Abstract
Purpose
The purpose of this study was to describe the incidence of subsidence in patients with AO/OTA 41 (tibial plateau) fractures which were repaired with a novel fenestrated screw system to used to deliver CaPO4 bone substitute material to fill the subchondral void and support the articular reduction.
Methods
Patients with unicondylar and bicondylar tibial plateau fractures were treated according to the usual technique of two surgeons. After fixation, the Zimmer Biomet N-Force Fixation System®, a fenestrated screw that allows for the injection of bone substitute was placed and used for injection of the proprietary calcium phosphate bone graft substitute into the subchondral void. For all included patients, demographic information, operative data, radiographs, and clinic notes were reviewed. Patients were considered to have articular subsidence if one or more of two observations were made when comparing post-operative to their most recent clinic radiographs: > 2 mm change in the distance between the screw and the lowest point of the tibial plateau, > 2 mm change in the distance between the screw and the most superior aspect of the plate. Data were analyzed to determine if there were any identifiable risk factors for complication, reoperation, or subsidence using logistic regression. Statistical significance was set at p < 0.05.
Results
34 patients were included with an average follow-up of 32.03 ± 22.52 weeks. There were no overall differences between height relative to the medial plateau or the plate. Two patients (5.9%) had articular subsidence. Six patients (15.2%) underwent reoperation, two (6%) for manipulations under anaesthesia due to arthrofibrosis, and four (12%) due to infections. There were 6 (19%) total infections as 2 were superficial and required solely antibiotics. One patient had early failure.
Conclusion
Use of a novel fenestrated screw system for the delivery of CaPO4 BSM results in articular subsidence and complication rates similar to previously published values and appears to be a viable option for addressing subchondral defects in tibial plateau fractures.
Level of evidence
IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Treatment goals for tibial plateau fractures include restoring the mechanical axis and knee stability. Anatomic reduction of the articular surface is important for stability and efficient load transfer between the femur and tibia. Failure to recreate a stable, well-aligned knee can result in adverse outcomes such as knee pain, post-traumatic arthrosis, and the need for total knee arthroplasty [1,2,3].
Maintaining articular reduction to union can be challenging. Many materials have been proposed to fill the subchondral void and support the articular reduction: autograft, allograft chips or struts, and various bone substitute materials (BSMs) [4,5,6]. Calcium phosphate (CaPO4) is widely used due to its compressive strength in biomechanical [7,8,9] and clinical series [10,11,12,13,14]. Traditionally, CaPO4 is available in multiple forms, including chips, putty, or a viscous injectable through a drill hole in the proximal tibial metaphysis. However, during injection egress of the material can prove problematic; some material is often extruded back through the injection portal, thus reducing available volume in the defect. Moreover, intra-articular material seepage in the post-operative period may necessitate a revision operation [15, 16].
A novel CaPO4 delivery system intended to optimize the delivery of subchondral bone void fillers is commercially available. The N-Force Fixation System (Zimmer Biomet, Warsaw, IN) consists of 4.0- and 7.0-mm fenestrated screws intended to deliver a proprietary CaPO4 bone substitute material (N-Force Blue, Zimmer Biomet, Warsaw, IN) along the screw and into bone defects. However, no data exist to guide surgeons in the potential adoption of this new technology. We sought to define the effectiveness of the system in preventing articular subsidence and to define complications associated with its use.
Methods
We identified patients treated for tibial plateau fractures between August 2016 and October 2018 at three hospitals. Thirty-four patients underwent open reduction internal fixation of tibial plateau fractures with standard plate and screw constructs and fenestrated screw CaPO4 delivery system (OTA/AO 41) by two surgeons (JAS, GSM) and at least one follow-up visit. These fractures represent a series of all patients treated with the device during this time period, beginning with the first use of the device. The decision to use the device was made at the discretion of the operating surgeon. Typically, a contained void (closed space without comminution through which the BSM can egress) with an adjacent surface amenable to screw placement (the screw must be placed orthogonal to the surface to avoid premature egress of BSM) was considered optimal. In fractures for which an “open-book” approach to reduction or those with extensive cortical comminution, alternate defect management strategies were employed. Patient demographic and injury information was recorded. Clinic notes were reviewed for clinical information and complications. We identified all-cause reoperation, superficial infection (requiring antibiotics), deep infection (requiring surgical debridement), and nonunion.
Procedure
After open reduction internal fixation was performed according to the surgeons’ standard techniques, the defect was assessed for use of the fenestrated delivery system. The fenestrated screw is ideally placed through the bone defect. The screw cannot be placed through a plate at this time. For use in the proximal tibia, 4.0 mm screws was chosen in all cases. A 1.2 mm guidewire was placed in the desired location and assessed fluoroscopically. The desired screw length was measured, and the pilot for the screw was drilled over the wire. The injection system consists of an interlocking cannulated system; the first cannula was threaded onto the head of the screw prior to insertion which was then inserted until the cannula was flush with the bone. At this point, the BSM was mixed according to the manufacturer’s specifications. The second injection cannula was then threaded into the previously inserted cannula: screw construct, allowing for injection of BSM under fluoroscopic control. Once the BSM was fully injected, both cannulas were removed and the screw was fully seated flush with the cortex (Supplemental Fig. 1). No other bone graft was used. The joint was inspected via direct visualization for extravasation of the cement, though none was observed. Closure then proceeded according to the surgeons’ preferred technique. Patients were kept non-weight bearing for 12 weeks according to the surgeons’ typical protocol. No patients underwent arthroscopy postoperatively to evaluate for cement extravasation. Unlimited range of motion was permitted except with associated tubercle fractures.
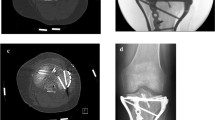
Radiographs obtained immediately post-operative and at final follow-up were used to identify articular subsidence. Subsidence was determined as a change in articular height relative to the medial plateau > 2 mm or a change in height of the articular surface relative to the proximal aspect of the plate of > 2 mm. A single positive criterion was sufficient to qualify as subsidence. Measurements were performed on a picture archiving and communication system (PACS) (Synapse, Fujifilm, Tokyo, Japan, and AGFA Impax, Agfa-Gevaert, Mortsel, Belgium) by an orthopaedic traumatology fellow (AT) and senior resident (DD) in previously described methodology [15]. A sample measurement is shown in Fig. 1.
Representative images for measures of height relative to the medial plateau and height of plate AP XR of the right knee demonstrating the method of measurement for a Height relative to the medial plateau and b height related to plate. These measurements were used to calculate subsidence with > 2 mm qualifying as a patient with subsidence
Statistics
Statistics were performed using SPSS software (IBM, Armonk, NY) and Prism GraphPad (Graphpad Software, La Jolla, CA). We utilized a Student’s t-test for continuous variables. A Fisher’s exact test was used to compare categorical variables. Univariate and multivariate analysis was performed. Significance was placed at p < 0.05.
Results
34 patients were included in this study. The mean age of the patients was 54.06 ± 14.57 years. There were 19 (55%) women. Mean body mass index (BMI) was 28.11 ± 9.88. The average time to surgery was 14.19 ± 14.16 days. Five patients (15%) had a meniscal injury in addition to their tibial plateau fracture that was repaired at the time of surgery. Medical comorbidities included osteoporosis (n = 2, 6%), tobacco use (n = 9, 21%), diabetes mellitus (n = 6, 18%), renal disease or chronic kidney disease (n = 3, 9%), anxiety (n = 3, 9%), and depression (n = 2, 6%). Demographic information is available in Table 1.
The most common mechanism of injury (Supplemental Table 1) was fall from height (n = 9, 26%), followed by pedestrian struck by auto (n = 8, 24%). All fractures were classified according to the Schatzker and OTA/AO classification systems [17, 18]. The predominant fracture types were Schatzker II (n = 15, 44%) and 41B3 (n = 15, 44%). A full analysis of fracture type is available in Supplemental Table 1. There were no open fractures.
Mean follow-up was 32.03 ± 22.52 weeks. Average time to weight bearing was 11.72 ± 2.67 weeks (Table 2). Mean overall height relative to the medial plateau postoperatively was 2.25 ± 2.05 mm (Fig. 2). At final follow-up, it was 1.86 ± 2.01 mm (change of 0.39 ± 1.43 mm) (Fig. 2c, d). The mean articular height relative to the plate was 4.42 ± 3.19 mm post-operative and 3.25 ± 3.41 mm at final follow-up (change of 1.16 ± 2.38 mm). There was no significant difference between mean post-operative and final values for either measurement (p = 0.88 and 0.19, respectively). Average range of motion at most recent follow-up (n = 18) was 119° ± 17.4°.
Representative Images and overall measures of subsidence for patients receiving N-force screw. a Injury, post-operative and follow-up AP images of patient who received N-force screw and did not suffer from subsidence. b Injury, post-operative, and follow-up AP images of patient who received N-force screw and suffered from subsidence. c Mean height relative to the medial plateau for patients immediately post-operative and at most recent follow-up for patients treated with N-force (p > 0.05). d Mean height of the plate for patients immediately post-operative and at most recent follow-up for patients treated with N-force (p > 0.05)
Overall, six patients (15.2%) underwent reoperation (Table 2). Reasons included two (6%) manipulations under anaesthesia due to arthrofibrosis and four debridements for deep infection. There were six (19%) total infections; two were superficial and required solely antibiotics. One of the operative treated patients had implant removal during secondary surgery due to infection. One patient had early failure. Two patients (5.9%) had articular subsidence at 11 and 24 weeks postoperatively. Figure 2 shows representative AP radiographs of patients with no measurable subsidence (A), and a patient with subsidence (B). A summary of patients with subsidence is found in Table 3.
Discussion
The rate of articular subsidence for a wide variety of tibial plateau fractures treated with a novel fenestrated screw for the delivery of CaPO4 BSM was 5.9%. This rate is superior to a large randomized-controlled trial by Russell et al. that reported 9% subsidence in 69 patients with a similar variety of fracture types. However, as a prospective trial, they excluded patients with diabetes and other comorbidities, while we included all patients who had been treated with this device. Similar exclusion criteria would put our rate at 3.4% (1/29).
More recent studies have reported lower rates. A 2014 study of Schatzker II fractures reported no subsidence in 77 patients [15]. A second study in 2017 reported 3.4% subsidence (1/29) across fracture types but was a single-centre, single-surgeon cohort [11]. Comparison among these studies is challenging owing to the different BSM used. We also utilized very strict criteria for subsidence while many studies only used one measurement or grading technique.
It is important to identify the BSM used in these studies, as each has different mechanical properties and compressive strength. The BSM in this study (N-Force Blue, Zimmer Biomet, Warsaw, IN) is designed specifically to be inserted through the N-force fenestrated screw. As such it has unique flow properties but lower compressive strength (7–9 MPa) compared even to other BSM from the same manufacturer (28–42 MPa). This suggests that perhaps other properties besides compressive strength such as flow, volume, percentage fill of the defect, or administration technique may play a part in preventing subsidence. Further study should attempt to characterize how these factors may influence success.
The complication rate in our study was comparable to previously published rates, which range between 2 and 23.6% [19,20,21,22,23]. We report a mix of superficial (n = 2) and deep/operative (n = 4) infections, and of these superficial and deep infections only one required implant removal. Only one patient in our cohort went on to delayed union and this was likely due to several medical comorbidities known to limit the healing process (diabetes mellitus, chronic kidney disease with end organ damage). This nonunion rate of 3% is within the range reported (0–10%) [19, 22, 24, 25]. Studies have shown a range of 0–20% [10, 19, 21, 22, 24] of tibial plateaus require reoperation for reasons such as infection, malalignment, or arthrofibrosis. With our limited cohort, our study results were comparable with previous investigations.
The strengths of this study include that this was a series of patients with a wide variety of fracture types and comorbidities making the results generalizable. Additionally, this series includes the surgeons’ initial cases using this system suggesting that this system may have a short learning curve as indicated by our low rate of subsidence. Additionally, a strict criterion for subsidence was used.
There are several limitations to the study. It was a retrospective review and therefore subject to selection bias as the decision to use this delivery system was made at the discretion of the treating surgeons, and the use of the screws was heterogenous varying the exact number and location of the screws. Therefore, patients who may have been ideal candidates, presented problematic scenarios, or benefited from a particular construct may not have been included, which may limit generalizability of the findings. The radiographs were not taken with magnification correction or according to a specified protocol, which may have masked smaller differences, and accounts for the mean subsidence being less in the final post-operative radiographs than initial. However, we compared radiographs taken within the same institutions with similar protocols in all settings with relatively consistent values suggesting that there was little change between initial and final follow-up. Additionally, we did not use advanced imaging in the post-operative period to assess proper placement within the subchondral defect, or subsequent subsidence. This study was underpowered for one of the outcome measures. A post hoc power analysis revealed that 165 patients would be needed to detect a 2 mm difference in height relative to the medial plateau when comparing pre- and post-operative subsidence, which was not feasible in this early cohort. Additionally, this new technology has the potential for increased cost to standard methods. Lastly, we were unable to obtain functional outcome data from most patients, which would be valuable in assessing true long-term clinical outcomes.
Conclusion
Use of a novel fenestrated screw system for the delivery of CaPO4 BSM results in subsidence and complication rates similar to previously published values and appears to be a viable option for addressing subchondral defects in tibial plateau fractures.
References
Elsoe R, Larsen P, Nielsen NPH et al (2015) Population-based epidemiology of tibial plateau fractures. Orthopedics 38:e780–e786
Court-Brown CM, Caesar B (2006) Epidemiology of adult fractures: a review. Injury 37:691–697
Biyani A, Reddy NS, Chaudhury J et al (1995) The results of surgical management of displaced tibial plateau fractures in the elderly. Injury 26:291–297
Nusselt T, Hofmann A, Wachtlin D et al (2014) CERAMENT treatment of fracture defects (CERTiFy): protocol for a prospective, multicenter, randomized study investigating the use of CERAMENTTM BONE VOID FILLER in tibial plateau fractures. Trials 15:75
Iundusi R, Gasbarra E, D’Arienzo M et al (2015) Augmentation of tibial plateau fractures with an injectable bone substitute: CERAMENTTM. Three year follow-up from a prospective study. BMC Musculoskelet Disord 16:115
Goff T, Kanakaris NK, Giannoudis PV (2013) Use of bone graft substitutes in the management of tibial plateau fractures. Injury 44(Suppl 1):S86-94
Trenholm A, Landry S, McLaughlin K et al (2005) Comparative fixation of tibial plateau fractures using alpha-BSM, a calcium phosphate cement, versus cancellous bone graft. J Orthop Trauma 19:698–702
Welch RD, Zhang H, Bronson DG (2003) Experimental tibial plateau fractures augmented with calcium phosphate cement or autologous bone graft. J Bone Joint Surg Am 85:222–231
McDonald E, Chu T, Tufaga M et al (2011) Tibial plateau fracture repairs augmented with calcium phosphate cement have higher in situ fatigue strength than those with autograft. J Orthop Trauma 25:90–95
TA Russel, RKLeighton, Alpha-BSM Tibial Plateau Fracture Study Group (2008) Comparison of autogenous bone graft and endothermic calcium phosphate cement for defect augmentation in tibial plateau fractures. A multicenter, prospective, randomized study. J Bone Joint Surg Am 90:2057–2061
Oh CW, Park KC, Jo YH (2017) Evaluating augmentation with calcium phosphate cement (chronOS Inject) for bone defects after internal fixation of proximal tibial fractures: a prospective, multicenter, observational study. Orthop Traumatol Surg Res 103:105–109
Ollivier M, Bulaïd Y, Jacquet C et al (2018) Fixation augmentation using calcium-phosphate bone substitute improves outcomes of complex tibial plateau fractures. A matched, cohort study. Int Orthop 42:2915–2923
Bajammal SS, Zlowodzki M, Lelwica A et al (2008) The use of calcium phosphate bone cement in fracture treatment. A meta-analysis of randomized trials. J Bone Joint Surg Am 90:1186–1196
Oztürkmen Y, Caniklioğlu M, Karamehmetoğlu M, Sükür E (2010) Calcium phosphate cement augmentation in the treatment of depressed tibial plateau fractures with open reduction and internal fixation. Acta Orthop Traumatol Turc 44:262–269
Berkes MB, Little MTM, Schottel PC et al (2014) Outcomes of Schatzker II tibial plateau fracture open reduction internal fixation using structural bone allograft. J Orthop Trauma 28:97–102
Ryf C, Goldhahn S, Radziejowski M et al (2009) A New Injectable Brushite Cement: First Results in Distal Radius and Proximal Tibia Fractures. Eur J Trauma Emerg Surg 35:389–396
Schatzker J, McBroom R, Bruce D (1979) The tibial plateau fracture. The Toronto experience 1968–1975. Clin Orthop Relat Res. (138):94–104
Marsh JL, Slongo TF, Agel J et al (2007) Fracture and dislocation classification compendium - 2007: orthopaedic trauma association classification, database and outcomes committee. J Orthop Trauma 21:S1-133
Ruffolo MR, Gettys FK, Montijo HE et al (2015) Complications of high-energy bicondylar tibial plateau fractures treated with dual plating through 2 incisions. J Orthop Trauma 29:85–90
Shah SN, Karunakar MA (2007) Early wound complications after operative treatment of high energy tibial plateau fractures through two incisions. Bull NYU Hosp Jt Dis 65:115–119
Khatri K, Sharma V, Goyal D, Farooque K (2016) Complications in the management of closed high-energy proximal tibial plateau fractures. Chin J Traumatol 19:342–347
Morris BJ, Unger RZ, Archer KR et al (2013) Risk factors of infection after ORIF of bicondylar tibial plateau fractures. J Orthop Trauma 27:e196-200
Colman M, Wright A, Gruen G et al (2013) Prolonged operative time increases infection rate in tibial plateau fractures. Injury 44:249–252
Kugelman D, Qatu A, Haglin J et al (2017) Complications and unplanned outcomes following operative treatment of tibial plateau fractures. Injury 48:2221–2229
Weiner LS, Kelley M, Yang E et al (1995) The use of combination internal fixation and hybrid external fixation in severe proximal tibia fractures. J Orthop Trauma 9:244–250
Funding
There were no sources of funding for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
G. S. Marecek has received research support funding from BoneSupport AB and is a paid consultant for DePuy Synthes Globus Medical, Nuvasive, Stryker, Smith & Nephew, and Zimmer Biomet. G.S. Marecek is a committee member for the Orthopaedic Trauma Association and Western Orthopaedic Association. Donald Desanto has stock or stock options in AbbVie, Amgen Co, Becton Dickinson, and Company, Cardinal Health, Inc., Celgene, Hill-Rom Holdings, Inc., Johnson & Johnson, Masimo, Norvartis, Procter & Gamble, Sangam Therapeutics, Shockwave Medical, and Stryker. John Scolaro is a paid consultant for Globus Medical, Nuvasive, Smith & Nephew, Stryker, and Zimmer Biomet. John Scolaro receives IP royalties from Globus Medical. Alexander Telis, Edward Compton, Douglass Tucker, John Carney, and Adam K. Lee have no competing interests.
Ethical approval
This study received no outside funding and was initiated following after Institutional Review Board (IRB) approval.
Human and animal rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
As this study included human subjects informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Telis, A.L., Tucker, D.W., Compton, E. et al. Treatment of tibial plateau fractures with a novel fenestrated screw system for delivery of bone graft substitute. Eur J Orthop Surg Traumatol 31, 1321–1327 (2021). https://doi.org/10.1007/s00590-021-02871-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-021-02871-y