) Surgical treatment with cannulated screws for pediatric femoral neck fractures: a case series. Injury 50:40–44
Bali K, Sudesh P, Patel S, Kumar V, Saini U, Dhillon MS (2011) Pediatric femoral neck fractures: our 10 years of experience. Clin Orthop Surg 3:302–308
Colonna PC (1929) Fracture of the neck of the femur in children. Am J Surg 6:793–797
Ratliff AH (1962) Fractures of the neck of the femur in children. J Bone Joint Surg Br 44:528–542
Togrul E, Bayram H, Gulsen M, Kalaci A, Ozbarlas S (2005) Fractures of the femoral neck in children: long-term follow-up in 62 hip fractures. Injury 36:123–130
Inan U, Köse N, Ömeroglu H (2009) Pediatric femur neck fractures: a retrospective analysis of 39 hips. J Child Orthop 3:259–264
Morsy HA (2001) Complications of fracture of the neck of the femur in children. A long-term follow-up study. Injury 32:45–51
Canale ST, Bourland WL (1977) Fracture of the neck and intertrochanteric region of the femur in children. J Bone Joint Surg Am 59:431–443
Ratliff AH (1974) Fractures of the neck of the femur in children. Orthop Clin North Am 5:903–924
Mirdad T (2002) Fractures of the neck of femur in children: an experience at the Aseer Central Hospital, Abha, Saudi Arabia. Injury 33:823–827
Bagatur AE, Zorer G (2002) Complications associated with surgically treated hip fractures in children. J Pediatr Orthop B 11:219–228
Moon ES, Mehlman CT (2006) Risk factors for avascular necrosis after femoral neck fractures in children: 25 Cincinnati cases and meta-analysis of 360 cases. J Orthop Trauma 20:323–329
Bombaci H, Centel T, Babay A, Türkmen IM (2006) Evaluation of complications of femoral neck fractures in children operated on at least 24 hours after initial trauma. Acta Orthop Traumatol Turc 40:6–14
Tetsunaga T, Akazawa H, Tetsunaga T (2014) Intra-articular loose body caused by avascular necrosis of the femoral head in children. J Pediatr Orthop B 23:44–48
Leung PC, Lam SF (1986) Long-term follow-up of children with femoral neck fractures. J Bone Joint Surg Br 68:537–540
Flynn JM, Wong KL, Yeh GL, Meyer JS, Davidson RS (2002) Displaced fractures of the hip in children. Management by early operation and immobilisation in a hip spica cast. J Bone Joint Surg Br 84:108–112
Funding
None declared.
Author information
Authors and Affiliations
Contributions
M.Y. designed the protocol, reviewed the literature, analyzed the data, and critically reviewed and wrote the manuscript. O.O. and A.Y. analyzed the data, reviewed the literature, and critically reviewed and wrote the manuscript. T.O.B. and Y.İ. designed the protocol, collected and analyzed the data, and reviewed the literature. M.Ç.K. and S.S.D. collected and analyzed the data. H.G. collected and analyzed the data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yerli, M., Ocak, O., Yüce, A. et al. Retrospective analysis of 35 pediatric femoral neck fractures. Eur J Orthop Surg Traumatol 32, 1385–1390 (2022). https://doi.org/10.1007/s00590-021-03126-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-021-03126-6