Abstract
The aim of the present study was to analyze the clinical and radiographic outcomes and Kaplan–Meier survivorship of patients who underwent revision surgeries of the acetabular cup that had sustained aseptic loosening. We reviewed 101 consecutive patients (120 hips; 10 men 11 hips; 91 women 109 hips; age at surgery 66 years; range 45–85) who underwent acetabular component revision surgery, at a follow-up period of 15.6 years (range 10–32). To evaluate the state of the acetabulum, acetabular bony defects were classified according to the AAOS classification based on intraoperative findings: type I (segmental deficiencies n = 24 hips), type II (cavity deficiency n = 48), type III (combined deficiency n = 46), and type IV (pelvic discontinuity n = 2). The Harris hip score improved from 42.5 ± 10.8 (mean ± SD) before surgery to 74.9 ± 14.6 points at follow-up. The survival rates of the acetabular revision surgery with cemented, cementless, and cemented cups plus reinforcement devices were 74, 66, and 82 %, respectively. The difference in the survival rate between the cemented and cementless group was marginal (p = 0.048 Gehan–Breslow–Wilcoxon, p = 0.061 log-rank), probably due to the early-stage failure cases in the cementless group. The cementless and reinforcement groups included nine early-stage failure cases. To prevent early-stage failure, we recommend the cementless cups for types I and II acetabular bone defects with adequate contact between host bone and acetabular component, and the cemented cup with or without reinforcement devices, together with restoration of bone stock by impaction or structured bone grafting, for cases lacking such contact.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total hip arthroplasty (THA) is one of the preferable solutions for regaining ambulatory activity in patients with end-stage osteoarthritis (OA), and the procedure is well developed technically and large numbers of patients benefit from THA worldwide [1–3]. However, despite the improvements in implant designs and surgical techniques, the revision rate remains high, and the number of revisions is expected to increase in the future due to the increase in the volume of primary THA and the proportion of younger, more active patients who are likely to survive longer than their prosthetic implants [4, 5].
Compared with primary THA, greater technical and decision-making challenges face the surgeon at revision THA, especially due to the need to manage acetabular bone loss and uncertainties regarding implant choice, and fixation strategies [4]. Various procedures of revision surgery and devices have been described for the reconstruction of the acetabulum, such as cemented cups [6–8], cementless cups [4, 9, 10] including the use of jumbo cups [11, 12], and the combination of cemented cups and reinforcement devices [13–15]. In addition, various techniques of bone grafting for the acetabular bone defects have been reported [16–18]. However, despite the number of proposed solutions, reconstruction of the acetabulum in revision THA is still a perplexing problem [4, 8, 17].
The present retrospective study is a long-term follow-up study (mean follow-up period of 15.6 years) designed to characterize the clinical and radiographic outcome of acetabular revision surgery. Specifically, we compared the long-term survival rates of the cemented cups, cementless cups, and cemented cups with reinforcement devices, after acetabular revision surgeries.
Materials and methods
Patient demographics
This study was designed to review patients with follow-up period of 10–32 years after acetabular cup revision surgery. Between 1988 and 2005, 117 Japanese patients (137 hips) with THA that had sustained aseptic loosening underwent acetabular revision surgery at our University Hospital. In this series, 8 patients (9 hips) died prior to the 10-year follow-up visit without having undergone additional surgery, and 6 patients (6 hips) were lost to follow-up before the 10-year period. These 14 patients (15 hips) were excluded, but 20 patients (23 hips) who died after the 10-year follow-up examination were included in this study, where the date of the last consultation was considered the final examination. The cause of death was unrelated to acetabular reconstruction. Fourteen patients who were lost to follow-up after the 10-year follow-up examination were also included in this study. Twenty-two patients who underwent a second or third revision surgery were included but only data of the first revision surgery were analyzed in this case series. In addition, two hips with septic loosening of the implants were excluded from the study. Thus, the remaining 101 patients (120 hips) were the subjects of this study.
Nineteen patients (one man; 18 women) had bilateral lesions and 82 (nine men; 73 women) had unilateral aseptic loosening. Isolated acetabular revision was performed in 68 cases, while the remaining 52 patients underwent revision of both acetabular and femoral components. The mean age of the patients at the time of revision surgery was 65.8 years (range 45–85). The primary diagnosis before primary THA was osteoarthritis in 100 hips, rheumatoid arthritis in 9, and avascular necrosis of the femoral head in 11.
Surgical technique
All surgeries were conducted through a standard posterolateral approach with a reduced and curved skin incision, removal of loose components, curettage of pseudomembrane, and removal of previous cement to provide acetabular exposure. Acetabular bone defects were classified based on the following intraoperative findings and according to the classification of the American Academy of Orthopaedic Surgeons (AAOS) [19]: type I (segmental deficiencies in periphery and/or center of the acetabulum) in 24 hips, type II (cavitary deficiency in periphery and/or center) in 48 hips, type III (combined deficiency) in 46, and type IV (pelvic discontinuity) in two.
The treatment strategies for acetabular reconstruction were as follows. For type I acetabular defects, the acetabulum was prepared using hemispherical reamers, and then, the acetabular cup was either cemented into place or press-fit into the acetabulum with the addition of screws placed through the cementless cup with or without morselized bone grafting from acetabular reaming. For type II defects, any cavity defect in the center of the acetabulum was packed with structural or crushed allograft before fixation of the cement or cementless cup. On the other hand, for type III defects and type II defects with large cavity deficiency at the superio-lateral aspect of the acetabulum, we used a reinforcement plate or ring with structural and/or crushed allograft by forced impaction, followed by fixation of the polyethylene cup with cement. For type IV bone defects, a reinforcement device was selected after structural and/or impaction bone grafting, together with fixation of the posterior column using a reconstruction plate. However, since this study included elderly subjects, impaction bone grafting was performed in only 12 cases, and treatment of one patient with grade IV defect included only the use of reinforcement plate. In addition, we tended to use the cement cup before 1994, but this was gradually replaced with the cementless cup. Furthermore, conventional polyethylene liner was used in 48 hips before 1998, but this was subsequently changed to cross-linked polyethylene liner (72 hips).
A total of 37 acetabular cement cups were used, which included 30 MC-1 cups (Stryker Orthopaedics, Mahwah, NJ), 5 polyethylene acetabular cups (Stryker Orthopaedics), and 2 sockets (KYOCERA Medical, Osaka, Japan). On the other hand, 36 cementless cups were used, including 11 SecureFit PSL cups (Stryker Orthopaedics), 9 TriAD HA cups (Stryker Orthopaedics), 7 ATH shells (KYOCERA Medical), 4 APR cups (Zimmer, Warsaw, IN), 3 microstructured cups (Stryker Orthopaedics), and 2 AMS HA shells (KYOCERA Medical). We used 47 reinforcement devices, which included 34 KT plates (KYOCERA Medical), 8 Müller acetabular supporting rings (Zimmer), and 5 Kerboull acetabular cross-plates (Stryker Orthopaedics). The operation time ranged from 1.5 to 6.2 h (mean 3.2 h) and the mean blood loss was 632 g (range 200–4500). None of the patients suffered insult to the sciatic nerve, deep venous thrombosis, or developmental heterotopic ossification. Ambulation was allowed 2–42 days after surgery, and patients were discharged 20–85 days after surgery.
Ten- to thirty-two-year follow-up study
Follow-up investigation was performed every 1 year after the revision surgery and included evaluation of the Harris hip score before surgery and at the latest clinical examination, and radiography. Radiological assessment was performed on standard antero-posterior and lateral radiographs taken after surgery and at each follow-up visit. The acetabular component was classified as definitely loose if the sum of horizontal and vertical migration was >5 mm, if the change in the acetabular component was >5°, or if there was a progressive radiolucent line >1 mm around the whole acetabular component [20, 21]. The mean follow-up period was 15.6 years (range 10–32).
The protocol for investigating the clinical outcome and radiological findings was approved by the Ethics Review Committee of Fukui University Faculty of Medicine, and a written informed consent was obtained from all patients.
Statistical analysis
Changes in Harris hip score were evaluated with two-tailed Student’s t tests. The Kaplan–Meier analysis was performed to assess survival rates, in which the endpoint was defined as re-revision surgery. Comparison of the survival rate of the different groups (cemented cups, cementless cups, and cemented cups with reinforcement devices) was performed with the log-rank and Gehan–Breslow–Wilcoxon tests. A significant difference was defined as p < 0.05. Data were expressed as mean ± standard deviation (SD). Changes in Harris hip score were evaluated with two-tailed Student’s t tests, and comparison of Harris hip score between the groups was evaluated with analysis of variance (ANOVA). All analyses were conducted using SPSS Statistics for Mac OS version 21 software (IBM, Armonk, NY).
Results
Kaplan–Meier survival rate
Kaplan–Meier survival rate with re-revision at 10 years as the endpoint was 95 % (95 % confidence interval [CI], 87–102) in the cemented group, 80 % (95 % CI, 75–97) in the cementless group, and 84 % (95 % CI, 81–98) in the reinforcement group. The rate at the final follow-up was 74 % (95 % CI, 34–97), 66 % (95 % CI, 31–90), and 82 % (95 % CI, 66–94), respectively (Fig. 1). The survival rate tended to be better in the cemented group than the cementless group, but the difference was only marginal (p = 0.048 by Gehan–Breslow–Wilcoxon test, p = 0.061 by log-rank test). There were no significant differences among the other groups.
Kaplan–Meier survival curves with re-revision as the endpoint. The survival rates of the acetabular revision surgery with cemented cups, cementless cups, and cemented cups with reinforcement devices were 74, 66, and 82 %, respectively. The survival rate for cemented group was statistically better than that of the cementless group with marginal difference [p = 0.048 by Gehan–Breslow–Wilcoxon test, p = 0.061 by log-rank test (asterisks)], due to the initial failure of the cementless group
Clinical results
The mean preoperative Harris hip score improved significantly after surgery in patients treated with the cemented cup [from 43.5 ± 13.6 (range 16–58) to 77.2 ± 15.1 points (42–96)], cementless cup [from 43.6 ± 12.2 (12–60) to 76.2 ± 14.4 points (38–92)], and reinforcement device [40.9 ± 10.2 (18–58) to 72.1 ± 17.8 points (32–92)] (p < 0.001, each). There were no significant differences among the groups.
Radiographic findings
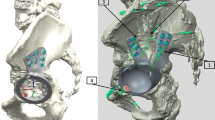
In patients treated by cemented cups, radiolucency was noted in 14 hips including 8 hips with cup migration. Of these cases, re-revision was performed in 6 hips while no treatment was provided in the remaining 8 hips (Fig. 2). In patients treated by cementless cups, changes in the acetabular component were observed within 2 years in 4 hips (Table 1; Fig. 3), and radiolucency was noted in 7 hips. Re-revision surgery was conducted in 8 hips while no treatment was provided in 3 hips. All other cases showed no significant radiolucency, though wear of the polyethylene liner was noted. Patients treated by cemented cups with reinforcement devices demonstrated breakage of the reinforcement plates with absorption of the grafting bones in 10 hips, dislodgement of the cemented cup within 2 years in one, and migration of the reinforcement ring in one. Breakage of the reinforcement plates occurred within 2 years in 4 cases (Table 1; Fig. 4). Re-revision surgery was conducted in 8 cases, while the other 4 have not yet undergone such surgery.
Serial antero-posterior radiographs taken a 1 week, b 10 years, c 20 years, d 25 years, and e 30 years after right-side cemented revision THA in a 58-year-old woman. The acetabulum with AAOS type II bone defect was reconstructed by Socket (KYOCERA Medical), which was a cemented standard polyethylene cup, with structural bone grafting. Radiolucency between the cement and bone was observed with cup migration 25 years after the revision surgery (d), but the patient did not complain of pain or any disability
Serial antero-posterior (a, b, c) and lateral (d, e, f) radiographs taken 1 week (a, d), 3 months (b, e), and 8 months (c, f) after left-side acetabular revision surgery by cementless cup in a 68-year-old man (Patient 4, Table 1). Impaction bone grafting with hydroxyapatite was performed for AAOS type III bone defect (a, b), and the space between the acetabular component and impacted mixture of hydroxyapatite and allograft demonstrated impacted allograft (arrows in d). Eight months after the revision surgery, a clear zone was observed on the lateral view of the radiograph (arrowhead in f). Intraoperative photograph just after removal of the loose cementless cup showed that the acetabular surface was covered by granulation tissue (g)
Serial antero-posterior radiographs taken a 1 week, b 6 months, c 1 year, and d 2 years after right-side revision THA with KT plate (KYOCERA Medical) and polyethylene acetabular cup (Stryker Orthopaedics) in a 56-year-old woman. The acetabulum with AAOS type II bone defect was reconstructed after allograft bone grafting without impaction (a). Collapse of the grafted bone and breakage of the KT plate occurred 2 years after the revision surgery (d)
Discussion
This 10–32 year follow-up study of acetabular revision surgeries, which compared the survival rates of the cemented cups, cementless cups, and cemented cups with reinforcement devices, demonstrated a trend toward the cemented group to have a better survival rate than the cementless group; however, the difference was only marginal (p = 0.048 Gehan–Breslow–Wilcoxon, p = 0.061 log-rank). We considered that this marginal difference was due to the early-stage failure of the cementless group. In addition, there was no significant difference in the survival rate between the cemented and reinforcement group; however, Kaplan–Meier curves of these groups were similar including several early-stage failure cases. Because of the limitation of this non-randomized retrospective study, it was difficult to compare the survival rate between the groups simply; however, the decrease in survival rate after 10 years in all groups was dependent on the wear of standard polyethylene liner [21], and the cementless and reinforcement group included several early-stage failure cases.
Sternheim et al. [8] followed their patients for 18 years after surgery and reported that the 20-year survival rates of the cemented and cementless cups were 36 and 76 %, respectively. However, they also described that patients of the cemented cup group predated those of the cementless group and suggested that the reason for the finding was in part related to the use of small-diameter cups in some patients. While high failure rates of the cemented acetabular components have been reported [4, 8], others reported that the use of cemented cups together with impaction bone grafting in patients with rheumatoid arthritis during revision surgery was associated with significant improvement in the long-term survival rate (85 % at 8–19 year follow-up) in comparison with other techniques [7]. In our case series, the cemented cup was mostly used before 1994, while the conventional polyethylene cups were used before 1998. We considered that these practices in the selection of preferred implants might have influenced the survival rate of the cemented cup.
On the other hand, several reports [4, 8, 9, 11, 12, 16] described satisfactory long-term outcome using the cementless components in acetabular cup revision surgery. Sternheim et al. [8] argued that the favorable outcome of the cementless cup could be due to the biologic fixation achieved by bone ingrowth onto the cementless cups. In the present study, the 10- to 25-year survival rate of the cementless cups was 66 %. The survival rate gradually decreased, similar to that of cemented cups, but the cementless group included four cases with failure occurring within 2 years after revision surgery, and such failure was due to implant instability. In this regard, Patel et al. [16] stressed the importance of achieving at least more than 50 % host bone contact in the part of the dome and posterior column. We considered that the cause of instability of the acetabular components in Patients 2 and 4 (Table 1) was lesser contact between the component and host bone. In other words, inadequate bone grafting was the cause of instability in Patient 2, and implant instability was due to the contact between the component and impacted allograft at most areas of the component. In Patients 1 and 3 (Table 1), the contact between the acetabular components and host bone was adequate; however, the bone quality of the acetabulum was relatively low. We believe that the selection of the cementless cup in acetabular revision surgery should be limited to patients with adequate acetabular bone stock at the superio-lateral and posterior acetabulum, with confirmed good bone quality. Such selection strategy should ensure satisfactory early outcome, which in turn could improve long-term outcome of the cementless cups.
Reconstruction of acetabula with considerable pelvic bone stock deficiencies, such as AAOS type III and IV bone defects, in revision arthroplasty, requires complex reconstructive techniques. Bone grafting is one of the most effective procedures for reconstruction of acetabula with massive bone defects. However, van Haaren et al. [17] reported postoperative failure in 34 % of patients who undertook revision THA with impaction bone grafting and cemented cups for AAOS type III or IV acetabular bone defects during 7.2-year follow-up period. They reasoned the high failure rate of the cemented impaction grafting technique to the extent of bone defect and especially the lack of bony support behind the graft in case of large segmental defects. In the present study, we used reinforcement plate or ring in the majority of cases with type III and IV bone defects except in two cases with type III defects. The survival rate of the cemented cups with reinforcement devices was 82 % for the 10–17 year follow-up. In this group, five patients developed failure within 2 years, including dislodgement of the cemented cup from the Müller ring in one hip, and breakage of reinforcement plate in four. A reinforcement plate or ring, such as Kerboull plate, KT plate, or Müller ring, must be used and placed as close as possible to the original acetabular position. It should also be used in combination with a morselized and/or structural bone graft for bone defects to prevent future failure [13–15]. In this regard, only chip allograft was used to fill the acetabular defects in four cases who developed breakage of the reinforcement plate. We emphasize here the importance of impaction allografting and/or structural bone grafting for type III acetabular defect, especially to the weight-bearing portion to prevent early-stage failure.
Conclusions
In conclusion, we reported that the mean 15.6-year follow-up (range 10–32) survival rates of acetabular revision with cemented cups, cementless cups, and cemented cups with reinforcement devices were 74, 66, and 82 %, respectively. While the survival rate of the cemented cups tended to be better than those of the cementless group, the difference was only marginal (p = 0.048 Gehan–Breslow–Wilcoxon, p = 0.061 log-rank). The marginal difference was due to the early-stage failure cases of the cementless group. Nine cases of the cementless and reinforcement groups showed early-stage failure. To prevent such failures, we believe that the use of cementless cups should be limited to types I and II acetabular bone defects with adequate contact of host bone and acetabular component. On the other hand, the cemented cup with or without reinforcement devices, together with restoration of bone stock by impaction or structured bone grafting, should be selected for those cases with inadequate contact between the host bone and acetabular component.
References
Ando M, Imura S, Omori H, Okumura Y, Bo A, Baba H (1999) Nonlinear three-dimensional finite element analysis of newly designed cementless total hip stems. Artif Organs 23:339–346
Kawahara H, Kokubo Y, Yayama T, Uchida K, Kobayashi S, Nakajima H, Oki H, Negoro K, Mwaka ES, Orwotho NT, Baba H (2010) Metaphyseal-loading anterolaterally-flared femoral stem in cementless total hip arthroplasty: five- to eleven-year follow-up evaluation. Artif Organs 34:377–383
Kokubo Y, Uchida K, Oki H, Negoro K, Nagamune K, Kawaguchi S, Takeno K, Yayama T, Nakajima H, Sugita D, Yoshida A, Baba H (2013) Modified metaphyseal-loading anterolaterally flared anatomic femoral stem: five- to nine-year prospective follow-up evaluation and results of three-dimensional finite element analysis. Artif Organs 37:175–182
Kremers HM, Howard JL, Loechler Y, Schleck CD, Harmsen WS, Berry DJ, Cabanela ME, Hanssen AD, Pagnano MW, Trousdale RT, Lewallen DG (2012) Comparative long-term survivorship of uncemented acetabular components in revision total hip arthroplasty. J Bone Joint Surg 94A:e82
Kurtz S, Ong K, Lau E, Mowat F, Halpern M (2007) Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg 89A:780–785
Trumm BN, Callaghan JJ, George CA, Liu SS, Goetz DD, Johnston RC (2014) Minimum 20-year follow-up results of revision total hip arthroplasty with improved cementing technique. J Arthroplasty 29:236–241
Schreurs BW, Luttjeboer J, Thien TM, de Waal Malefijt MC, Buma P, Veth RP, Slooff TJ (2009) Acetabular revision with impacted morselized cancellous bone graft and a cemented cup in patients with rheumatoid arthritis. A concise follow-up, at eight to nineteen years, of a previous report. J Bone Joint Surg 91A:646–651
Sternheim A, Abolghasemian M, Safir OA, Backstein D, Gross AE, Kuzyk PR (2013) A long-term survivorship comparison between cemented and uncemented cups with shelf grafts in revision total hip arthroplasty after dysplasia. J Arthroplasty 28:303–308
Trumm BN, Callaghan JJ, Liu SS, Goetz DD, Johnston RC (2012) Revision with cementless acetabular components: a concise follow-up, at a minimum of twenty years, of previous reports. J Bone Joint Surg 94A:2001–2004
Kim KC, Ha YC, Kang BJ, Lee YK, Ji HM, Koo KH (2012) Use of cementless acetabular component with a hook and iliac flanges in revision arthroplasty for massive acetabular defect. J Orthop Sci 17:18–24
Gustke KA, Levering MF, Miranda MA (2014) Use of jumbo cups for revision of acetabulae with large bony defects. J Arthroplasty 29:199–203
Lachiewicz PF, Soileau ES (2013) Fixation, survival, and dislocation of jumbo acetabular components in revision hip arthroplasty. J Bone Joint Surg 95A:543–548
Wegrzyn J, Pibarot V, Jacquel A, Carret JP, Béjui-Hugues J, Guyen O (2014) Acetabular reconstruction using a Kerboull cross-plate, structural allograft and cemented dual-mobility cup in revision THA at a minimum 5-year follow-up. J Arthroplasty 29:432–437
Stöckl B, Beerkotte J, Krismer M, Fischer M, Bauer R (1997) Results of the Müller acetabular reinforcement ring in revision arthroplasty. Arch Orthop Trauma Surg 116:55–59
Kawanabe K, Akiyama H, Onishi E, Nakamura T (2007) Revision total hip replacement using the Kerboull acetabular reinforcement device with morsellised or bulk graft: results at a mean follow-up of 8.7 years. J Bone Joint Surg 89B:26–31
Patel S, Sukeik M, Haddad FS (2013) Initial implant stability predicts migration but not failure in cementless acetabular revision with bone grafting. J Arthroplasty 28:832–837
van Haaren EH, Heyligers IC, Alexander FG, Wuisman PI (2007) High rate of failure of impaction grafting in large acetabular defects. J Bone Joint Surg 89B:296–300
Pereira GC, Kubiak EN, Levine B, Chen FS, Di Cesare PE (2007) Cavitary acetabular defects treated with morselized cancellous bone graft and cementless cups. Int Orthop 31:445–450
D’Antonio JA, Capello WN, Borden LS, Bargar WL, Bierbaum BF, Boettcher WG, Steinberg ME, Stulberg SD, Wedge JH (1989) Classification and management of acetabular abnormalities in total hip arthroplasty. Clin Orthop Relat Res 243:126–137
DeLee JG, Charnley J (1976) Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res 121:20–32
Nakashima Y, Sato T, Yamamoto T, Motomura G, Ohishi M, Hamai S, Akiyama M, Hirata M, Hara D, Iwamoto Y (2013) Results at a minimum of 10 years of follow-up for AMS and PerFix HA-coated cementless total hip arthroplasty: impact of cross-linked polyethylene on implant longevity. J Orthop Sci 18:962–968
Author’s contribution
YK designed the study. YK drafted the manuscript. YK and HO performed surgical treatment. KN, KT, TM, and HN performed managed the clinical and radiological evaluation. DS performed statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflict of interest.
Ethical approval
All procedures performed in this report were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Kokubo, Y., Oki, H., Sugita, D. et al. Long-term clinical outcome of acetabular cup revision surgery: comparison of cemented cups, cementless cups, and cemented cups with reinforcement devices. Eur J Orthop Surg Traumatol 26, 407–413 (2016). https://doi.org/10.1007/s00590-016-1763-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-016-1763-1