Abstract
Background
Intertrochanteric fractures are of great interest worldwide and are the most frequently operated fractures. Intramedullary nailing is commonly used in the treatment of intertrochanteric fractures. The purpose of this study is to assess the necessity of using the distal blocking screw in 31-A1 and 31-A2 fractures, classified according to the Orthopaedic Trauma Association classification system (AO/OTA).
Methods
This is a prospective study of 143 consecutive patients (mean age 85.01 years, mean final follow-up 14.1 months) surgically treated with the same intramedullary nail. In 75 cases, the distal locking screw was not used. Parameters evaluated during follow-up were: blood loss, transfusion requirements, surgery duration, and fluoroscopy time. Harris Hip Score and Barthel Activity Daily Living were used for the clinical evaluation. Radiographic Union Score For Hip (RUSH score) and Tip apex distance (TAD) were measured for radiologic evaluation.
Results
The group treated without locking screw showed significantly shorter surgical duration time (31.9 vs. 47.2 min), a decrease in blood loss (variation Hb − 1.06 vs. − 1.97), and reduced X-rays exposure time (25.4 vs. 31.6 s). No significant differences were observed in the postoperative period and in the radiographic and clinical scores.
Conclusion
This study demonstrates that in intertrochanteric 31-A1 and 31-A2 stable fractures, the absence of distal locking screw does not compromise bone healing and prevents several clinical complications.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Intertrochanteric fractures are of great interest worldwide and are the most frequently operated fracture. Due to the increase in life expectancy, these fractures are likely to become more frequent in the future [1,2,3]. Over the years, different kinds of surgical treatments such as sliding hip screws or plates and intramedullary nails have been researched and implemented with different outcomes [4]. Osteosynthesis by means of intramedullary nails offers the opportunity to perform minimally invasive surgery causing little damage to the soft tissues. Nevertheless, this kind of surgery has been correlated with some documented complications [5].
In the literature, there is an ongoing debate whether distal locking screws are necessary.
In fact, distal locking screws for axial and/or rotationally unstable fracture patterns have been found to maintain fracture length, prevent limb shortening, and subsequently increase fracture stability and allow early postoperative ambulation [6, 7].
Nevertheless, there are a good number of clinical and biomechanical reports that support intramedullary intertrochanteric fracture fixation without any distal interlocking screws [8, 9].
However, these biomechanical studies did not take into account the dynamic loading conditions, nor the common rotational forces, which represent better the actual clinical scenario of a patient mobilized after fixation.
The purpose of this study is to assess the necessity of using the distal blocking screw in 31-A1 and 31-A2 fractures, according to the AO/OTA classification.
Materials and methods
This prospective non-randomized study included 143 consecutive patients with pertrochanteric fractures operated with the same intramedullary nail (SM Supernail GT, by LIMA®) from January 2014 to January 2015.
This study was conducted in accordance with the ethical guidelines of the Declaration of Helsinki, and informed consent was obtained from all patients.
All the fractures were classified according to the AO/OTA classification system. We included patients with 31-A1 and 31-A2 stable fractures with a preoperative Barthel Activity Daily Living > 15. Exclusion criteria were dementia, patients not walking before trauma, unstable 31-A3 or subtrochanteric fractures, pathological fractures, open fractures, bilateral simultaneous fractures, fractures associated with a neurovascular injury as well as previous ipsilateral hip or femur surgery. Patients with BMI > 30 and with symptomatic anemia (HB < 8) were also excluded. The patients were divided in two different groups: In 68 cases, the distal screw was used (group A: locking), while it was not used in 75 cases (group B: unlocked). All the surgeries were performed by the same surgeon who had considerable experience in this type of procedure. The average final follow-up was 14.1 months (range 12–18). For the clinical evaluation, Barthel Activity Daily Living and Harris Hip Score were used at 6 and 12 weeks after surgery and in the final clinical evaluation. At hospital admission, two standard X-rays of the hip were performed on all the patients. The X-ray examination was repeated at first day after surgery and then at 6 and 12 weeks postoperatively. We divided our observational study in three phases: In the first phase, we assessed blood loss and transfusion requirements pre- and postoperative. In the second phase, we did clinical and radiological examinations at 6 and 12 weeks after surgery.
Patient population
In group A (distal locked nail), there were 68 patients with mean age of 84.5 years (range 63–96). Fifty-seven patients were females and 11 were male; 26 patients had left side injury, while 42 patients had right side involved. According to Orthopaedic Trauma Association classification system (AO/OTA), 38 patients had 31-A1-type injury, while 30 patients had 31-A2 injury. Mean hospital stay was 2.47 days (range 1–6 days).The mean preoperative BMI was 23.93 kg/m2 (range 15.79–29.41 kg/m2), and mean preoperative Hb (hemoglobin) and Ht (hematocrit) were 11.6 g/dl (range 8.8–16.4 g/dl) and 33.81% (range 25.5–47.3%), respectively.
In group B (distal unlocked nail), there were 75 patients with mean age of 85.48 years (range 64–100).There were 62 female and 13 male patients. Thirty-eight patients had left side injury, while 37 had right side fracture. According to Orthopaedic Trauma Association classification system (AO/OTA), 35 patients had 31-A1-type injury, while 40 patients had 31-A2 injury. Mean hospital stay was 2.88 days (range 0–8 days). The mean preoperative BMI was 23.73 kg/m2 (range 19.53–30.41 kg/m2), and mean preoperative Hb (hemoglobin) and Ht (hematocrit) were 11.08 g/dl (range 8–15.4 g/dl) and 33.49% (range 28.7–47.2%), respectively (Table 1).
Follow-up
We evaluated clinical parameters (blood loss and general complications) during hospitalization time. The day after surgery postoperative radiographic examinations were performed for all patients. Clinical and radiographic examinations were repeated at 6 and 12 weeks post-op. Mean follow-up was 14.1 months (range 12–19) for all the cases. At the final follow-up, 41 out of 143 (28.6%) patients were lost: The remaining 102 patients were clinically examined in order to detect possible general clinical complications.
Evaluation scores
For the clinical evaluation, the Barthel Activity Index was used in the preoperatively and then at 6 and 12 weeks postoperatively. All the patients included in this study had a score > 15 (min 15 max 20, mean 18.2). The Harris Hip Score was used at 6 and 12 weeks postoperatively.
X-ray scores
Enrollment required the availability of plain hip X-rays, in AP and lateral views, performed the day after surgery, for a baseline assessment, and subsequently during the follow-up at 6 and 12 weeks postoperatively. The authors utilized the Radiographic Union Score for Hip (RUSH) for follow-up bony union assessment of the fracture [10, 11]. RUSH provides four component scores of cortical bridging, cortical disappearance, trabecular consolidation, and trabecular disappearance. Each component can be scored from 1 to 3 for. Similarly, the two trabecular indexes were scored from 1 to 3 each based on consolidation for one of the indexes and fracture line disappearance for the other. The overall RUSH score therefore ranged from a minimum of 10 to a maximum of 30. Images were reviewed separately, and consensus was achieved at the second evaluation in cases of scoring disagreement. Tip apex distance (TAD) was determined by measuring the distance from the tip of the cephalic screw to the apex of the femoral head on both AP and oblique radiographs and was not normalized on cephalic screw length. All the radiographic assessments were carried out using the software package IMPAX (v. 6.4, Agfa).
Statistical analysis
Statistical analysis was performed with MedCalc Statistical Software version 14.8.1 (MedCalc Software bvba, Ostend, Belgium). We defined statistical significance for a p value < 0.05.
Design of the cephalomedullary nail
All the intramedullary nails were made by a single manufacturer. The Supernail GT Lima nail was the same for all cases: the standard version (length 180 mm). The proximal diameter is 15.5 mm, and the distal diameter is 10 mm. The length of the helical blade ranged from 75 to 120 mm. The caput–collum–diaphysis (CCD) angle of the nail was 125° or 130°. The distal part of the nail contained one oval hole for either dynamic or static locking purposes. In all the cases where the distal screw was used, it was placed dynamically. The length of the cephalic screw ranged from 70 mm to 120 mm, with 10.5 mm of diameter. An anti-rotational screw was inserted to block the cephalic screw. The angle of the intramedullary nail was decided by the surgeon depending on the each patient’s variables such as patient age, fracture type, fracture reduction, quality of bone, and width of the medullar cavity. During surgery, all fractures were treated by closed reduction under C-arm fluoroscopy control.
Surgical technique
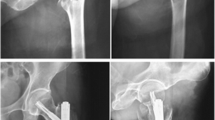
The patient is positioned on the operatory table, and adequate fracture reduction is accomplished while the patient is in the supine position on the fracture table. Through a small incision of 4–5 cm proximal to the greater trochanter, the fascia is incised without dissecting the fibers of the gluteus medius. This approach is designed to minimize soft tissue damage around the proximal femur. A nail system with a targeting guide and a trocar system helps protect the gluteus medius [12]. Choosing the correct nail entry point into the greater trochanter is one of the crucial elements of intramedullary nailing. In most cephalomedullary nails, the guide pin is positioned right at the tip or slightly medial to the tip of the greater trochanter in the AP view. After that, the greater trochanter is drilled at the apex level with a cannulated tip and the guide wire is introduced. A radiographic examination of the two views is recommended. If the guide wire is well positioned, a flexible reamer is used to prepare the femoral canal. After that, the nail is inserted into the femoral canal and the guide wire is removed. A lateral incision on the thigh in line with the anteversion position of the nail guide is performed. At this point, the guide wire cannula is inserted to introduce the cephalic reamer and the cephalic screw is positioned until the apex of the femoral head. It is important to check the correct position of the screw under image intensifier; at this time, it is important to verify the correct tip apex distance (TAD) that should be less than 25 mm in both radiographic views. The cephalic screw should be centered in the neck fragment. If the screw is not centered, flexion and extension of the limb may result in the loosening of the bone–screw interface, and the screw may be subsequently cut out. The cephalic screw is inserted 5 mm deeper than the standard position, without giving a screw compression, in order to allow a dynamic fracture compression during weight bearing. Then, an anti-rotational screw is inserted, to allow the sliding of the cephalic screw, while avoiding its rotatory motion and the subsequent rotation of the femoral head and neck. Sutures of subcutaneous and cutaneous tissue are performed. In group A, we did not use the distal blocking screw, and in group B, a distal dynamic blocking screw was positioned by means of a dedicated kit (Figs. 1, 2, 3).
Postoperative management
The same rehabilitation program was used in both groups. Depending on their general conditions, patients could be put in a sitting position on the first postoperative day. From the second postoperative day, the patients were allowed partial weight bearing, with the help of two crutches and a physiotherapist. After 40 days, ambulation with single crutch was allowed. Suture removal was performed 15 days after surgery.
Results
The gathered results were then classified according to the different categories and separated in groups A and B as follows:
Group A (locked)
Mean postoperative Hb: 9.67 g/dl (range 7.2–15.9 g/dl).
Mean postoperative Ht: 27.99% (range 23.3–39.8%).
Mean transfusion requirements: 2.07 (range 0–6).
Mean surgical case duration: 47.16 min (range 25–90).
Nail angle
-
125° in 29 patients.
-
130° in 39 patients.
Mean cephalic screw length: 93.35 mm (range 85–115).
Mean Harris Hip Score 40 days: 63.23 (range 55–79).
Mean Harris Hip Score 90 days: 81.23 (range 65–90).
Mean Barthel Index 40 days: 15.09 (range 13–18).
Mean Barthel Index 90 days: 17.86 (range 16–20).
Group B (unlocked)
Mean postoperative Hb: 10.02 g/dl (range 8.1–13.1 g/dl).
Mean postoperative Ht: 30.32% (range 24.4–40.1%).
Mean transfusion requirements: 1.33 (range 0–4).
Mean surgical case duration: 31.87 min (range 15–95).
Nail angle
-
125° in 17 patients.
-
130° in 58 patients.
Mean cephalic screw length: 93.25 mm (range 80–115 mm).
Mean Harris Hip Score 40 days: 65.39 (range 60–75).
Mean Harris Hip Score 90 days: 83.55 (range 65–90).
Mean Barthel Index 40 days: 15.09 (range 12–18).
Mean Barthel Index 90 days: 18.04 (range 15–20).
Radiation dose and exposure
For group A, the mean radiation dose was 3.11 mGY with an exposure time of 31.59 s, while for group B the mean radiation dose was 2.90 mGy with an exposure time of 25.40 s. The difference between the two groups was significant (p < 0.005).
Radiographic results
Median RUSH showed a strong statistical increase between the 6th and 12th week follow-up in both groups with a mean value of 20.66 and 24.31 and 20.83 and 23.78, respectively, in group A (p < 0.0001) and group B (p = 0.0002).
Furthermore, the mean RUSH score at 40 and 100 days post-op did not reveal any significant difference between the two groups. TAD variation between the groups was similar during the follow-up.
Complications
At the final follow-up, we reported two cases (2 of 68, 2.9%) of cephalic screw cutout and two cases (2 of 68, 2.9%) of diaphyseal fractures around the distal part of the nail, both in group A, while no cases of cutout were observed in the unlocked group. In group B, we reported one case of subtrochanteric fracture after osteosynthesis with breakage of anti-rotational screw, healed with conservative treatment (Fig. 4). We did not observe cases of non-union. No deep wound infection was observed. Hip pain after surgery was observed in 11 patients in group A (16.1%) and in 9 patients in group B (12%).
Discussion
The high incidence of hip fractures in the elderly represents a global health issue, especially because of the high rate of morbidity and mortality that is connected with it [13, 14]. Hip fractures are the fractures most frequently submitted to surgery and are the most frequent among the elderly, after wrist and vertebral fractures [15, 16]. The evolution of osteosynthesis allowed the development of increasingly accurate mini-invasive surgical techniques, in order to reduce soft tissue damage, blood loss, postoperative pain, and the general complications. Intramedullary nails can provide these advantages while also reducing surgery duration and transfusion requirements [17, 18].
In this retrospective study, we analyzed 143 intertrochanteric stable fractures treated with intramedullary nails. Sixty-eight were distally locked, and 75 were locked. unlocked nail has several advantages: first reduction in radiation exposure, for both the patient and the staff. Furthermore, in the proximity of the distal screw, increase in mechanical stress can lead to a hypertrophy of the surrounding cortical bone, pain in the fascia lata, and fractures around the screw. The hypertrophy of the distal cortical bone is a radiological sign of proximal stress shielding, with maximal stress at the nail tip [15, 19]. Hardy reports that the use of two static screws in the medullary nailing leads to a high degree of cortical hypertrophy, while the distal dynamic locking decreases the rate of this complication [20, 21]. On the basis of this observation, we reduced the use of distal blockage in the intertrochanteric stable fractures 31-A1 and 31-A2. Further important observation concerns the fact that in case distal locking was not performed, the surgical duration time was significantly shorter (p < 0.0001). Considering the clinical studies of US hospitals which have demonstrated that the average cost per minute of operating room time is $62 [22], we can infer that the non-locking procedure would result in considerable cost savings, especially given the extremely high occurrence of intertrochanteric fractures. Another factor to be taken into consideration is the risk of subsequent diaphyseal fractures around the distal part of the nail. In the unlocked nails, we did not have any fractures, while we had this type of fracture in two locked patients. Among the causes of the bone weakening at this distal implant-related fracture are excessive tightening of the distal screw and the excessive reaming of the medullary canal. Most of these fractures occur within three months from surgery [23, 24]. In the patient with no distal locking, we found a low incidence of decrease in hemoglobin. This is probably due to the fact that the distal screw is positioned in the proximity of the perforating branches of the deep femoral artery, whose accidental lesion during drilling can cause abundant postoperative bleeding [25].
Examining the radiographic results, we have to consider several aspects. Fracture healing is a frequent end point outcome in orthopedic research trials; therefore, differing and subjective accounts of fracture healing can dramatically affect the perceived efficacy of a treatment [26]. RUSH checklist improves the consistency and reliability of plain X-ray interpretation and, at the same time, increases the utility of hip fracture radiographs [10, 11].
RUSH appeared as a viable scoring system when applied to intertrochanteric hip fractures treated with intramedullary nail. Actually, the cortical/trabecular bridging and disappearance were easy to assess in both the radiographic views. The only problematic case is the evaluation of the lateral cortical bone; in these cases, the cephalic screw can hide the bridging and the fracture line. In such cases, we have inserted an intermediate consolidation value (2 points in the RUSH score). The significant improvement in RUSH during follow-up seems to reflect the union of fractures.
Consolidation seemed to advance similarly in both groups. TAD was not different in the two groups.
The present study has some weak points: The case record is not very wide, a lot of patients were lost at follow-up, and follow-ups were too short in order to assess late complications with a high degree of certainty. Moreover, an important limitation of this study is the absence of length and rotation stability measurements of the intertrochanteric fracture treated with or without distal locking screw.
In conclusion, the present study demonstrates that, in intertrochanteric 31-A1 and 31-A2 stable fractures, the absence of distal blocking screw does not compromise bone healing and prevents several clinical complications. Furthermore, this practice can provide other advantages, like cost saving and lower exposure to radiations. Nevertheless, more studies, especially randomized controlled trials, are necessary in order to validate our results.
References
Angulo Tabernero M, Aguilar Ezquerra A, Ungria Murillo J, Cuenca Espierrez J (2015) Epidemiology of fractures of the proximal third of the femur: 20 years follow-up. Rev Fac Cien Med Univ Nac Cordoba 72(3):145–151
Icks A, Arend W, Becker C et al (2013) Incidence of hip fractures in Germany, 1995–2010. Arch Osteoporos 8:140. https://doi.org/10.1007/s11657-013-0140-5
Pedersen AB, Baggesen LM, Ehrenstein V, Pedersen L, Lasgaard M, Mikkelsen EM (2016) Perceived stress and risk of any osteoporotic fracture. Osteoporos Int 27(6):2035–2045. https://doi.org/10.1007/s00198-016-3490-1
Dujardin FH, Benez C, Polle G, Alain J, Biga N, Thomine JM (2001) Prospective randomized comparison between a dynamic hip screw and a mini-invasive static nail in fractures of the trochanteric area: preliminary results. J Orthop Trauma 15(6):401–406
Hesse B, Gächter A (2004) Complications following the treatment of trochanteric fractures with the gamma nail. Arch Orthop Trauma Surg 124(10):692–698
Pajarinen J, Lindahl J, Michelsson O et al (2005) Pertrochanteric femoral fractures treated with a dynamic hip screw or a proximal femoral nail. A randomised study comparing post-operative rehabilitation. J Bone Joint Surg Br 87(1):76–81
Haidukewych GJ (2009) Intertrochanteric fractures: ten tips to improve results. J Bone Joint Surg Am 91(3):712–719
Gallagher D, Adams B, El-Gendi H et al (2013) Is distal locking necessary? A biomechanical investigation of intramedullary nailing constructs for intertrochanteric fractures. J Orthop Trauma 27(7):373–378. https://doi.org/10.1097/BOT.0b013e31827cd5bd
Rosenblum SF, Zuckerman JD, Kummer FJ et al (1992) A biomechanical evaluation of the Gamma nail. J Bone Joint Surg Br 74(3):352–357
Bhandari M, Chiavaras MM, Parasu N et al (2013) Radiographic union score for hip substantially improves agreement between surgeons and radiologists. BMC Musculoskelet Disord 14:70. https://doi.org/10.1186/1471-2474-14-70
Chiavaras MM, Bains S, Choudur H et al (2013) The Radiographic Union Score for Hip (RUSH): the use of a checklist to evaluate hip fracture healing improves agreement between radiologists and orthopedic surgeons. Skelet Radiol 42(8):1079–1088. https://doi.org/10.1007/s00256-013-1605-8
Court-Brown CM, Heckman JD, McQueen M, Ricci W, Tornetta P III, McKee M (2014) Rockwood and Green’s fractures in adults, VIII edn. Wolters Kluwer, Riverwoods
Ma J, Xing D, Ma X et al (2012) The percutaneous compression plate versus the dynamic hip screw for treatment of intertrochanteric hip fractures: a systematic review and meta-analysis of comparative studies. Orthop Traumatol Surg Res 98(7):773–783. https://doi.org/10.1016/j.otsr.2012.07.004
Varela-Egocheaga JR, Iglesias-Colao R, Suárez-Suárez MA et al (2009) Minimally invasive osteosynthesis in stable trochanteric fractures: a comparative study between Gotfried percutaneous compression plate and Gamma 3 intramedullary nail. Arch Orthop Trauma Surg 129(10):1401–1407. https://doi.org/10.1007/s00402-009-0955-0
Robinson CM, Adams CI, Craig M et al (2002) Implant-related fractures of the femur following hip fracture surgery. J Bone Joint Surg Am 84-A(7):1116–1122
López-Vega M, Gil-Monzó ER, Rodrigo-Pérez JL et al (2015) Randomized prospective study on the influence distal block and Gamma 3 nail on the treatment of intertrochanteric fractures of femur. Rev Esp Cir Ortop Traumatol 59(1):26–35. https://doi.org/10.1016/j.recot.2014.06.004
Ozkan K, Unay K, Demircay C, Cakir M, Eceviz E (2009) Distal unlocked proximal femoral intramedullary nailing for intertrochanteric femur fractures. Int Orthop 33(5):1397–1400. https://doi.org/10.1007/s00264-008-0673-1
Karn NK, Singh GK, Kumar P, Singh MP, Shrestha BP, Chaudhary P (2009) Management of trochanteric fractures of the femur with external fixation in high-risk patients. Int Orthop 33(3):785–788. https://doi.org/10.1007/s00264-008-0546-7
Barry TP (1984) Radiation exposure to an orthopedic surgeon. Clin Orthop Relat Res 182:160–164
Hardy DC, Drossos K (2003) Slotted intramedullary hip screw nails reduce proximal mechanical unloading. Clin Orthop Relat Res 406:176–184
Huang H, Xin J, Ma B (2014) Analysis of complications of intertrochanteric fracture treated with Gamma 3 intramedullary nail. Int J Clin Exp Med 7(10):3687–3693
Macario A (2010) What does one minute of operating room time cost? J Clin Anesth 22(4):233–236. https://doi.org/10.1016/j.jclinane.2010.02.003
Albareda J, Laderiga A, Palanca D, Paniagua L, Seral F (1996) Complications and technical problems with the gamma nail. Int Orthop 20(1):47–50
Saarenpää I, Heikkinen T, Jalovaara P (2007) Treatment of subtrochanteric fractures. A comparison of the Gamma nail and the dynamic hip screw: short-term outcome in 58 patients. Int Orthop 31(1):65–70
Han CD, Lee YH, Yang KH et al (2013) Relationship between distal screws and femoral arteries in closed hip nailing on computed tomography angiography. Arch Orthop Trauma Surg 133(3):361–366. https://doi.org/10.1007/s00402-012-1674-5
Davis BJ, Roberts PJ, Moorcroft CI, Brown MF, Thomas PBM, Wade RH (2004) Reliability of radiographs in defining union of internally fixed fractures. Injury 235(6):557–561
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Lanzetti, R.M., Caraffa, A., Lupariello, D. et al. Comparison between locked and unlocked intramedullary nails in intertrochanteric fractures. Eur J Orthop Surg Traumatol 28, 649–658 (2018). https://doi.org/10.1007/s00590-018-2143-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-018-2143-9