Abstract
Introduction
Currently, the best and simplest way that used to select the distal femoral valgus cut (DFVC) angle in total knee arthroplasty (TKA) is standing long leg radiograph. However, this kind of film is still not available in all hospitals. The purpose of this study is to compare the accuracy of different empirical DFVC angles in the restoration of the neutral mechanical alignment of the femoral component after TKA.
Method
125 patients who diagnosed primary osteoarthritic knee and underwent unilateral TKA were randomly assigned into three groups: A, B, and C, according to the use of an intramedullary guide with the DFVC angle of 4°, 5°, and 6°, respectively. At three months after surgery, anteroposterior hip-to-ankle computed tomography (CT) scanograms were evaluated. Mechanical axis angle (MAA), mechanical lateral distal femoral angle (LDFA), femoral bowing, femoral neck-shaft angle (FNSA), and outliers of femoral component position were measured and compared among three groups. Independent influencing factors for the outliers > ±3° were determined using binary logistic regression analysis.
Results
Group B was older than group A. There were no significant differences of postoperative MAA, LDFA, femoral bowing, and FNSA among three groups. Outliers > ±3° of femoral component position in each group were 14.6%, 19.0%, and 16.7%, respectively (p = 0.865). When considering the outliers > ±2°, group C (35.7%) had a trend to have fewer outliers than groups A and B (41.5 and 42.9%). However, this finding was not reached the statistical significance (p = 0.778). Femoral bowing was only significantly influencing factors that related to the outliers > ±3° (p = 0.003).
Conclusion
This study demonstrates that there are no significant differences in coronal femoral component alignment among using the DFVC angle of 4°, 5°, and 6°. The use of the DFVC angle of 6° had a trend to reduce the outliers. Nevertheless, femoral bowing is the crucial influencing factor for selecting the degree of DFVC angle.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Accurate coronal alignment after total knee arthroplasty (TKA) is one of the critical factors that correlate with good clinical outcome [1]. According to Insall’s concept [2], most surgeons aim to realign the knee to the neutral mechanical axis. Setting the alignment in TKA, the conventional instruments are commonly used. It consists of an extramedullary guided rod for proximal tibial resection and intramedullary (IM) guided rod for distal femoral resection. Nevertheless, this method has a limited degree of accuracy and leads to malalignment or outliers. Alcelik et al. [3] conducted a meta-analysis of 12 studies and revealed that 26.2% of TKA using conventional instruments had overall alignment outliers > ± 3° and 17.6% of femoral and 8.8% of the tibial component had outliers > ±3° in the coronal plane, respectively.
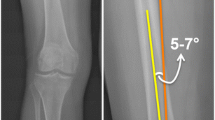
Accuracy of the use of IM guided rod in femoral component placement is depended on several factors, including the fitness of rod within the femoral canal, impaction of plate to rest against the distal femoral condyles [4], location of the entry point into the distal femur [5], femoral bowing in coronal plane [6], height of the patient [7], and selection of a distal femoral valgus cut (DFVC) angle. The degree of the DFVC angle can be determined with several methods. First, the distal femur is resected at a fixed angle. Based on the assumption that the angle between the femoral anatomical and mechanical axis is approximately 5° [8], a fixed valgus correction angle of 5° is chosen. Nevertheless, the variation of this angle is depended on individuals and preoperative deformity [9]. Second, using the standing preoperative long leg radiograph, the DFVC angle is measured from the difference between the femoral anatomical and mechanical axis. Nevertheless, this benefit is still unclear [4, 10]. Furthermore, several hospitals have a limited facility of standing long leg radiographs. Thus, most surgeons have to performed TKA using only conventional knee radiograph preoperatively.
As we knew, this is the first randomized controlled trial that aims to find out the best empirical DFVC angle [4°, 5°, and 6°] to restore the neutral mechanical axis of the femoral component after TKA. Additionally, we also aim to determine the influencing factors to coronal malalignment of femoral component positioning.
Materials and methods
Our institutional review board approved this study. The Thai patients who were diagnosed with primary osteoarthritic knee and scheduled to undergo unilateral TKA were recruited. Patients with previous complex knee surgery, extra articular deformity of the knee, retained hardware at hip or femur, and those who refused consent were excluded. In the operative theater, all eligible patients were randomly assigned to three groups according to the degree of DFVC angle; groups A, B, and C used 4°, 5°, and 6°, respectively. A randomized sequence was generated by a computer program using the blocks-of-six technique. The sequence was concealed by opaque envelopes and opened by the scrub nurse before the operation.
Three experienced arthroplasty surgeons (CK, NR, and PC) who used similar surgical techniques performed all the operations. All TKAs were carried out under regional anesthesia using a tourniquet pressure of 300 mmHg. A mini-medial parapatellar approach was used. In 90° of knee flexion, osteophytes around intercondylar notch were removed for identifying its upper border. Whiteside’s line [11], which defined as a line from the deepest part of the trochlea groove anteriorly to the center of the intercondylar notch, was drawn. An entry point for IM guided rod was marked as 2 mm medial and 10 mm superior to the top of intercondylar notch [12]. The 8 mm IM drill with the step was used to drill a hole at the entry point. The side-cutting minimal invasive surgery quadriceps-sparing (MIS-QS) instrumentation (Zimmer, Warsaw, IN, US) was used to perform the distal femoral bone cut (Fig. 1). The degree of the DFVC angle of the instrument was selected according to the randomized sequence. The proximal tibia was cut perpendicular to the mechanical axis using an extramedullary guided rod. All patients received the cemented Nexgen LPS-Flex fixed-bearing prosthesis (Zimmer, Warsaw, IN, US) without patellar resurfacing.
Demographic data including age, gender, operated side, weight, height, body mass index (BMI), and preoperative anatomical femorotibial angle (FTA) were recorded. At three months after surgery, anteroposterior hip-to-ankle computed tomography (CT) scanograms, with the patella orientated straight ahead and centered over the femoral condyles, were evaluated. Two independent blinded outcome assessors measured the radiographic outcomes using the digital tools of the picture archiving and communication system (PACS). The center of the femoral head was determined using the circle tool. The center of the knee was defined as the apical midpoint of the intercondylar notch of the femoral component. The center of the talar dome was defined as the center of the ankle. The femoral mechanical axis (FMA) was described as a line between the center of the femoral head and the center of the knee, while the tibial mechanical axis (TMA) was described as a line between the center of the knee and the center of the ankle. Mechanical axis angle (MAA) defined as the angle between FMA and TMA was measured. The femoral component alignment was determined using the lateral distal femoral angle (LDFA). This angle formed by a line connecting the distal femoral component surface and the FMA (Fig. 2).
a Postoperative hip-to-ankle CT scanogram showing the center of the femoral head (A), the center of the knee (B), the center of the ankle (C), the femoral mechanical axis (FMA), the tibial mechanical axis (TMA) and mechanical axis angle (MAA). b The measurements of lateral distal femoral angle (LDFA), femoral bowing angle (the angle between the line FpFc and FdFc: Fp, a point bisecting the shaft at the lower border of the lesser trochanter; Fd, a point bisecting the shaft 10 cm proximal to the knee joint; and Fc, a point bisecting the shaft midway between Fp and Fd) and femoral neck-shaft angle (FNSA, the angle between femoral neck axis (FNA) and FpFc)
According to the method of Mullaji et al. [6], the femoral bowing was measured in the coronal plane. Three points were marked on the femoral shaft as followings: Fp, a point bisecting the shaft at the lower border of the lesser trochanter; Fd, a point bisecting the shaft 10 cm proximal to the knee joint; and Fc, a point bisecting the shaft midway between Fp and Fd. Femoral bowing was the angle between the line FpFc and FdFc. The other radiographic parameter, femoral neck-shaft angle (FNSA), was also measured as followings: superior and inferior head-neck junctions were identified. A line between these two points was drawn and defined as the head-neck junction plane. A line crossing the center of the femoral head and perpendicular to the head-neck junction plane was created and represented as a femoral neck axis (FNA). FNSA was the angle between the FNA and the line FpFc (Fig. 2).
To calculated the sample, the previous study of Victor et al. [13] reported that the use of fixed 5° of DFVC angle had 14% of the outlier > ±3° (86% of success rate). In order to detect a significant difference (p < 0.05) with 20% of the non-inferiority margin, a sample size of 38 knees per group was estimated to have sufficient power of 0.8. When combined with an assumed lost-to-follow-up rate of 10%, we recruited a total of 126 patients (42 knees per group) in this study.
Statistical analysis
Data were analyzed using SPSS version 18.0 (Chicago, Illinois). Continuous and categorical data were presented as mean ± standard deviation and number (percentage), respectively. The differences among the three groups were analyzed using one-way ANOVA and chi-square test. Once the differences existed among the mean, Bonferroni post hoc test was used to determine which groups differed. Binary logistic regression analysis was used to identify the influencing factors that related to coronal alignment outliers > ±3° of femoral component positioning. Statistical significance was set at a p-value < 0.05.
Results
A total of 126 patients were recruited in this study. One patient in group A had a loss to follow-up. Thus, the remaining 125 patients were included in the final analysis. The flow of patients was summarized in the CONSORT diagram (Fig. 3). Patient characteristics were comparable among the three groups except for age. Group B was significantly older than group A (Table 1).
For postoperative radiographic outcomes, there were no significant differences of MAA, LDFA, femoral bowing, and FNSA among three groups. The boxplot of LDFA in each group was shown in Fig. 4. The outliers > ±3° of femoral component positioning in groups A, B, and C were 14.6%, 19.0%, and 16.7%, respectively. When considering the outliers > ±2° of femoral component positioning, group C had a trend to have fewer outliers than other groups. However, these findings were not reached the statistical significance (Table 2).
To identify the influencing factors that related to outliers > ±3° of femoral component positioning, The independent variables including age, gender, BMI, femoral bowing, and FNSA were fit in the binary logistic regression model. We found that femoral bowing was only significantly influencing factor that related to the outliers (p = 0.003). Femoral bowing in the patients who had outliers > ±3° was 5.0 ± 4.0°, while in the patients who had not outliers > ±3° was 2.5 ± 2.1° (Fig. 5).
Discussion
The selection of the DFVC angle relied on the relationship between the FMA and anatomical axis of the femur, most commonly mentioned as 5° or 6° [14]. However, the high variation of this angle was found in an Asian population with end-stage osteoarthritis [15]. Although Nam et al. [4] reported that the use of hip-to-ankle radiographs for measuring a DFVC angle could improve the alignment in TKA, this long radiograph was not available in all hospitals due to costly cost and the need for special equipment. Thus, we aimed to find out the best empirical DFVC angle for helping the surgeon to reduce the alignment outliers.
This study's notable findings were no significant difference in femoral component positioning among using 4°, 5°, or 6° of DFVC angle. A 6° DFVC angle had a trend to reduce the outliers > ±2°. Compared with previous studies, Andrews et al. [16] reviewed 788 radiographs and suggested that using a DFVC angle of 6° was a reliable surgical technique and resulted in a neutral alignment in 86% of patients. Moreover, Mullaji et al. [6] reported that the means distal femoral axis-mechanical axis angle in Indian patients were 7.3 ± 1.6°. Their results help explain why using a 6° DFVC angle had a trend to reduce the outliers > ±2° in our study.
The significance of femoral bowing was another important finding in our study. Coronal bowing of femur and tibia were common in Asians with the osteoarthritic knee [6, 17,18,19]. Kobayashi et al. [17] reported that femoral bowing in Japanese patients varied from − 7.4° to 10.9°. While Yau et al. [19] demonstrated that the incidence of femoral bowing > 2° in the Chinese population was 62%, with a mean of 5.3 ± 4.0° [19], this value was comparable to the outliers group in our study. Furthermore, Kim et al. [20] found that the femoral IM guide angle was mainly influenced by the shape of the femoral shaft. The femoral bowing had a more significant effect on the coronal alignment of TKA than proximal (or FNSA) or distal variations (or LDFA) of femoral shape. In the limited-resource hospital, we recommended that the evaluation of femoral bowing using anteroposterior radiograph of femur might be advantageous for reducing the femoral component outliers.
If a standing long leg radiograph was not feasible in clinical application, we recommended routinely using the 6° DFVC angles to reduce the femoral component outlies, especially in the Asian population. In another option, the surgeon could decide the optimal DFVC angle from the preoperative anteroposterior radiograph of the femur available in any hospital.
Limitations
There were several limitations to our study. Firstly, we studied only Thai patients relatively small compared to Caucasians. Drexler et al. [7] found that height and medial hip offset were the main determinants of the DFVC angle during TKA. Thus, the alternative results might be happening in other races. Secondly, our study focused only 4°, 5°, or 6° of the DFVC angle. Some studies reported that using a fixed 7° DFVC angle had no significant differences in femoral component alignment than the DFVC angle from hip-to-ankle radiograph measurement [21]. Thirdly, we have known that it was challenging to detect the few degrees of radiographs' differences. Nevertheless, the randomized controlled design, blinding to the assessors, and standard anteroposterior hip-to-ankle CT scanogram could accommodate us to reduce the bias, including the slight rotation of the scanogram that influenced the outcomes were inevitable.
Future direction
This study proved that the distal femoral empirical cut using the IM cutting guide may not be accurately perpendicular to the mechanical axis or as we intended preoperatively. We should go further into the individualized femoral cut by utilizing the feasible tools to enhance the mechanical axis's accuracy, such as requesting long-standing film, gyroscopic assist device, computer-assisted surgery, robotic-arm assisted surgery in the future.
Conclusion
There was no significant difference in femoral component positioning among using 4°, 5°, or 6° of DFVC angle. In terms of the trend to diminish the outliers, the selection of 6° might be the best empirical DFVC angle for the limited-resource hospital. However, all surgeons must consider the critical effect of coronal femoral bowing.
References
Ritter MA, Faris PM, Keating EM, Meding JB (1994) Postoperative alignment of total knee replacement. Its effect on survival. Clin Orthop 299:153–156
Insall JN (ed) (1984) The total knee replacement. In: Surgery of the knee. Churchill Livingstone, New York, pp 1447–64
Alcelik I, Blomfield M, Öztürk C, Soni A, Charity R, Acornley A (2017) A comparison of short term radiological alignment outcomes of the patient-specific and standard instrumentation for primary total knee arthroplasty: a systematic review and meta-analysis. Acta Orthop Traumatol Turc 51(3):215–222
Nam D, Vajapey S, Haynes JA, Barrack RL, Nunley RM (2016) Does use of a variable distal femur resection angle improve radiographic alignment in primary total knee arthroplasty? J Arthroplast 31(9 Suppl):91–96
Reed SC, Gollish J (1997) The accuracy of femoral intramedullary guides in total knee arthroplasty. J Arthroplast 12(6):677–682
Mullaji AB, Marawar SV, Mittal V (2009) A comparison of coronal plane axial femoral relationships in Asian patients with varus osteoarthritic knees and healthy knees. J Arthroplast 24(6):861–867
Drexler M, Abolghasemian M, Barbuto R, Naini MS, Voshmeh N, Rutenberg TF et al (2017) Patient’s height and hip medial offset are the main determinants of the valgus cut angle during total knee arthroplasty. J Arthroplast 32(5):1496–1501
Canale ST, Beaty JH (2008) Campbell’s operative orthopaedics, 11th edn. Elsevier Inc., Philadelphia
Mullaji AB, Shetty GM, Kanna R, Vadapalli RC (2013) The influence of preoperative deformity on valgus correction angle: an analysis of 503 total knee arthroplasties. J Arthroplast 28(1):20–27
McGrory JE, Trousdale RT, Pagnano MW, Nigbur M (2002) Preoperative hip to ankle radiographs in total knee arthroplasty. Clin Orthop 404:196–202
Whiteside LA, Arima J (1995) The anteroposterior axis for femoral rotational alignment in valgus total knee arthroplasty. Clin Orthop 321:168–172
Wangroongsub Y, Cherdtaweesup S (2009) Proper entry point for femoral intramedullary guide in total knee arthroplasty. J Med Assoc Thail Chotmaihet Thangphaet 92(Suppl 6):S1-5
Victor J, Dujardin J, Vandenneucker H, Arnout N, Bellemans J (2014) Patient-specific guides do not improve accuracy in total knee arthroplasty: a prospective randomized controlled trial. Clin Orthop 472(1):263–271
Deakin AH, Basanagoudar PL, Nunag P, Johnston AT, Sarungi M (2012) Natural distribution of the femoral mechanical–anatomical angle in an osteoarthritic population and its relevance to total knee arthroplasty. Knee 19(2):120–123
Lee C-Y, Huang T-W, Peng K-T, Lee MS, Hsu RW-W, Shen W-J (2015) Variability of distal femoral valgus resection angle in patients with end-stage osteoarthritis and genu varum deformity: radiographic study in an ethnic Asian population. Biomed J 38(4):350–355
Andrews SN, Beeler DM, Parke EA, Nakasone CK, Stickley CD (2018) Fixed distal femoral cut of 6° valgus in total knee arthroplasty: a radiographic review of 788 consecutive cases. J Arthroplast
Kobayashi H, Akamatsu Y, Kumagai K, Kusayama Y, Aratake M, Saito T (2017) Influence of coronal bowing on the lower alignment and the positioning of component in navigation and conventional total knee arthroplasty. Orthop Traumatol Surg Res OTSR 103(2):251–256
Lasam MPG, Lee KJ, Chang CB, Kang YG, Kim TK (2013) Femoral lateral bowing and varus condylar orientation are prevalent and affect axial alignment of TKA in Koreans. Clin Orthop 471(5):1472–1483
Yau WP, Chiu KY, Tang WM, Ng TP (2007) Coronal bowing of the femur and tibia in Chinese: its incidence and effects on total knee arthroplasty planning. J Orthop Surg Hong Kong 15(1):32–36
Kim J-M, Hong S-H, Kim J-M, Lee B-S, Kim D-E, Kim K-A et al (2015) Femoral shaft bowing in the coronal plane has more significant effect on the coronal alignment of TKA than proximal or distal variations of femoral shape. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 23(7):1936–1942
Stucinskas J, Robertsson O, Lebedev A, Wingstrand H, Smailys A, Tarasevicius S (2016) Measuring long radiographs affects the positioning of femoral components in total knee arthroplasty: a randomized controlled trial. Arch Orthop Trauma Surg 136(5):693–700
Acknowledgements
The authors acknowledge the assistance given by Nichakorn Khomawut with data collection. We also acknowledge Suthipol Udompunthurak, MSc. (Applied Statistics), for his assistance with the statistical analyses.
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study included human participants. It had been approved by Siriraj Institutional Review Board (SIRB).
Informed consent
Since this study was a retrospective chart review. Informed consent was obtained by phone from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pornrattanamaneewong, C., Ruangsomboon, P., Wingprawat, K. et al. Accuracy of empirical distal femoral valgus cut angle of 4° to 6° in total knee arthroplasty: a randomized controlled trial. Eur J Orthop Surg Traumatol 32, 175–181 (2022). https://doi.org/10.1007/s00590-021-02890-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-021-02890-9