Abstract
Introduction
This study examined whether the component position or muscle strength affects the cup-head translation under in vivo weight-bearing conditions after total hip arthroplasty (THA). We hypothesized that there was a correlation between the hip offset or abductor strength and cup-head translation during gait.
Materials and methods
We prospectively evaluated 31 patients undergoing unilateral cementless primary THA. The cup height, cup/stem offset, and limb length discrepancy were measured on anterior–posterior bilateral hip radiographic images. The isometric muscle strength of the lower limbs was quantified using a handheld dynamometer. Continuous radiographic images were recorded during gait, and cup-head translation was analysed using a computer-assisted method.
Results
The average cup height, cup/stem offset, and limb length discrepancy were − 3.8 ± 5.1 mm, 1.2 ± 5.2 mm/− 0.7 ± 7.7 mm, and − 2.1 ± 5.2 mm, respectively. The average hip abductor/flexor and knee extensor strength were 86% ± 18%/85% ± 17% and 88% ± 17% of the contralateral healthy hip, respectively. The average cup-head translation during swing phase of gait was − 0.003 ± 0.31 mm. Multiple regression analyses found no significant independent predictors of cup-head translation (p > 0.05).
Conclusions
The component position or muscle strength did not significantly influence cup-head translation during gait after well-positioned primary THA.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Total hip arthroplasty (THA) has become one of the most successful orthopaedic interventions for eliminating pain and improving the function during daily activity in patients with hip osteoarthritis (OA) [1]. Because of the improvements in the fabricated materials and surgical techniques, the long-term follow-up outcomes after THA have steadily improved [2]. However, revision surgery due to polyethylene liner wear, fracture, component loosening, and recurrent dislocation can still occur [3].
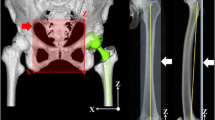
Interest in the cup-head separation accelerating liner wear in superior lateral rim due to edge loading and piston effect [4, 5] has recently risen. Dennis et al. [6] previously described significant cup-head translation of 3.3 mm on average during active hip abduction. In contrast, Tsai et al. [7] reported that cup-head translation was less than 1 mm during gait in all 28 patients evaluated. No clear trend has emerged from the literature [6, 7] regarding cup-head translation (Fig. 1) during in vivo activities. Several factors, including the component position, limb length discrepancy, muscle strength, and soft tissue tension around the hip joint, may be associated with the cup-head translation [3,4,5, 8, 9]. However, data concerning the effect of component position and muscle strength on cup-head translation are limited.
Therefore, we prospectively evaluated whether or not the component position and muscle strength are significantly correlated with cup-head translation under in vivo weight-bearing activities after primary posterolateral THA. We hypothesized that there was a correlation between the hip offset or abductor strength and cup-head translation during swing phase of gait.
Materials and methods
Subjects
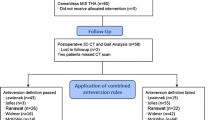
Patients who underwent primary THA at our institution between January 2012 and October 2016 were prospectively recruited for the study and provided preoperatively their written consent to participate in this institutional review board-approved study (#24-15). Patients who had functional abnormality or osteoarthritis in contralateral hips were excluded from the study. Patients with any history of previous arthroplasty and osteotomy, fracture around the hip joint, severe extra-articular deformity, and neuromuscular disease were also excluded. This prospective cohort involved 31 patients with 31 hips requiring unilateral THA. The reason for surgery was OA in 25 hips, including 13 hips with developmental dysplasia of the hip (DDH) as defined by a lateral centre–edge angle of Wiberg < 20° [10] (Crowe classification [11] type I, 10 hips; type II, 2 hips; type III, 1 hip), and osteonecrosis of the femoral head in 6 hips. The patient information is summarized in Table 1.
Implants and surgical techniques
A cementless stem, cementless acetabular cup, and 32-mm alumina ceramic femoral head on annealed crosslinked polyethylene (XLPE) acetabular liner (Kyocera PerFix 910 stem, AMS cup, and Aeonian liner; Kyocera Medical Corp., Osaka, Japan) were used in all 31 hips [2]. The radius of the ball-in-cup clearance was 0.2 mm. All THAs were performed by two senior hip surgeons using a posterolateral approach [12]. Intraoperative anterior–posterior (AP) radiographs were used to optimize the component position and limb length. The posterior soft tissues, including the piriformis muscle, obturator internus, superior gemellus, and posterior capsule, were routinely repaired in separate layers [12].
Measurement of component position
The cup height, cup/stem offset, global hip offset, length change in the operated limb, and limb length discrepancy were evaluated on AP bilateral hip radiographic image using the SYNAPSE PACS system (Fujifilm Medical Corp., Ltd., Tokyo, Japan) [13, 14] (Fig. 2). The horizontal line between the inferior aspects of both pelvic teardrops was drawn, after which a line perpendicular to the previous line was drawn at the bottom edge of the tear drop. The cup offset/height was measured as the distance between the centre of the femoral head and horizontal/vertical line. The stem offset was measured as the distance between the femoral head centre and longitudinal axis of the proximal third of the femur. Then the global hip offset was calculated by adding the cup offset to the stem offset. The limb length discrepancy was defined as the perpendicular distance between the lesser trochanters and a horizontal reference line connecting the inferior aspect of the acetabular teardrop [15]. All measurements were calculated by subtracting the measurements of the contralateral healthy hip from those of the replaced hip. Regarding the cup height and cup/stem offset, ‘plus’ values meant that the replaced hip was higher and larger than the contralateral healthy hip.
The cup offset (A), cup height (B), stem offset (C), global hip offset (A + C) in the replaced hip relative to the contralateral healthy hip (A’, B’, C’, and A’ + C’, respectively), and limb length discrepancy (D − D’) were measured using anteroposterior bilateral hip radiographic image. The continuous line is the horizontal reference line between the inferior aspects of pelvic teardrops. The small dotted line is perpendicular to the reference line at the bottom edge of the teardrop. The large dotted line is the longitudinal axis of the proximal third of the femur
Measurement of the muscle strength
Hip abductor, hip flexor, and knee extensor strength in the replaced and contralateral healthy hips were quantified using a handheld dynamometer (HHD; Anima Co., μ-TasF1, Tokyo, Japan) [14, 16] by well-trained physiotherapists at our institute who had an experience of more than a year in moment testing [14] (Fig. 3). During measurement of the hip abductor strength, patients were laid in the supine position with the hip and knee in a neutral position. A force sensor was placed 5 cm proximal to the lateral epicondyle of the femur. During measurement of the hip flexor and knee extensor strengths, patients were placed in a seated position, with straps across the waist and thighs for stabilization. Two trials were performed after one practice in all examinations, with the highest peak torque used for the analysis. The torque was obtained by multiplying the strength by the lever arm and expressed as a percentage of body weight (Nm/kg), and the percentage of the muscle strength in the replaced hip relative to the contralateral healthy hip was calculated.
Measurement of cup-head translation
Continuous AP radiographic images during gait were recorded at 3.5 frames/s using a flat-panel X-ray detector (Ultimax-I, Toshiba, Tochigi, Japan), with an image area of 420 mm (H) × 420 mm (V) and a resolution of 0.274 mm × 0.274 mm/pixel, 0.02 s pulse width, 80 kV, and 360 mA (Fig. 4). For gait, patients walked on a level treadmill at 1.0 km/h. The cup-head translation was obtained by using a computer-assisted method with a measurement software program (PolyWare, Draftware Developers, Vevay, IN, USA), for which the accuracy was 0.022–0.335 mm for the two-dimensional vector [17]. The program identified the centres of the cup and femoral head via an edge detection method and calculated the cup-head translation as the mid-swing phase relative to the stance phase during gait. ‘Plus’ values meant lateral, below, and posterior translations of the head relative to the cup in the out, down, and back vectors, respectively (Fig. 5). The inter- and intra-observer reliabilities evaluated by two independent observers at an interval of more than 1 month were 0.97 and 0.91, respectively, indicating that the measurement had excellent reliability [18].
Statistical analyses
Statistical analyses were performed using the JMP 13.0.0 software program (SAS Institute Inc., Cary, NC, USA). A paired t test was used to evaluate differences in global hip offset and limb length discrepancies between pre- and postoperative THAs. Single regression analyses and a multiple regression analysis using a stepwise variable entry method were performed to evaluate the factors associated with the cup-head translation. Demographic data (gender, age, body mass index [BMI], and diagnosis), radiographic data (cup height, cup offset, stem offset, length change in the operated limb, and limb length discrepancy), and clinical data (hip abductor, hip flexor, and knee extensor strength) were used in the linear regression analyses and multivariate logistic regression model. For all statistical analyses, a significant difference was defined as a p value < 0.05.
Results
The average cup height, cup offset, and stem offset in the replaced hip relative to the contralateral healthy hip were − 3.8 ± 5.1 mm (range − 15.2–5.1 mm), 1.2 ± 5.2 mm (range − 7.8–10.6 mm), and − 0.7 ± 7.7 mm (range − 15.9–15.6 mm), respectively. The average pre- and postoperative global hip offset discrepancies were 0.3 ± 6.2 mm (range − 7.4–15.8 mm) and − 0.5 ± 10.7 mm (range − 23.7–25.8 mm), respectively, without significant difference (p = 0.92). The average length change in the operated limb was 9.0 ± 8.1 mm (range − 5.5–34.4 mm). Compared to preoperative conditions, the average limb length discrepancy was significantly (p < 0.001) improved from − 11.2 ± 9.5 mm (range − 44.6–0.9 mm) to − 2.1 ± 5.2 mm (range − 15.2–8.3 mm).
The muscle strength in the replaced hip was 0.68 ± 0.25 Nm/Kg (range 0.16–1.25 Nm/Kg), 0.79 ± 0.25 Nm/Kg (range 0.14–1.30 Nm/Kg), and 0.96 ± 0.34 Nm/Kg (range 0.26–1.73 Nm/Kg) for hip abduction, hip flexion, and knee extension, respectively. The percentage of the muscle strength in the replaced hip relative to the contralateral healthy hip was 86% ± 18% (range 45–123%), 85% ± 17% (range 55–130%), and 88% ± 17% (range 49–118%) for hip abduction, hip flexion, and knee extension, respectively.
The average cup-head translation at mid-swing relative to the stance phase of gait was − 0.003 ± 0.31 mm (range − 0.74 to 0.62 mm). The average cup-head translations for the out, down, and back directions were − 0.08 ± 0.33 mm (range − 0.76 to 0.60 mm), 0.04 ± 0.27 mm (range − 0.48 to 0.52 mm), and − 0.04 ± 0.15 mm (range − 0.43 to 0.22 mm), respectively. There was no significant difference in each direction of cup-head translation (p > 0.05).
The single regression analyses assessing the sex, age, BMI, diagnosis, cup height, cup offset, stem offset, limb length discrepancy, hip abductor strength, hip flexor strength, and knee extensor strength showed no statistically significant correlation with cup-head translation (Table 2). The multiple regression analysis showed that there was no significant independent predictor of cup-head translation (Table 3).
Discussion
The most remarkable finding in this prospective study was that the component position and muscle strength had no significant relationship with cup-head translation after unilateral primary THA. The cup-head translation was − 0.003 ± 0.31 mm on average, with less than 1 mm of maximum translation during gait. A posterolateral approach with capsular and short external rotator repair produces sufficient stability without significant cup-head translation under dynamic conditions.
The average cup-head translation was − 0.003 ± 0.31 mm during swing phase of gait. None of the subjects in the present series had a marked cup-head translation of more than 1 mm. The results of this study differed from those in a previous report by Komistek et al. [9], but supported the findings by Tsai et al. [7]. Komistek et al. reported that all ten of their subjects with a metal-on-polyethylene implant had femoral head sliding of 2.0 mm on average during swing phase of gait. The fact that surface separation occurs is not surprising when considering joint laxity and instability. However, preventing significant separation is an important issue to address in order to avoid excessive stress on the polyethylene liner, which affects the longevity of the prosthesis and the clinical results [4,5,6]. Tsai et al. [7] reported that no hip translation larger than 0.72 mm was observed in any of the 28 cases of primary THA during gait, which is consistent with the results of our study. In our series, the radius of ball-in-cup clearance at the implanted components was manufactured to be 0.2 mm. Furthermore, the creep deformity of annealed XLPE was reported to be 0.23 mm on average [19]. In addition, the measurement software program accounted for a certain degree of error, with the accuracy ranging from 0.022 to 0.335 mm [17]. Taking these matters into account, primary THA using a posterolateral approach appears able to produce sufficient stability without significant cup-head translation during gait.
Joint stability is based on a combination of factors, such as the component position, limb length, muscle strength, and soft tissue tension around the replaced hip joint [8, 20,21,22]. However, few in vivo studies have evaluated the relationship between cup-head translation and the cup/stem offset, limb length discrepancy, or abductor/quadriceps muscle strength. A previous in vitro study using a theoretical forward solution mathematical model of the hip demonstrated that 1 cm of cup medialization caused approximately 2.5 mm of cup-head separation [21]. In the current in vivo series, cup medialization of more than 1 cm (maximum: 10.2 mm) in some outliers (2 hips: 6%) could be compensated for by dynamic muscle forces to provide hip stability during gait. None of the subjects had more than 2.5 cm of global hip offset discrepancy in the replaced hip relative to the contralateral healthy hip without significant difference to preoperative conditions. We usually aim for the same leg length on the replaced and healthy contralateral hips, and use a high-offset stem in most of the cases to keep preoperative global offset [14]. The postoperative limb length discrepancy: − 2.1 mm on average, was significantly improved compared to preoperative conditions: − 11.2 mm on average.
In this study, hip abductor, hip flexor, and knee extensor strength of the replaced hip recovered to 85–88% of the healthy contralateral strength at an average age of 8 months after THA. Postoperatively, 10–15% muscular weakness in the lower extremities has been reported at 6 to 24 months after THA [14, 23, 24]. Kamimura et al. [16] reported hip abductor, extensors, and knee extensors strength of the operated limb of 0.51 Nm/kg, 0.59 Nm/kg, and 0.8 Nm/kg in 48 Asian females with an average age of 67 years. Our values of hip abductor, extensors, and knee extensors strength: 0.68 Nm/Kg, 0.79 Nm/Kg, and 0.96 Nm/Kg in 11 Asian males and 21 Asian females with an average of 68.0 years, are comparable to these values. A proper hip offset and limb length contribute to the hip joint stability and abductor strength [14, 22], helping prevent significant cup-head translation under dynamic conditions.
Glaser et al. [20] reported that minimally invasive THA was able to reduce cup-head translation while walking on a treadmill due to the preserved soft tissue around the hip joint compared with traditional posterolateral THA. Tsai et al. [7] examined a total of 28 metal-on-polyethylene THAs without significant cup-head translation, but did not mention their applied surgical approach. In the current series, there was no significant cup-head translation during gait after primary metal-on-polyethylene THA using a posterolateral approach with capsular and short external rotator repair. These data suggest that, regardless of the surgical approach, ensuring an appropriate component position and soft tissue tension may prevent significant cup-head translation after THA during weight-bearing activities.
There are some limitations associated with this current study. First, the study was limited by the small number of patients. A wider variation in postoperative alignment and laxity may thus provide more robust results. However, the number of subjects is similar to previous fluoroscopic studies that have analysed ten or 28 THAs [6, 7, 9, 20]. Second, cup-head translation was evaluated only during gait cycle. Gait is one of the most important functions for many activities of daily living. However, a further study of daily activities, such as squatting, chair-rising, and pivoting motion, should be conducted. Finally, we were unable to estimate the precise surface separation between the polyethylene liner and femoral head because the measurement software program accounted for a certain degree of error and could not estimate the precise shape of the liner surface after creep deformity. However, the cup-head translation examined in this study was an effective index of the femoral head translation inside the polyethylene liner instead of cup-head separation. None of the above limitations and uncertainties bias our measurements or results, which indicate no significant relationship with the component position or muscle strength, and cup-head translation during gait.
In conclusion, a posterolateral approach with capsular and short external rotator repair provided sufficient stability between the cup and femoral head during gait after unilateral primary metal-on-polyethylene THA. The present finding provides baseline data for comparing outliers, such as malpositioned components and recurrent dislocation, in future studies.
References
Learmonth ID, Young C, Rorabeck C (2007) The operation of the century: total hip replacement. Lancet 370(9597):1508–1519
Nakashima Y, Sato T, Yamamoto T, Motomura G, Ohishi M, Hamai S et al (2013) Results at a minimum of 10 years of follow-up for AMS and PerFix HA-coated cementless total hip arthroplasty: impact of cross-linked polyethylene on implant longevity. J Orthop Sci 18(6):962–968
Hua X, Li J, Wang L, Jin Z, Wilcox R, Fisher J (2014) Contact mechanics of modular metal-on-polyethylene total hip replacement under adverse edge loading conditions. J Biomech 47(13):3303–3309
Blumenfeld TJ, Glaser DA, Bargar WL, Langston GD, Mahfouz MR, Komistek RD (2011) In vivo assessment of total hip femoral head separation from the acetabular cup during 4 common daily activities. Orthopedics 34(6):127
Harris WH (2012) Edge loading has a paradoxical effect on wear in metal-on-polyethylene total hip arthroplasties. Clin Orthop Relat Res 470(11):3077–3082
Dennis DA, Komistek RD, Northcut EJ, Ochoa JA, Ritchie A (2001) “In vivo” determination of hip joint separation and the forces generated due to impact loading conditions. J Biomech 34(5):623–629
Tsai TY, Li JS, Wang S, Scarborough D, Kwon YM (2014) In-vivo 6 degrees-of-freedom kinematics of metal-on-polyethylene total hip arthroplasty during gait. J Biomech 47(7):1572–1576
Elkins JM, Kruger KM, Pedersen DR, Callaghan JJ, Brown TD (2012) Edge-loading severity as a function of cup lip radius in metal-on-metal total hips—a finite element analysis. J Orthop Res 30(2):169–177
Komistek RD, Dennis DA, Ochoa JA, Haas BD, Hammill C (2002) In vivo comparison of hip separation after metal-on-metal or metal-on-polyethylene total hip arthroplasty. J Bone Joint Surg Am 84-A(10):1836–1841
Wiberg G (1939) Studies on dysplastic acetabula and congenital subluxation of the hip joint with special reference to the complication of osteoarthritis. Acta Chir Scand 83(Suppl 58):5–135
Crowe JF, Mani VJ, Ranawat CS (1979) Total hip replacement in congenital dislocation and dysplasia of the hip. J Bone Joint Surg Am 61(1):15–23
Nakashima Y, Hirata M, Akiyama M, Itokawa T, Yamamoto T, Motomura G et al (2014) Combined anteversion technique reduced the dislocation in cementless total hip arthroplasty. Int Orthop 38(1):27–32
Dastane M, Dorr LD, Tarwala R, Wan Z (2011) Hip offset in total hip arthroplasty: quantitative measurement with navigation. Clin Orthop Relat Res 469(2):429–436
Fukushi JI, Kawano I, Motomura G et al (2018) Does hip center location affect the recovery of abductor moment after total hip arthroplasty? Orthop Traumatol Surg Res 104(8):1149–1153
Lim YW, Huddleston JI 3rd, Goodman SB, Maloney WJ, Amanatullah DF (2018) Proximal femoral shape changes the risk of a leg length discrepancy after primary total hip arthroplasty. J Arthroplasty 33(12):3699–3703
Kamimura A, Sakakima H, Tsutsumi F, Sunahara N (2014) Preoperative predictors of ambulation ability at different time points after total hip arthroplasty in patients with osteoarthritis. Rehabil Res Pract 2014(861268):1–7
Stilling M, Kold S, de Raedt S, Andersen NT, Rahbek O, Soballe K (2012) Superior accuracy of model-based radiostereometric analysis for measurement of polyethylene wear: a phantom study. Bone Joint Res 1(8):180–191
Sato T, Nakashima Y, Akiyama M, Yamamoto T, Mawatari T, Itokawa T et al (2012) Wear resistant performance of highly cross-linked and annealed ultra-high molecular weight polyethylene against ceramic heads in total hip arthroplasty. J Orthop Res 30(12):2031–2037
Hamai S, Nakashima Y, Mashima N, Yamamoto T, Kamada T, Motomura G et al (2016) Comparison of 10-year clinical wear of annealed and remelted highly cross-linked polyethylene: a propensity-matched cohort study. J Mech Behav Biomed Mater 59:99–107
Glaser D, Dennis DA, Komistek RD, Miner TM (2008) In vivo comparison of hip mechanics for minimally invasive versus traditional total hip arthroplasty. Clin Biomech (Bristol, Avon) 23(2):127–134
Komistek RD, LaCour MT, Sharma A (2015) Proceedings of 2nd annual Pan Pacific orthopaedic congress; 22–25 July; Kona, the Big Island. Hwaii, USA. Conference supplement
Ogawa T, Takao M, Hamada H, Sakai T, Sugano N (2018) Soft tissue tension is four times lower in the unstable primary total hip arthroplasty. Int Orthop, Mar 27
Rasch A, Dalen N, Berg HE (2010) Muscle strength, gait, and balance in 20 patients with hip osteoarthritis followed for 2 years after THA. Acta Orthop 81:183–188
Judd DL, Dennis DA, Thomas AC et al (2014) Muscle strength and functional recovery during the first year after THA. Clin Orthop Relat Res 472:654–664
Harris WH (1969) Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am 51(4):737–755
Acknowledgements
Source of funding: This work was supported by JSPS KAKENHI Grant No. (25870499) and a grant from the Nakatomi Foundation.
Funding
This study was funded by JSPS KAKENHI Grant No. (25870499) and a grant from the Nakatomi Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kiyohara, M., Hamai, S., Hara, D. et al. Do component position and muscle strength affect the cup-head translation during gait after total hip arthroplasty?. Eur J Orthop Surg Traumatol 29, 1263–1269 (2019). https://doi.org/10.1007/s00590-019-02443-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-019-02443-1