Abstract
Background
Deep soft tissue sarcomas are frequently in contact with bone. The therapeutic decision of a composite resection strategy may be challenging, which is usually based on clinical and radiological criteria. The aims of the study were to evaluate the overall frequency of bone and periosteal infiltration in these patients in whom composite resection was indicated, and evaluate the role of magnetic resonance imaging and bone scintigraphy in this scenario.
Methods
Forty-nine patients with a composite surgical resection (soft tissue sarcoma and bone), treated at a single institution between 2006 and 2018, were retrospectively included. Presurgical planning of the resection limits was based on clinical and imaging findings (magnetic resonance imaging and bone scintigraphy). Magnetic resonance imaging was performed in all patients (100%) and bone scintigraphy in 41 (83.7% of the cases). According to magnetic resonance imaging results, patients were divided into two groups: Group A, in which the tumor is adjacent to the bone without evidence of infiltration (n = 24, 48,9%), and Group B, patients with evidence of bone involvement by magnetic resonance imaging (n = 25, 51,1%). BS showed a pathological deposit in 28 patients (68.3%). Histological analysis of the resection specimen was preceded to identify bone and periosteal infiltration. For the analysis of the diagnostic validity of imaging tests, histological diagnosis was considered as the gold standard in the evaluation of STS bone infiltration.
Results
Histological bone infiltration was identified in 49% of patients and isolated periosteal infiltration in 14.3%. In terms of diagnostic accuracy, magnetic resonance imaging and bone scintigraphy sensitivity values were 92% and 90%, and their specificity values were 91.7% and 52.4%, respectively.
Conclusions
The incidence of bone and periosteal infiltration of soft tissue sarcomas in contact with bone is high. Presurgical bone assessment by MRI has proven to be a sensitive and specific tool in the diagnosis of bone infiltration. Due to its high negative predictive value, BS is a useful test to rule out it. In those cases, in which there is suspicion of bone infiltration not confirmed by MRI, new diagnostic protocols should be established in order to avoid inappropriate resections.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
INTRODUCTION
Surgical removal with wide margin is widely recognized as the main treatment of soft tissue sarcomas (STS) [1], either by limb-sparing surgery or by amputation. Currently, there is not a well-stablished consensus about its optimal width [2, 3], which depends on variables related to the anatomical location of the tumor, the type and histological grade, as well as the use of adjuvant radiotherapy [1, 4].
The preoperative planning for a limb salvage procedure should include a careful evaluation of the local extension of the tumor, including the surrounding bone structures. The current knowledge about STS and bone involvement is scarce, making the diagnostic and therapeutic management more challenging.
In clinical practice, magnetic resonance imaging (MRI) and bone scintigraphy (BS) serve as a guide in decision-making for resection through the periosteum or bone. There is scarce literature about the validity of these imaging tests in the assessment of bone infiltration. The importance of this presurgical evaluation lies in two main points: recent studies have suggested a worse prognosis in those patients with bone infiltration [5,6,7], and wide surgical resections are associated with a higher rate of postsurgical complications and worse limb function [5].
Previous studies focused on the frequency of bone infiltration in soft tissue sarcomas were based on series in which all STS were included, regardless of their anatomical relationship with the bone [5, 7, 8]. Nonetheless, the frequency of bone infiltration of STS that were in contact with bone has not been studied.
Therefore, the aims of our study were: 1) to know the frequency of bone infiltration in patients with bone resection by anatomical proximity with a STS and 2) to assess the diagnostic validity of MRI and BS to detect bone infiltration by STS.
Patients and methods
Study design and patient population
After the local ethical committee’s approval, we performed a study which included 60 patients with STS and composite resection of bone and soft tissue. All these patients were treated at our tertiary referral musculoskeletal oncology center from January 2006 and December 2018. This is a retrospective observational study based on collected data from medical records, surgical protocols, imaging studies, and histological reports.
As regards inclusion and exclusion criteria, our series included patients over 16 years old with STS that were in contact with bone in appendicular skeleton treated with composite resection of bone and soft tissue, due to clinical and radiological suspicion of bone involvement. All patients were evaluated in a multidisciplinary sarcoma committee in order to decide the most appropriate oncological strategy.
Patients with local recurrence of a previous resection in which there was no suspicion of bone involvement at the time of the first surgery were excluded.
From these 60 patients, 11 were excluded (7 local recurrences, 2 cases of amputation with no suspicion of bone infiltration, and 2 patients without MRI studies). Thus, 49 patients with a median age at diagnosis of 49.9 (34.3–56.6) years were finally included.
Demographic variables (sex and age at diagnosis) and clinical variables were collected and analyzed. Clinical variables were divided into two groups: 1) related to clinical presentation (type and histological grade, location, size, AJCC [American Joint Committee on Cancer] stage [9], presence or absence of metastasis at diagnosis) and 2) Related to diagnostic and therapeutic approach (imaging tests, type of surgical technique as well as neoadjuvant chemotherapy, radiotherapy in monotherapy or in combination. Baseline clinical characteristics are shown in Table 1.
Preoperative assessment
For the presurgical planning of the resection limits, MRI and BS findings were evaluated, together with the clinical suspicion based on physical examination. MRI was performed in all patients (100%) and BS was studied in 41 (83.7%) of the cases. In all cases, MRI and BS studies were assessed by expert musculoskeletal radiologists and nuclear medicine specialists, following the protocols of their own departments, respectively. Furthermore, the studies must be those closest to the surgery date, and after neoadjuvant treatment if performed.
Radiological criteria in MRI: MRI imaging was performed with a 1.5-T imager, in all studies T1 and T2-weighted sequences were evaluated, as well as after the gadolinium administration, with or without fat suppression sequences. Bone contact was defined as the absence of normal tissue between the tumor and bone without cortical involvement or marrow infiltration, with or without the presence of bone edema, and bone infiltration by the tumor is defined as the loss of a normal soft tissue interface between the tumor mass and the bone cortex on T1-weighted images. The T2-weighted images were evaluated for peritumoral edema and reactive changes extending to the cortical surface to the cortical surface. Two groups of patients were classified according to bone involvement: patients with doubtful or probable infiltration on MRI, in which the tumor is adjacent to the bone without infiltration (Group A); and patients with evidence of bone involvement on MRI, where cortical infiltration was observed with or without marrow involvement (Group B). After MRI evaluation, Group A and Group B were formed by 24 (48.9%) and 25 (51.1%) of the patients, respectively.
Evaluation criteria in bone scintigraphy: BS was performed according to our hospital protocol using Tc99m-HMDP or Tc99m-MIBI as radiotracers. All the significant increases of bone metabolic activity located close to a STS were recorded. BS studies showed an increased radiotracer uptake in 28 patients (68.3%), and no pathological bone activity in the remaining 13 cases (31.7%).
Physical examination: physical examination was used to determine if the STS moved without restraint over the periosteal surface of the bone, or if the tumor appeared firmed to the bone. This evaluation was reproduced in the operating room after the fascia was opened around the tumor.
Surgical management
According to the MRI findings, composite resection of bone and soft tissue was indicated in Group B patients. However, in Group A, the decision was made according to the results of the BS and physical examination. If the sarcoma was fixed to bone, even after fascia had been opened, or the BS scan showed a pathological increase in bone metabolic activity, the composite resection was also indicated. When it was possible to ensure suitable surgical margins and the limb’s function was not compromised, limb salvage surgery was preferred over amputation. Our diagnostic and therapeutic algorithm is shown in Fig. 1.
Histological study
Surgical margins were assessed for macro- and microscopically infiltration and classified in wide margin, marginal, or intralesional by the same pathologists. Bone infiltration was defined as evidence of tumor cells invading bone cortex with or without penetration into the marrow canal. Periosteal infiltration was defined as evidence of tumor cells invading the periosteum without affecting underlying bone tissues. Selected tissue was fixed in 10% buffered formalin, processed and embedded in paraffin wax by conventional techniques. Microscopic evaluation was made on 4-m thick sections stained by hematoxylin and eosin. Immunohistochemical tests were used for histological characterization.
Statistical analysis
Categorical variables were represented as frequency and percentage, and continuous variables, including age, as median value and interquartile range (IR). Categorical variables were compared by χ2 test or Fisher's exact test. All tests were two-sided and differences were considered statistically significant at P values < 0.05. Statistical analysis was performed with SPSS (IBM SPSS Statistics® version 25).
Sensitivity, specificity, predictive values, false positive and false negative rates, as well as diagnostic efficiency were calculated for the assessment of the diagnostic accuracy of the imaging tests by the application of two-by-two tables. For these analyses, histological diagnosis was considered as the gold standard in the evaluation of STS bone infiltration.
Results
Therapeutic management
Limb salvage surgery was indicated in 32 (65.3%) patients, and amputation was restricted to the remaining 17 cases (34.7%). The type of reconstruction (endoprosthesis, biological reconstruction with allografts, or no reconstruction) was individualized according to the patient’s characteristics. Surgical reconstruction was carried out in 21 (42.9%) patients, mostly by tumoral prosthesis (80.1%), in comparison with the use of allografts (19.9%). The remaining 28 (57.1%) patients were not reconstructed because they were small bone resections or amputations. Prophylactic nailing was not performed in any case. Postsurgical complications were present in 19 (38.8%) patients, being those related to the surgical wound (dehiscence and/or skin necrosis), the most frequent ones, requiring surgical treatment in 8 of 19 cases. No patient’s patient suffered allograft fracture or prosthetic explant during follow-up time.
In forty patients (81.6%), the oncological margin was wide (R0). The remaining nine cases showed a microscopically positive margin (R1). There were no patients with macroscopically positive margin (R2). Those patients with a R1 margin were treated early by enlargement margin surgery, followed by radiotherapy in two of them. In the other cases, different postoperative adjuvant regimens with radiotherapy, chemotherapy, or a combination of both, were prescribed. A total of 27 (55.1%) patients received adjuvant treatment. The adjuvant use of radiotherapy was restricted to patients with conservative limb surgery (7 out of 32, 21.9%). Fourteen patients (28.6%) received chemotherapy and 6 patients (12.2%), both treatments. Eleven out of 19 patients (57.9%) who presented complications, received any type of adjuvant therapy: 6 patients received chemotherapy, 1 patient received radiotherapy, and 4 patients, both of them.
Overall incidence of bone infiltration in soft tissue sarcomas
Of the 49 patients included in the study, histological bone infiltration was confirmed in 24 of the 49 patients, representing an incidence of bone infiltration in 49% of cases. The pathology reports also described periosteal involvement without bone involvement in 7 of 49 patients (14.3%). Therefore, there was bone infiltration or periosteal involvement in 63.3% of cases.
However, there were no significant differences according to type and histological grade, location, size, AJCC, type of surgical technique, neoadjuvant or adjuvants treatments (chemotherapy, radiotherapy in monotherapy or in combination); surgical margins, local recurrence, development of metastases or death. A comparison between patients with and without bone infiltration is shown in Table 2.
Diagnostic accuracy of MRI and BS in the detection of bone infiltration
As summarized in Table 2, BS has shown a sensitivity of 90% with a specificity of 52.4% in detecting bone infiltration, what implies a high false positive rate (47.6%). Regarding predictive values, the negative predictive value was higher than the positive (84.6% vs. 64.3%), and the efficiency of BS was 70.7%.
Concerning MRI, it showed a sensitivity of 92% and a specificity of 91.7%. Considering a doubtful result as negative, positive predictive value was 92% and negative predictive value 91.7%. The efficiency for MRI was 91.8%.
Some examples which show the correlation between imaging and histological findings are represented in Figs. 2, 3, and 4.
A 42-year-old patient with synovial sarcoma around the right scapula. a. MRI shows STS in intimate contact with the scapula, with an infiltrative appearance but without evident bone involvement. b. Increased radiotracer uptake in soft tissues around the right scapula, with no bone involvement. c. Surgical specimen after scapulectomy, which confirms the presence of free bone margins. d, e. Histological samples with hematoxylin–eosin staining (× 4 and × 10, respectively), which show basophilic areas enriched in tumoral cells of synovial sarcoma (within the blue rectangle), next to the bone and the periosteum, which are preserved
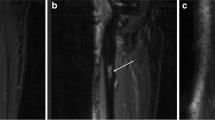
A 52-year-old patient with right thigh rhabdomyosarcoma. a. MRI which shows a tumor in the anterior compartment of the thigh that reaches laterally the medial periosteum of the distal metaphysis of the femur, and infiltrates the distal tendon of the adductor magnus. b. BS scan which shows pathological uptake in the distal region of the right femur suggestive of bone involvement. c. Microscopic periosteal infiltration without bone involvement
57-year-old patient with right foot synovial sarcoma. a. MRI shows a tumor which ruptures the cortical and invades the bone at the diaphysis of the first and second metatarsal bones. b. BS scan which shows pathological uptake in right foot’s tarsus and metatarsus. c. Microscopic periosteal and bone infiltration
DISCUSSION
The current knowledge about STS and bone involvement is scarce, making the therapeutic management more challenging. MRI has become the preferred modality for evaluating the local extension of the tumor and the proximity to critical structures such as the bone. When MRI shows an evident tumor involvement in the underlying bone, a composite resection is indicated. However, when there is no clear evidence of bone involvement, the surgical decision must be made according to physical examination and other imaging studies such as BS. This is relevant because a positive surgical margin at the time of resection has consistently been shown to be the most important predictive factor of local recurrence of STS [10, 11]. In addition, recent studies have suggested that there may be a worse prognosis for patients with tumor bone involvement [5,6,7, 12, 13]. Our study is based on one of the largest series to date, focused on the evaluation of the real incidence of bone infiltration in STS in patients with clinical and radiological suspicion. Furthermore, the simultaneous assessment of the diagnostic accuracy of the main imaging tests in charge of defining oncological margins and subsequently, the most suitable presurgical planning.
Overall incidence of bone infiltration in our series was 49%, higher than those ones previously reported. In 2006, Patrick P. Lin et al. analyzed bone infiltration in 50 patients with STS in the lower extremities, according to computed tomography scan and MRI findings. The composite resection of soft tissue and adjacent bone tissue was performed only in 11 cases, and a real histological bone infiltration was confirmed in 3 of 50 cases (6%) [8]. When comparing our study to Lin's series, a noticeable discrepancy in bone infiltration is detected (6% vs 49%), due to different selection criteria. Lin et al. included all high-grade STS, over 5 cm, with or without bone resection. In our study, all the patients had radiological suspicion of bone involvement, and bone resection was performed in all of them. If we focus on that subgroup of patients with suspicion of bone infiltration in Lin’s series, the incidence of histological infiltration rises to 27.3% [8]. Regarding adjuvant treatments, the predominance of chemotherapy over other treatments is remarkable. This is partially justified by the high rate of synovial sarcomas (n = 10, 20.4%), which were treated in 60% of cases with chemotherapy, and in 30% of cases with different combinations of chemotherapy and radiotherapy. Nevertheless, 22 patients (44.9%) did not receive any adjuvant treatment and 21.9% of the patients received radiotherapy. The previous extensive resections performed in some patients, and the presence of complications, such as dehiscence of the surgical wound and local infection (22.5%), explain this low percentage in comparison with other authors [1, 2, 6, 8, 9].
From a clinical perspective, it is more interesting to know the incidence of infiltration in those cases in which the tumor rests on the bone due to its clinical and therapeutic implications. We have observed that in 49% of the cases there was bone infiltration; hence, a composite resection of the STS and bone was necessary to obtain a negative margin. In addition, our study also evaluated periosteal infiltration (14,3%) in this group of patients. Although it remains true that the recurrence rate depends on the adequacy of the surgical margins, the periosteum is an adequate margin in the absence of bone infiltration [5]. In those cases, in which the periosteum is infiltrated, some authors support a composite resection with the bone in order to obtain a wide margin. On the contrary, other authors have suggested that the periosteum may behave as an adequate margin in this particular scenario, even if it is very thin or even focally positive, not carrying a substantial risk of recurrence at the bone interface, as long as postsurgical radiotherapy is applied [8].
An accurate radiological assessment of the extension of the STS provides critical anatomical information for planning the surgical approach. According to our results, MRI has shown to be an accurate diagnostic technique for this task, with high sensitivity (92%) and specificity (91.7%). Other studies focused on the effectiveness of MRI for the detection of bone involvement in STS have reported similar results to ours (sensitivities from 90 to 100%, and specificities from 88 to 89%) [14,15,16,17]. In cases of doubtful infiltration, our diagnostic protocol included the use of physical examination and BS in the decision-making algorithm. BS is a useful test to rule out bone infiltration due to its high sensitivity (90%), at the expense of a low specificity (52.4%), and a false positive rate that reaches 47.6%.
The results of our study indicate that the overall accuracy of MRI in the detection of bone involvement by STS is high, regardless of physical examination and BS. In 2 out of the 25 cases with histological bone infiltration, MRI was not able to detect it. Analyzing deeply these two cases, we observed that they both had received neoadjuvant radiotherapy. Some authors have reported that prior radiotherapy could contribute to peritumoral changes of increased signal intensity in MRI (mainly because of the presence of edema) [18].
In addition, in 18 cases (36.7%), the bone could have been preserved. Therefore, new diagnostic protocols should be established to evaluate this type of patient to avoid unnecessary bone resections. In this scenario, some authors have reported that computerized tomography (CT) is more sensitive than MRI for detecting cortical disruption, whereas MRI is more sensitive and specific for detecting marrow involvement [15]. On the contrary, other authors have reported that intermediate density-weighted MRI may be more sensitive than CT for the detection of shallow cortical lesions in cadavers [16, 19].
Due to its high negative predictive value, BS is useful to rule out bone infiltration, and it could be of high value when MRI does not detect bone infiltration. In those cases, a resection through the periosteum could be performed, due to the low probability of bone infiltration.
In those cases, without evident bone infiltration in MRI, a CT scan could also be considered to assess the bone cortex [13, 16, 19].
Limitations
Although cases were consecutively included, this is a retrospective cohort study with all the intrinsic limitations.
A potential selection bias is based on the fact that all the patients had a previous suspicion (clinical and/or radiological) of bone infiltration; therefore, our results about incidence of bone infiltration and diagnostic accuracy of imaging tests are limited to this subgroup.
Although the total number of patients included is not low, there is great heterogeneity in terms of histological variant, grade, stage, type of adjuvant treatment, and follow-up period compared to other STS series.
Conclusions
The frequency of bone and periosteal infiltration of soft tissue sarcomas in contact with bone is high. In STS with suspicion of bone involvement and subsequent bone resection, the incidence of histological bone infiltration is 49% and periosteal involvement is 14.3%.
Presurgical bone assessment by MRI has proven to be a sensitive and specific tool in the diagnosis of bone infiltration. Due to its high negative predictive value, BS is a useful test to rule out it. In those cases, in which there is suspicion of bone infiltration not confirmed by MRI, new diagnostic protocols should be established in order to avoid inappropriate resections.
Acknowledgments
We thank Carlos Nicolás Pérez and Raquel Álvarez for their editing help and our colleagues in the musculoskeletal oncology team for their collaboration in the final result of the article.
References
Ahmad R, Jacobson A, Hornicek F, Haynes AB, Choy E, Cote G, Nielsen GP, Chen YL, DeLaney TF, Mullen JT (2016) The width of the surgical margin does not influence outcomes in extremity and truncal soft tissue sarcoma treated with radiotherapy. Oncologist 21(10):1269–1276. https://doi.org/10.1634/theoncologist.2015-0534
Harati K, Goertz O, Pieper A, Daigeler A, Joneidi-Jafari H, Niggemann H, Stricker I, Lehnhardt M (2017) Soft tissue sarcomas of the extremities: surgical margins can be close as long as the resected tumor has no Ink on It. Oncol 22(11):1400–1410. https://doi.org/10.1634/theoncologist.2016-0498
Kandel R, Coakley N, Werier J, Engel J, Ghert M, Verma S, Sarcoma Disease site group of cancer care ontario’s program in evidence-based care (2013) Surgical margins and handling of soft-tissue sarcoma in extremities: a clinical practice guideline. Curr Oncol 20(3):e247–54
Endo M, Lin PP (2018) Surgical margins in the management of extremity soft tissue sarcoma. Chin Clin Oncol 7(4):37. https://doi.org/10.21037/cco.2018.08.10
Ferguson PC, Griffin AM, O’Sullivan B, Catton CN, Davis AM, Murri A, Bell RS, Wunder JS (2006) Bone invasion in extremity soft-tissue sarcoma: impact on disease outcomes. Cancer 106(12):2692–2700. https://doi.org/10.1002/cncr.21949
Gronchi A, Lo Vullo S, Colombo C, Collini P, Stacchiotti S, Mariani L, Fiore M, Casali PG (2010) Extremity soft tissue sarcoma in a series of patients treated at a single institution: local control directly impacts survival. Ann Surg 251(3):506–511. https://doi.org/10.1097/SLA.0b013e3181cf87fa
Panicek DM, Go SD, Healey JH, Leung DH, Brennan MF, Lewis JJ (1997) Soft-tissue sarcoma involving bone or neurovascular structures: MR imaging prognostic factors. Radiol 205(3):871–875
Lin PP, Diaz E, Normand AN, Deavers MT, Cannon CP, Ballo MT, Pisters PW, Pollock RE, Lewis VO, Zagars GK, Yasko AW (2007) Periosteal Margin in Soft-Tissue Sarcoma. Cancer 109(3):598–602. https://doi.org/10.1002/cncr.22429
Amin MB, Edge S, Greene et al (2018) AJCC cancer staging manual, 8th edn. Springer International Publishing
Stefanovski PD, Bidoli E, De Paoli A et al (2002) Prognostic factors in soft tissue sarcomas: a study of 395 patients. Eur J Surg Oncol 28:153–164. https://doi.org/10.1053/ejso.2001.1242
Stojadinovic A, Leung DH, Hoos A, Jaques DP, Lewis JJ, Brennan MF (2002) Analysis of the prognostic significance of microscopic margins in 2,084 localized primary adult soft tissue sarcomas. Ann Surg 235:424–434. https://doi.org/10.1097/00000658-200203000-00015
Williard WC, Hajdu SI, Casper ES, Brennan MF (1992) Comparison of amputation with limb-sparing operations for adult soft tissue sarcoma of the extremity. Ann Surg 215:269–275. https://doi.org/10.1097/00000658-199203000-00012
White LM, Wunder JS, Bell RS et al (2005) Histologic assessment of peritumoral edema in soft tissue sarcoma. Int J Radiat Oncol Biol Phys 61:1439–1445. https://doi.org/10.1016/j.ijrobp.2004.08.036
Kransdorf MJ, Murphey MD (1997) The use of gadolinium in the MR evaluation of soft tissue tumors. Semin Ultrasound CT MR 18:251–268. https://doi.org/10.1016/s0887-2171(97)80016-9
Berthoty D, Haghighi P, Sartoris DJ, Resnick D (1989) Osseous invasion by soft-tissue sarcoma seen better on MR than on CT (letter). AJR Am J Roentgenol 152:113. https://doi.org/10.2214/ajr.152.5.1131-a
Elias DA, White LM, Simpson DJ, Kandel RA, Tomlinson G, Bell RS, Wunder JS (2003 Oct) Osseous invasion by soft-tissue sarcoma: assessment with MR imaging. Radiology 229(1):145–152. https://doi.org/10.1148/radiol.2291020377
Panicek DM, Gatsonis C, Rosenthal DI et al (1997) CT and MR imaging in the local staging of primary malignant musculoskeletal neoplasms: report of the Radiology Diagnostic Oncology Group. Radiology 202:237–246. https://doi.org/10.1148/radiology.202.1.8988217
Richardson ML, Zink-Brody GC, Patten RM, Koh WJ, Conrad EU (1996) MR characterization of post-irradiation soft tissue edema. Skeletal Radiol 25:537–543. https://doi.org/10.1007/s002560050131
Preidler KW, Brossmann J, Daenen B et al (1997) Measurements of cortical thickness in experimentally created endosteal bone lesions: a comparison of radiography, CT, MR imaging, and anatomic sections. AJR Am J Roentgenol 168:1501–1505. https://doi.org/10.2214/ajr.168.6.9168714
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The author(s) declare that they have no competing interests
Ethical standards
The study has been approved by the ethics committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Merino-Rueda, . ., Barrientos-Ruiz, I., Bernabeu-Taboada, D. et al. Radiological and histopathological assessment of bone infiltration in soft tissue sarcomas. Eur J Orthop Surg Traumatol 32, 631–639 (2022). https://doi.org/10.1007/s00590-021-03018-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-021-03018-9