Abstract
Objective
Supracondylar femoral nonunions after dynamic condylar screw (DCS) treatment are uncommon, and few studies have addressed an optimal treatment technique for this disorder. Re-insertion of a new plate may not be secure because of bony defects in the distal fragment, created by the lag screw of the DCS.
Materials and methods
Forty-two consecutive adult patients with 42 supracondylar femoral nonunions were treated with removal of the DCS, re-alignment of the knee axis, and insertion of a retrograde dynamic traditional femoral locked nail. When necessary, a humeral plate was augmented to reinforce rotational stability.
Results
A final group of 36 patients with 36 nonunions were followed for an average of 2.8 years (range 1.1–6.2 years). All nonunions healed with a union rate of 100 %, and the average time to union was 4.2 months (range 2.5–5.5 months). Complications included two malunions. There were no instances of nonunion or deep infection. Satisfactory knee function among 36 patients improved from 8.2 % preoperatively to 86.1 % at the last follow-up (p < 0.001). All 36 patients could walk without aids.
Conclusion
The described technique may be an excellent alternative treatment for an aseptic supracondylar femoral nonunion after DCS treatment. The technique is not difficult, and the union rate and satisfactory rate are high.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Supracondylar femoral fractures are not uncommon [1, 2]. Due to the anatomic characteristics in this region (thin cortex, wide marrow cavity, and curved surface), which are unfavorable for implant stabilization, fracture treatment is often associated with a high rate of postsurgical complications [3, 4]. As many as 46 % of these patients have unsatisfactory results [1, 5].
Currently, the preferred implants for treatment of fractures in this region include plate and retrograde locked intramedullary nail systems [6–8]. However, each technique has unique advantages and disadvantages and none can be considered better than others. A locked plate has been increasingly used worldwide [9, 10]; however, the high cost and technical demands of this approach greatly limit its use [11, 12]. A dynamic condylar screw (DCS) has the advantages of convenient use and sufficient mechanical stability and thus is considered the best choice in various traditional plates for various supracondylar femoral fractures [13, 14].
The aseptic nonunion rate with a DCS to treat supracondylar femoral fractures ranges from 0 to 10 % [13, 15–17]. Once a nonunion occurs after DCS treatment, treatment can become extremely complex. The large bony defects in the distal fragment when the lag screw of the DCS is removed may critically compromise the stability of screws in a new plate.
Few studies have specifically reported treatment approaches for supracondylar femoral nonunions after DCS treatment [18]. Theoretically, re-inserting a new unlocked or locked plate may not provide sufficient stability for screw purchase in the distal fragment. Additionally, the rugged and uneven fragmented surface may greatly restrict an ideal area to place a new plate. Under such situations, a retrograde locked intramedullary nail may be valuable to stabilize the fracture fragments. Several authors have reported their success using a traditional dynamic femoral locked nail with a retrograde fashion to treat distal femoral nonunions [19, 20]. Could such a technique also be used to treat supracondylar femoral nonunions after DCS treatment? To answer this question, a retrospective study using retrograde dynamic traditional femoral locked nails to treat aseptic supracondylar femoral nonunions after DCS treatment was designed. The feasibility of such a use was carefully evaluated.
Materials and methods
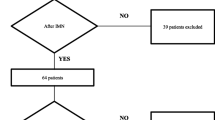
From May 2004 to July 2013, 42 consecutive adult patients of 18 years of age or older, with 42 supracondylar femoral nonunions after failed DCS treatment, were treated with retrograde dynamic locked intramedullary nailing at the author’s institution. The author treated and followed up all patients. The patients aged from 21 to 74 years (average, 37 years), and the male-to-female ratio was 3:1. Inclusion criteria for this study were patients with supracondylar femoral nonunions that had been stabilized with DCS. Patients with nonunions not treated by dynamic locked intramedullary nailing were excluded from the study. Patients with suspicious deep infections were advised to be treated with external fixation and were excluded from the study, while those who had previous deep infections that had subsided were included in the study.
At the outpatient department (OPD), patient’s treatment course was inquired carefully. All fractures were initially caused by high-energy injuries, such as automobile or motorcycle accidents, or falls from heights. Seven fractures were open [21]. Thirty-two fractures were initially treated at other hospitals. Eight fractures had resulted in deep infections. After repeated surgical treatment and antibiotic use, no infection recurred over an average of 1.8 years (range 1.4–2.6 years). The period from the initial injury to the present revision surgery averaged 2.3 years (range 0.7–4.6 years), and patients required from 1 to 6 surgeries (average 2.4 surgeries). The maximal knee flexion averaged 65° (range 0°–140°), and 28 patients had <90° of knee flexion. All patients were dependent on walking aids.
At the OPD, the fracture and wound healing processes of all patients were also carefully investigated. The knee range of motion (ROM) of each patient was measured with goniometry. Plain radiographs of the femur and knee, and full-length standing scanogram were routinely checked. The treatment plans were thoroughly explained to the patient and family. The approach and the angle requiring correction were determined.
At admission, complete blood cell (CBC) count, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) levels were routinely checked. Patients who had previous deep infection but subsided at the present time were treated, and vancomycin and ceftazidime were locally used intraoperatively.
Surgical technique
Patients received spinal or generalized anesthesia. A sterilized pneumatic tourniquet was routinely used and could be removed whenever necessary.
For patients with knee flexion >90°, a lateral approach along the prior incision wound was performed. The wound was extended along the prior lateral approach. The knee joint was opened after the wound was extended to the upper tibia. For those with <90° knee flexion, a midline approach with an inverted V-fashioned quadriceps flap incision was performed and the knee was bent to 90°. The prior DCS was removed, and the local area was thoroughly debrided. The knee axis was re-aligned with manipulation to fit the desired correction angle.
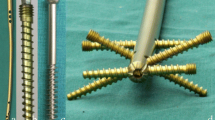
A 3-mm Kirschner wire (Mizuho Medical Co. Ltd., Tokyo, Japan) was inserted in the intercondylar notch 5–10 mm anterior to the insertion of the posterior cruciate ligament. An 8-mm reamer was used to enlarge the bony inlet in the intercondylar notch. Consequently, a flexible guide wire was inserted in a retrograde fashion from the bony inlet to the proximal marrow cavity. The marrow cavity was then reamed as widely as possible. After this, a 1-mm smaller traditional femoral locked nail (Smith & Nephew, Memphis, TN, USA; or Zimmer, Warsaw, IN, USA) was inserted in a retrograde fashion. Only the lower diagonal locked screws were inserted. The rotational stability was checked manually. If rotational stability was insufficient, a humeral dynamic compression plate (Synthes, Bettlach, Switzerland) was augmented. Cancellous bone graft procured from the ipsilateral tibial condyle and bone graft substitutes (Wiltrom Medical Inc., Hsinchu, Taiwan; 60 % hydroxyapatite and 40 % β-tricalcium phosphate) were packed in the nonunion site. For patients with prior deep infection, six vials of vancomycin (500 mg/vial, Tai-Yu Co., Hsinchu, Taiwan) and ceftazidime (500 mg/vial, China Chemical & Pharmaceutical Co., Taipei, Taiwan) powder were placed in situ. Bone graft was mixed with antibiotic powder and placed in the gap. The wound was closed with non-absorbable sutures, and a closed drain was inserted. For patients treated with the quadriceps flap approach, the quadriceps tendon was sutured with a V–Y mode with the knee in 80° flexion.
After surgery, progressive knee ROM exercise was encouraged, and patients were permitted to walk as early as possible using protected weight bearing. A continuous passive motion (CPM) device (OrthoLogic Canada Ltd., Toronto, Canada) was used with gradual increasing knee flexion. Patients were followed up at the OPD at 4–6 weeks intervals. Clinical and radiological fracture healing processes were then evaluated. After the fracture healed, patients were followed up each year and whenever necessary. Knee function evaluation was recorded at each follow-up.
Fracture union was defined as clinically lack of pain and tenderness at the fracture site, and the ability to walk without aids. In addition, solid callus had bridged the fragments in three of four views on plain radiographs [22, 23]. A nonunion was defined as the fracture site had not healed after 1 year of treatment or when a second surgery was necessary to achieve a union [24].
Knee function was evaluated using the modified Mize scoring system [25], which was selected because of its simplicity and relative practicality. Outcome included four grades, and a satisfactory result was defined as an excellent or good grade. An excellent grade consisted of: (1) absence of pain, (2) <10° flexion loss, (3) full extension, and (4) no varus, valgus, or rotational deformity. A good grade consisted of no more than one of the following: (1) >20° flexion loss, (2) >10° extension loss, (3) >10° valgus or rotational deformity, (4) >5° varus deformity, or (5) minimal pain. An unsatisfactory result included a fair grade (any two of the above criteria) and a failure grade (any of the following: flexion ≤90°, varus or valgus deformity >15°, joint incongruence, or disabling pain [25]).
Fisher’s exact test was used for statistical comparison. Statistical significance was p < 0.05.
Results
Thirty-six patients with 36 nonunions were followed up for at least 1 year (average, 2.8 years; range 1.1–6.2 years). Six patients were lost to follow-up despite maximal efforts to contact them. The six patients discontinued to follow after being discharged with an average of 1.2 months (range 0–2.5 months). The final group of 36 patients included six patients with previous deep infection. Seven of the forty-two original knees required plate augmentation to protect the patients from rotational instability.
Femoral locked nails of the diameters of 11–13 mm were used. Cancellous bone grafting was performed in all 42 patients, and bone graft substitute was added in 13 patients.
All 36 fractures healed with a union rate of 100 % (36/36) and an average union time of 4.2 months (range 2.5–5.5 months; Figs. 1, 2, 3).
A 38-year-old man sustained a right supracondylar femoral nonunion for 1.6 years. Removal of the dynamic condylar screw, retrograde dynamic locked nailing, and cancellous bone grafting were performed. The fracture healed within 4.5 months. At the 4.8-year follow-up, the patient had good knee function
A 63-year-old woman sustained a left supracondylar femoral nonunion for 2 years. Removal of the dynamic condylar screw, retrograde dynamic locked nailing, plate augmentation, and cancellous bone grafting were performed. The fracture healed within 4 months. At the 5.7-year follow-up, the patient had good knee function
Complications included two malunions (>5° varus, >10° valgus or rotational deformity). No patients had leg length discrepancy >2 cm. There were no nonunions or deep infections. Malunions in two patients were caused by associated varus knees of 8° and 10°. No reoperations were needed.
Satisfactory knee function was improved from 8.3 % (3/36) of patients preoperatively to 86.1 % (31/36) at the last follow-up (p < 0.001, Table 1). The unsatisfactory knees in five patients were due to associated flexion loss and minimal pain. All patients could walk without aids.
Usually, the retrograde nail was suggested to be removed in patients with prior infection after 2 years. For patients without prior infection, implants were removed as patients’ request. At the latest follow-up, 21 nails were removed.
Discussion
After the supracondylar femur was realigned, a dynamic locked nail was inserted in a retrograde fashion. The gaps in the marrow cavity were eradicated by intramedullary reaming, packing cancellous bone graft or bone graft substitutes, and using a dynamic locked nail. The axial and bending stabilities are steadily provided by a locked nail with distal locking [26, 27]. The osteogenic potentials can be initiated by use of cancellous bone graft [28]. A 100 % union rate was achieved in the current study.
Few specific reports of supracondylar femoral nonunions after DCS treatment have appeared in the medical literature [18]. Theoretically, such nonunions might be treated with various traditional or locked plates [29]. Anatomically, a large bony defect in the distal fragment after the lag screw is removed may greatly hinder new screw purchase. Therefore, bone graft or bone cement may be necessary to fill the defect concomitantly. This added procedure may greatly increase the technical complexity; however, using a retrograde locked nail without paralleling the orientation of the lag screw can overcome this technical disadvantage. Using buttress condylar plates to treat supracondylar femoral nonunions after DCS treatment, Chapman and Finkemeier [18] achieved a 100 % union rate with a 60 % satisfactory knee function in five patients. Using a new DCS, Chapman and Finkemeier [18] achieved a 100 % union rate with a 66 % satisfactory knee function in three patients. Using a locked plate, Hailer and Hoffmann [30] achieved a 100 % union rate with a 100 % satisfactory knee function in one case report. Using a custom retrograde femoral nail, Khan et al. achieved a 100 % union rate with a 100 % satisfactory knee function in two patients [31]. In the current study, a 100 % union rate with an 86 % satisfactory knee function was achieved in 36 patients (Table 1).
Factors that favor fracture healing are a minimal gap, adequate stability, and sufficient nutrition [32]. A DCS is considered the strongest implant among various traditional plates [13]. The causes for failed treatment of supracondylar femoral fractures with a DCS may include all three described factors [32]. The fracture site may be poorly reduced with a big gap. The fragments may be so comminuted or osteoporotic that the lag screw cannot be steadily placed. Although the bridging technique is developed to save periosteal dissection, vascular compromise may have occurred during injury in comminuted fractures [16]. Despite the fact that DCS treatment may have high success rates, nonunions normally cannot be completely avoided. In other words, techniques to treat supracondylar femoral nonunions after DCS treatment still require to be continuously improved. Using DCS with a minimally invasive percutaneous plate osteosynthesis (MIPPO) technique to treat supracondylar femoral fractures, Krettek et al. [16] reported achieving a 100 % union rate and 70 % of their patients had satisfactory knee function.
A static classic supracondylar nail has been used very successfully to treat supracondylar femoral fractures [33, 34]. Theoretically, the nails can also be used to treat nonunions in the supracondylar femur. However, the short length of the nail may introduce a femoral shaft fracture due to the proximal end of the nail acting as a stress riser [35]. In addition, a classic supracondylar nail is expensive. Thus, using a classic supracondylar nail may not be a better approach than using a traditional femoral locked nail. Many authors recommended a retrograde locked nail reaching the level of the lesser trochanter [36]. Thus, insertion of the upper locked screw becomes technically difficult. In the current study, a dynamic femoral locked nail was used and the upper locked screws were not inserted.
The stability of the proximal fragment relies on three-point friction forces between the nail and femur [37, 38]. Should the anti-rotational stability be insufficient by manual tests, a humeral plate is augmented. Because the plate was used simply for anti-rotation, a humeral plate proved sufficient [19]. The humeral plate was not difficult to place in the small distal fragment because of its small width.
This study may have some limitations. First, a DCS may be gradually replaced by a locked plate and bony defects in the distal fragment may not be evident. However, a locked plate is expensive and technically demanding [11, 12]. A DCS for supracondylar femoral fractures may not be completely replaced. Thus, the technique described in this study may provide an alternate and optimal treatment. Next, the retrograde locked nail is recommended for use in a dynamic mode. Inserting proximal locked screws at the lesser trochanter level requires an image intensifier and is technically demanding. At times augmentation of a small plate to reinforce rotational stability may be necessary. Inserting screws on the bone with an intramedullary nail in the marrow cavity requires pre-drilling the screw tract using a Kirschner wire first. Or, the drill-bit easily breaks when the nail is impacted. All surgeons must understand this concept before the plate augmentation is performed.
In conclusion, a retrograde dynamic traditional femoral locked nail may be an excellent alternative and an optimal choice for aseptic supracondylar femoral nonunions after DCS treatment. The technique is not difficult, and the union rate and satisfactory function rate are high.
References
Merchan ECR, Maestu PR, Blanco RP (1992) Blade-plating of closed displaced supracondylar fractures of the distal femur with the AO system. J Trauma 32:174–178
Wahnert D, Hoffmeier K, Frober R, Hofmann GO, Muckley T (2011) Distal femur fractures of the elderly—different treatment options in a biomechanical comparison. Injury 42:655–659
Wu CC, Shih CH (1992) Treatment of femoral supracondylar unstable comminuted fractures: comparison between plating and Grosse-Kempf interlocking nailing techniques. Arch Orthop Trauma Surg 111:232–236
Wang JW, Weng LH (2003) Treatment of distal femoral nonunion with internal fixation, cortical allograft struts, and autogenous bone-grafting. J Bone Joint Surg (Am) 85:436–440
Moore TJ, Watson T, Green SA, Garland DE, Chandler RW (1987) Complications of surgically treated supracondylar fractures of the femur. J Trauma 27:402–406
Stover M (2001) Distal femoral fractures: current treatment, results and problems. Injury 32(Suppl 3):SC3–SC13
Watanabe Y, Takai S, Yamashita F, Kusakabe T, Kim W, Hirasawa Y (2002) Second-generation intramedullary supracondylar nail for distal femoral fractures. Int Orthop 26:85–88
Shan S, Desai P, Mounasamy V (2015) Retrograde nailing of femoral fractures: a retrospective study. Eur J Orthop Surg Traumatol 25:1093–1097
Granata JD, Litsky AS, Lustenberger DP, Probe RA, Ellis TJ (2012) Immediate weight bearing of comminuted supracondylar femur fractures using locked plate fixation. Orthopedics 35:e1210–e1213
Assari S, Kaufmann A, Darvish K, Park J, Haw J, Safadi F, Rehman S (2013) Biomechanical comparison of locked plating and spiral blade retrograde nailing of supracondylar femur fractures. Injury 44:1340–1345
Henderson CE, Lujan TJ, Kuhl LL, Bottlang M, Fitzpatrick DC, Marsh JL (2011) Healing complications are common after locked plating for distal femur fractures. Clin Orthop Relat Res 469:1757–1765
Collinge CA, Gardner MJ, Crist BD (2011) Pitfalls in the application of distal femur plates for fractures. J Orthop Trauma 25:695–706
Petsatodis G, Chatzisymeon A, Antonarakos P, Givissis P, Papadopoulos P, Christodoulou A (2010) Condylar buttress plate versus fixed angle condylar blade plate versus dynamic condylar screw for supracondylar intra-articular distal femoral fractures. J Orthop Surg (Hong Kong) 18:35–38
Henderson CE, Kuhl LL, Fitzpatrick DC, Marsh JL (2011) Locking plates for distal femur fractures: Is there a problem with fracture healing? J Orthop Trauma 25(Suppl 1):S8–S14
Shewring DJ, Meggitt BF (1992) Fractures of the distal femur treated with the AO dynamic condylar screw. J Bone Joint Surg (Br) 74:122–125
Krettek C, Schandelmaier P, Miclau T, Tscherne H (1997) Minimally invasive percutaneous plate osteosynthesis (MIPPO) using the DCS in proximal and distal femoral fractures. Injury 28(Suppl 1):A20–A30
Christodoulou A, Terzidis I, Ploumis A, Metsovitis S, Koukoulidis A, Toptsis C (2005) Supracondylar femoral fractures in elderly patients treated with the dynamic condylar screw and the retrograde intramedullary nail: a comparative study of the two methods. Arch Orthop Trauma Surg 125:73–79
Chapman MW, Finkemeier CG (1999) Treatment of supracondylar nonunions of the femur with plate fixation and bone graft. J Bone Joint Surg (Am) 81:1217–1228
Wu CC (2009) Retrograde dynamic locked nailing for femoral supracondylar nonunions after plating. J Trauma 66:195–199
Wu CC (2011) Retrograde dynamic locked nailing for aseptic nonunion of femoral supracondyle after antegrade locked nailing. Arch Orthop Trauma Surg 131:513–517
Gustilo RB, Anderson JTT (1976) Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones with retrospective and prospective analysis. J Bone Joint Surg (Am) 58:453–458
Kempf I, Grosse A, Beck G (1985) Closed locked intramedullary nailing: its application to comminuted fractures of the femur. J Bone Joint Surg (Am) 67:709–720
Pihlajamaki HK, Salminen ST, Bostman OM (2002) The treatment of nonunion following intramedullary nailing of femoral shaft fractures. J Orthop Trauma 16:394–402
Seinsheimer F (1978) Subtrochanteric fractures of the femur. J Bone Joint Surg (Am) 60:300–306
Mize RD, Bucholz RW, Grogan DP (1982) Surgical treatment of displaced, comminuted fractures of the distal end of the femur: an extensile approach. J Bone Joint Surg (Am) 64:871–879
Heiney JP, Battula S, O’Connor JA, Ebraheim N, Schoenfeld AJ, Vrabec G (2012) Distal femoral fixation: a biomechanical comparison of retrograde nail, retrograde intramedullary nail, and prototype locking retrograde nail. Clin Biomech 27:692–696
Paller DJ, Frenzen SW, Bartlett CS 3rd, Beardsley CL, Beynnon BD (2013) A three-dimensional comparison of intramedullary nail constructs for osteopenic supracondylar femur fractures. J Orthop Trauma 27:93–99
Stevenson S (1998) Enhancement of fracture healing with autogenous and allogeneic bone grafts. Clin Orthop Relat Res 355S:S239–S246
Koval KJ, Seligson D, Rosen H, Fee K (1995) Distal femoral nonunion: treatment with a retrograde inserted locked intramedullary nail. J Orthop Trauma 9:385–391
Hailer YD, Hoffmann R (2006) Management of a nonunion of the distal femur in osteoporotic bone with the internal fixation system LISS (less invasive stabilization system). Arch Orthop Trauma Surg 126:350–353
Khan AM, Ryan MG, Meinhard BP, Miller T (1999) Use of a custom retrograde intramedullary rod for the management of distal femoral nonunion: a report of two cases. Am J Orthop 28:361–364
Karlstrom G, Olerud S (1974) Fractures of the tibial shaft: a critical evaluation of treatment alternatives. Clin Orthop Relat Res 105:82–111
Henry SL, Trager S, Green S, Seligson D (1991) Management of supracondylar fractures of the femur with the GSH intramedullary nail: preliminary report. Contemp Orthop 22:631–640
Zlowodzki M, Williamson S, Cole PA, Zardiackas LD, Kregor PJ (2004) Biomechanical evaluation of the less invasive stabilization system, angled blade plate, and retrograde intramedullary nail for the internal fixation of distal femur fractures. J Orthop Trauma 18:494–502
Leibner ED, Mosheiff R, Safran O, Abu-Snieneh K, Liebergall M (1999) Femoral fracture at the proximal end of an intramedullary supracondylar nail: a case report. Am J Orthop 28:53–55
Ricci WM (2005) Femur: trauma. In: Vaccaro AR (ed) Orthopedic knowledge update: 8. American Academy of Orthopedic Surgeons, Rosemont, IL, pp 425–431
Barry M, Paterson JMH (2004) Flexible intramedullary nails for fractures in children. J Bone Joint Surg (Br) 86:947–953
Vallamshetla VRP, Dc Silva U, Bache CE, Gibbons PJ (2006) Flexible intramedullary nails for unstable fixation of the tibia in children: an eight-year experience. J Bone Joint Surg (Br) 88:536–540
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Wu, CC. Retrograde dynamic locked intramedullary nailing for aseptic supracondylar femoral nonunion after dynamic condylar screw treatment. Eur J Orthop Surg Traumatol 26, 625–631 (2016). https://doi.org/10.1007/s00590-016-1800-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-016-1800-0