Abstract
Introduction
We describe a fixation technique for tibial tuberosity osteotomies (TTO) utilising a plate and screw construct which adheres to established principles of bone healing. We record and discuss the complication profile and benefits of this technique.
Method
The technique is outlined, and thirty consecutive case of TTO fixed with this combination of plate and screws were analysed during a study period from January 2018 to October 2018. All patients were followed up clinically to 3 months post-operation for the purpose of identifying early complications of surgery. Radiographic series were reviewed at 2, 6 and 12 weeks post-operation for evidence of fracture, loss of position, hardware failure and union.
Results
All cases went on to clinical and radiographic union by 12 weeks. We identified one case of hardware failure, one case of superficial infection and one case of stiffness requiring manipulation.
Conclusion
We have found this technique of plate and screw construct to be effective in arthroscopically assisted TTO fixation leading to consistent union without loss of position with a low complication profile.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Tibial tuberosity osteotomy (TTO) and transfer is a well-described surgical treatment option for a variety of patellofemoral joint (PFJ) disorders. Once osteotomised, the tibial tuberosity can be mobilised in multiple planes addressing patella height and influencing PFJ tracking. Securing the osteotomised tibial tuberosity is a key step in this procedure. Despite wide acceptance and application of this osteotomy, there remains a paucity of literature to guide surgeons on how best to obtain fixation. Ideally, fixation techniques will lend to predictable union, allow functional rehabilitation and carry a low complication profile.
The first described technique of TTO was by Hauser in 1938 and involved a distalisation and medialisation of the patella tendon on a tibial tubercle bone block measuring one-half inch square [1]. This was countersunk and secured into an excised bone block of the same measurements both distal and medial to its origin. This osteotomy was fixed with sutures and reefing of surrounding periosteum. Immobilisation in plaster of Paris was required. Hauser described this operation as a total tendon transplant and so began the lineage of this surgical procedure.
Multiple techniques have now been described for the creation of the osteotomy and its subsequent fixation. Fixation techniques include large-fragment screws, small fragments screws, sutures, staples and cerclage wires. The standard technique for TTO fixation at our institution has utilised two large-fragment, countersunk lag screws. The complication profile of this technique includes but is not limited to: fracture of the tuberosity, fracture of the tibia, loss of position of the tuberosity, non-union and prominent symptomatic metalware [2,3,4,5,6,7].
In an effort to address these complications, we developed a fixation technique utilising a plate and screw construct which adheres to established principles of fracture management. The rationale for this technique is explored, and the union rate and complication profile of our first 30 cases are reported.
Method
Using the Avon surgical registry, we identified thirty consecutive cases of TTO fixed with the new technique during a study period from January 2018 to October 2018.
The procedures were performed by specialist orthopaedic knee surgeons (DC and JDE). Patient demographics, indication for surgery, distance of distalisation and/or medialisation is reported. All patients were followed up clinically to 3 months post-operation for the purpose of identifying complications of surgery. Further follow-up was organised on a case-by-case basis.
The patients’ radiographic series at 2, 6 and 12 weeks post-operation were reviewed on digital radiographs (Kodak© Picture Archiving and Communication System on a liquid crystal display) for evidence of fracture, loss of position, hardware failure and union. Both anteroposterior (AP) and lateral views of the knee were assessed.
Surgical technique
Preoperative planning includes a comprehensive history and examination which must include alignment and rotational profile screening, supplemented by radiographic investigations. All patients routinely undergo plain imaging including weight-bearing anterior–posterior (AP), lateral and skyline views. To objectively assess patella-femoral morphology, magnetic resonance imaging is performed in all cases. Patella height is quantified using the patellotrochlear index as described by Biedert et al. This informs surgical planning, with the goal of normalising patella height to a patellotrochlear index of 30%.
Setup
All patients are examined under anaesthesia prior to tourniquet application. The patient is positioned supine on the operating table with a foot roll set to hold the leg at 70 degrees and a side support secured low on the lateral thigh to allow for adequate manoeuvering during arthroscopy (Fig. 1). A high thigh tourniquet is placed. A single dose of prophylactic antibiotic is administered at the time of induction.
A diagnostic arthroscopy is performed using a 30-degree camera. An accessory superolateral portal facilitates a diagnostic and dynamic assessment of PFJ morphology, congruence, engagement and tracking. Any intra-articular pathology that needs addressing is treated at this stage (chondral flaps, synovial plica, etc.).
Anterolateral approach
An anterolateral approach to the tibial tuberosity is performed. A 10-cm curvilinear incision is used: parallel and 3 cm lateral to the tibial crest. It is centred at the level of the tibial tuberosity with the proximal aspect curving laterally towards Gerdy’s tubercle (Fig. 2).
The anterolateral incision, through careful skin mobilisation, gives access to both the lateral and medial aspects of the patella tendon and tibial tubercle. Through this incision, the skin can be mobilised to access the proximal medial aspect of the tibia should hamstring harvest be required for adjunct procedures such as medial patellofemoral ligament reconstruction (Fig. 3). It is important to identify the proximal insertion point of the patella tendon, which dictates the proximal extent of the osteotomy and avoids intra-articular extension. The surgeon will need to develop a space behind the insertion of the patella tendon to perform the proximal portion of the osteotomy.
The fascia over tibialis anterior is incised, 1 cm parallel to the tibial crest, leaving a cuff of tissue to repair. The lateral aspect of the tibia adjacent to the proposed osteotomy length can be exposed with the use of a periosteal elevator. The exposure required is dictated by the intended osteotomy length. At our institution, a standard osteotomy measures 70 mm in length. Proximally, the depth is 15 mm from the anterior tuberosity crest and carried distally in a horizontal plane which creates a taper in the distal portion of the osteotomy. We favour a step-cut osteotomy to facilitate biplanar compression during subsequent fixation.
Osteotomy
The knee is placed in extension. A moistened pack protects tibialis anterior as it is retracted to expose the bone for osteotomy, which is marked out with diathermy. Using a fan blade saw, the osteotomy is commenced in the coronal plane from the lateral aspect of the tibia (Fig. 4a). Once this cut is complete, the periosteum is divided over the osteotomy medially, joining the proximal paratendinous incision. The predetermined length of distalisation is marked out on the osteotomy fragment. It is usually between 7 and 12 mm. Two parallel cuts are made to remove the predetermined length of bone (Fig. 4b). Prior to distalisation, the fragment must be freed proximally, from both bone and soft tissue. A wide osteotome is used to complete the osteotomy from above, starting approximately 2 cm above the proximal insertion point of the patella tendon (Fig. 4c). It is then imperative to release the robust retro-patella tendinous attachments coursing from the tubercle to the fat pad to allow tension-free distalisation. Using a bone holding forceps, the fragment is elevated and the release is performed as demonstrated in Fig. 4d. The tibial tuberosity is now mobile.
a A sagittal saw is used to perform the tibial tuberosity osteotomy. b Two distal transverse cuts are made to remove the desired amount of bone to distalise the osteotomy. c A broad osteotome is used to complete the osteotomy proximally, aimed at approximately 60 degrees to prevent fracture into the tendinous insertion. d The tuberosity is mobilised and released from retro-patella tendinous attachments
Fixation
Distalisation and, if required, medialisation are performed to the desired position. If the described soft tissue releases are performed, the fragment will sit without tension using a bone holding forceps. Temporary fixation with 2-mm K-wires is also possible. Patella–trochlea engagement and tracking can be assessed arthroscopically at this point. A three-hole, 1/3 tubular, small fragment plate is positioned so that the middle hole is centred over transverse, distal osteotomy cut. A 3.5-mm fully threaded bicortical screw is inserted in the distal hole (Fig. 5). A second 3.5-mm screw is placed through the proximal hole of the plate; this is placed in lag mode and will compress the osteotomy. A third screw is now positioned proximal to the plate and is placed as a lag screw.
Assessment and closure
Arthroscopic assessment is once again carried out through the supra-lateral viewing portal, and images are saved at 0, 20, 40 and 60 degrees of flexion. Figure 6 shows views at 20 degrees flexion of the PFJ pre- and post-tibial tuberosity distalisation. Finally, assessment of osteotomy stability is performed by ranging the knee to 90 degrees of flexion, followed by closure. Waterproof dressing, bandages and articulated knee splint are applied. The patient is allowed to weight bear as tolerated with the splint on and range the knee as tolerated at rest.
Results
From January 2018 until October 2018, thirty consecutive cases of tibial tuberosity osteotomy and transfer using the described technique were performed by the authors JDE (n = 14) and DC (n = 16). Twenty-five patients were female and five were male. The average age of our cohort was 29. The indications for surgery were: patella alta with instability n = 19, patella alta with PFJ pain n = 6, patella alta with PFJ arthritis n = 5. All osteotomies were distalised with the average distance being 9 mm. Five osteotomies were also medialised by an average of 5 mm. A combination of tibial tuberosity transfer and medial patellofemoral ligament reconstruction was performed in 17 cases and a modified Insall soft tissue procedure in five cases.
At the 3-month radiographic check, all cases demonstrated union. We identified one case of hardware failure with the head of a lag screw breaking between weeks six and twelve. This patient demonstrated both radiographic and clinical union; there was no loss of position, and the broken screw head was asymptomatic.
One patient developed superficial infection and was treated with a 10-day course of oral antibiotics. Under the care of the physiotherapists, this same patient was restricted in movement for an extended period while the infection resolved. This resulted in a stiff knee with range of movement 0°–90°. Our patient underwent a manipulation under anaesthetic at 8 weeks post-index procedure. Post-operative range of movement was 0°–130°, and this range was maintained.
Discussion
Tibial tuberosity osteotomy and transfer, although a straightforward procedure, can result in major complications. Such is the importance of the extensor mechanism; any complication can have a dramatic impact on clinical function. In Fulkerson’s original series of 30 tibial tubercle anteromedial transfers, 7% sustained fracture or failure of fixation. Described complications of the procedure included: fracture of the tuberosity, fracture of the tibia, loss of position of the tuberosity, non-union, prominent symptomatic metalware and delayed post-operation functional recovery leading to quadriceps atrophy [2,3,4,5,6,7]. It is our intention to seek an ideal form of fixation which leads to bone union, avoids symptomatic metalware, maintains position of the osteotomy and allows early functional recovery.
Described techniques for fixation of tibial tuberosity osteotomies include: two large-fragment lag screws [8, 9], three small fragment screws [10] and cerclage wire constructs [11, 12]. These are illustrated in Fig. 7 with our technique for comparison.
Werner et al. compared the cyclical loading profile and load to failure characteristics of tubercle osteotomies fixed with either two 4.5-mm cortical screws or three 3.5-mm screws [13]. They found no clinically relevant difference in the constructs loading characteristics. While both constructs can withstand physiological loading, Johnson et al. reported that 3.5-mm screws were less painful and less likely to need removal than the 4.5-mm screws [14]. The trade-off in screw size is the requirement for an additional screw into the tuberosity.
Davies has comprehensively reviewed the use of 4.5-mm screws vs cerclage wires, staples and sutures in the fixation of tubercle osteotomy in the context of knee arthroplasty [15]. Their work confirmed that screws were superior at resisting cyclical loads at a patella tendon angle of 25°, and this reached significance when testing load to failure.
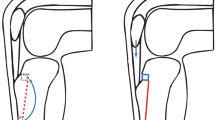
The described techniques involve internal fixation through the tuberosity into the tibia posterior to the osteotomy, the purpose of which is to provide orthogonal compression and promote union. While this is effective in resisting pull-out, loss of position may still occur due to oblique force vectors generated by the patella tendon. The points of fixation with lag screws are at the tapered screw–neck bone interface and the distal cortex. Translation of the osteotomy and therefore loss of position is possible with an intact construct (Fig. 8).
Surgeons at our institute have begun utilising the construct depicted in Fig. 5 in an attempt to address some of these issues. Our construct utilises screws as they have been shown to be superior to cerclage wires. To avoid prominent hardware, our construct utilises 3.5-mm small-fragment screws. To minimise the number of drill holes in the tuberosity, we use two screws in this fragment. To gain orthogonal compression, the first tuberosity screw is placed in lag mode. To prevent loss of position, the tuberosity is held by a screw and plate fixed distally into the tibia acting as a post to prevent translation and fragment elevation.
This construct has the benefit of being low profile while only utilising two screws into the tuberosity and provides orthogonal osteotomy compression while resisting translation. Future studies are planned to evaluate whether this can be translated into early functional rehabilitation and prevention of quadriceps muscle atrophy.
Conclusion
We have found this technique of plate and screw construct to be effective in arthroscopically assisted TTO fixation leading to consistent union without loss of reduction with a low complication profile.
References
Hauser EDW (1938) Total tendon transplant for slipping patella: new operation for recurrent dislocation of the patella. Surg Gynecol Obstet 66:199–214
Stetson WB, Friedman MJ, Fulkerson JP, Cheng M, Buuck D (1997) Fracture of the proximal tibia with immediate weightbearing after a Fulkerson osteotomy. Am J Sports Med 25:570–574
Fulkerson JP (1999) Fracture of the proximal tibia after Fulkerson anteromedial tibial tubercle transfer: a report of four cases. Am J Sports Med 27:265
Bellemans J, Cauwenberghs F, Brys P, Victor J, Fabry G (1998) Fracture of the proximal tibia after Fulkerson anteromedial tibial tubercle transfer: a report of four cases. Am J Sports Med 26:300–302
Wolff AM, Hungerford DS, Krackow KA, Jacobs MA (1989) Osteotomy of the tibial tubercle during total knee replacement: a report of twenty-six cases. J Bone Joint Surg 71A:848–852
Cosgarea AJ, Freedman JA, McFarland EG (2001) Nonunion of the tibial tubercle shingle following Fulkerson osteotomy. Am J Knee Surg 14:51–54
Ritter MA, Carr K, Keating EM, Faris PM, Meding JB (1996) Tibial shaft fracture following tibial tubercle osteotomy. J Arthroplasty 11:117–119
Fulkerson JP (1983) Anteromedialization of the tibial tuberosity for patellofemoral malalignment. Clin Orthop Relat Res 177:176–181
Pemmaraju G, Raad A, Kotecha A, Chugh S, Mughal E (2015) Modified technique of tibial tuberosity transfer. Arthrosc Tech 4(4):349–352
Clark D, Walmsley K, Schranz P, Mandalia V (2017) Tibial tuberosity transfer in combination with medial patellofemoral ligament reconstruction: surgical technique. Arthrosc Tech 6(3):591–597
Whiteside LA, Ohl MD (1990) Tibial tubercle osteotomy for exposure of the difficult total knee arthroplasty. Clin Orthop Relat Res 260:6–9
Mendes MW, Caldwell PE, Jiranek JA (2004) The results of tibial tubercle osteotomy for revision total knee arthroplasty. J Arthroplasty 19:167–174
Warner BT, Kamath GV, Spang JT, Weinhold PS, Creighton RA (2013) Comparison of fixation methods after anteromedialization osteotomy of the tibial tubercle for patellar instability. Arthroscopy 29:1628–1634
Johnson AA, Wolfe EL, Mintz DN, Demehri S, Shubin Stein BE, Cosgarea AJ (2018) Complications after tibial tuberosity osteotomy: association with screw size and concomitant distalization. Orthop J Sports Med 6(10):2325967118803614. https://doi.org/10.1177/2325967118803614
Davis K, Caldwell PE, Wayne J, Jiranek WA (2000) Mechanical comparison of fixation techniques for the tibial tubercle osteotomy. Clin Orthop 380:241–249
Funding
No funds were obtained for this paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interest is declared.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Stevens, J.M., Barton, S.B., Alexander, M. et al. Plate and screw fixation of arthroscopically assisted tibial tuberosity osteotomy: technique and results. Eur J Orthop Surg Traumatol 30, 139–145 (2020). https://doi.org/10.1007/s00590-019-02536-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-019-02536-x