Abstract
Purpose
Early-onset scoliosis (EOS) has always been a challenging situation for spine surgeons. The aim of treatment is to control the direction of curve progression to allow for the complete development of lungs. Among all the growth constructs available, traditional growth rods (TGR) and magnetically controlled growth rods (MCGR) are most widely used. The MCGR has been introduced a few years back and there is a dearth of long-term follow-up studies. The purpose of this study is to compare the effectiveness of TGR and MCGR for the treatment of EOS.
Methods
All patients of EOS managed with either TGR or MCGR were included in the study. The patients managed with other methods or having follow-up < 2-years were excluded from the study. A total of 20 patients were recruited in the MCGR group and 28 patients were recruited in the TGR group. Both groups were matched by etiology, gender, pre-operative radiological parameters, and complications including unplanned surgeries.
Results
The mean age in our study was 7.90 years in the MCGR group and 7.46 years in the TGR group. The mean duration of follow-up in the MCGR group was 50.89 months and in the TGR group 94.2 months. Pre-operative cobb’s angle in the coronal plane and T1–S1 were comparable in both groups with a mean cobb’s angle of 65.4 in MCGR and 70.5 in TGR. The mean T1–S1 length in the MCGR group was 36.1cms and in the TGR group was 35.2 cms (p = 0.18). The average increase in T1–S1 length was 1.3 cm/year in the TGR group and 1.1 cm/year in the MCGR group (p > 0.05). The TGR patients underwent 186 open lengthening surgeries and 11 unplanned surgeries for various complications. The MCGR group has 180 non-invasive lengthening with only 4 unplanned returns to OT for various causes.
Conclusion
The curve correction was similar in both TGR and MCGR groups. The average T1–S1 length achieved on final follow-up was similar in both groups. The MCGR patients have attained similar correction with fewer invasive procedures and lesser complications compared to the TGR group.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Early onset scoliosis (EOS) is defined as curvature of spine > 10 degrees with onset before the age of 10 years [1]. The deformity in spine could be congenital or is the result of bone dysplasias, neuromuscular conditions, syndromes or any idiopathic condition with no gross visible defects.
EOS, if progressive, needs early intervention to reduce or stop the progression of curve, allowing the chest wall & lungs to develop adequately. Various treatment options were proposed with time. Before the introduction of implants, casting and bracing were used which had a high percentage of failure and compliance issues [2]. Paul Harrington introduced spinal implants in which the Harrington rod was used to distract on the concave side of deformity repeatedly and no fusion was done. But it had high rates of implant failure which made its use limited [3]. Few surgeons even tried fusion surgery at an early age of 4.1 years but there were high rates of reported crank-shaft phenomenon and progression of deformity [4].
The surgical treatment of EOS has evolved to a great extent with the introduction of growth friendly spinal implant systems. These systems allow spine and thorax to develop and grow without much progression of the curve. These implants are of 3 types: distraction based, guided growth and compression based [5]. The distraction-based systems are most commonly and widely used which include Traditional growing rods (TGR) and Magnetically controlled growing rods (MCGR). The MCGR has managed to overcome the biggest limitation of TGR, repeated open lengthening of the growth rods, due to which it became the implant of choice among spine surgeons. Moreover, the lengthening intervals are more frequent with MCGR which mimics the natural growth of spine. However, in certain group of patients like severe sagittal plane deformity or short stature, the use of MCGR is limited [6]. Hence, long-term follow-up with results comparing the two are required to appropriately define the indications and give optimum results to the patients.
This study aims to compare TGR and MCGR in the treatment of EOS.
Materials and methods
This is a multi-centre, single surgeon, retrospective cohort study for Early Onset Scoliosis (EOS). All patients with EOS of any aetiology, managed with growing rods, age at the time of index surgery < 10 years, and minimum follow-up of 2 years were included in the study. The patients with follow-up of less than 2 years were excluded from the study. The indications of both TGR and MCGR were same which includes all patients with age < 10 years, Cobb angle > 30˚ and thoracic height < 22 cms. All the patients were given option for both the procedures and the pros and cons of the procedures explained.
Surgical technique
The initial steps in the surgical technique for both the procedures were the same. As described by Akbarnia et al. [7], pre-decided upper and lower instrumented vertebrae was marked on the skin using fluoroscopy, after anaesthesia and positioning. Sub-periosteal exposure was done at the proximal level using midline incision and for the distal level, exposure was done using Wiltse approach [8]. Thereafter, pedicle screws were put at the lower instrumented vertebrae and hooks or pedicle screws were used for the upper vertebrae. No exposure was done in between to avoid periosteal stripping and spontaneous fusion. Then upper and lower anchors were connected by passing the rods- TGR/MCGR sub-fascially/intra-muscularly on both the sides. The spinal cord neuromonitoring was used in all cases. Wound was properly irrigated and closed in layers (Figs. 1, 2).
A case of congenital EOS managed with MCGR. a, b AP & lateral radiographs of pre-index surgery, c, d AP & lateral radiographs post-index surgery, e, f AP & lateral radiographs after 2 year follow-up, g, h AP & lateral radiographs after 5 years follow-up, i, j AP & lateral radiographs after growth rod graduation
Post-operatively, in TGR, distractions were done at 6 months interval and 3 months interval in cases of MCGR.
Patient data collection
For all patients included in our study, we have collected following parameters: aetiology, age, sex, pre-op Cobb angle in coronal plane, pre-op thoracic kyphosis, Sagittal balance, Pre-op T1–S1 length on AP whole spine roentgenogram. Then coronal Cobb angle, thoracic kyphosis, Sagittal balance, T1–S1 length was collected at immediate post-op and at final follow-up. Also, number of distraction and complications during the surgery and during follow-up were noted which also includes unplanned return to operation theatre.
Aetiologies were classified as per standard classification [9] of EOS as congenital, idiopathic, neuromuscular and syndromic. The Cobb angle was measured on AP radiograph of whole spine between cephalad end plate of upper end vertebrae and caudal end plate of lower end vertebrae of the curve. The kyphosis angle was measured on lateral radiographs between superior end-plate of T1 vertebrae and inferior end-plate of T12 vertebrae. The Sagittal balance was measured as the distance between postero-superior part of S1 vertebrae and C7 plumb line. T1–S1 length was also measured on AP radiograph, from mid-point at cephalad end plate of T1 vertebrae and mid-point at cephalad end plate of S1 vertebrae. Annual T1–S1 growth was measured as difference between average T1–S1 length at immediate post-op and at final follow-up which is divided by duration of time in years.
Final follow-up is defined as either the recent follow-up in cases where final fusion has not been done or follow-up just before fusion in cases where final fusion is done.
Appropriate statistical methods were used to compare the 2 groups. Paired t test was used for quantitative variables in the 2 groups. Statistical analysis was performed with SPSS for Windows, version 21.0.
Results
Our study population was sequential population with overlap (the TGR patients were enrolled from 2007 to 2018 and MCGR from 2013 to 2021). The MCGR group had 20 patients of EOS which includes 14 cases of congenital, 3 syndromic, and 3 idiopathic. The TGR group had 28 patients and it consists of 24 congenital, and 4 idiopathic. The MCGR group had 16 females and 4 males whereas TGR group had 19 females and 9 males. The mean pre-operative age in MCGR group was 7.9 ± 1.6 years (range, 5–10 years) and in TGR group 7.5 ± 2.5 years (range, 3–10 years) which was statistically similar (p = 0.49). The mean post-operative follow-up in MCGR patients was 50.9 months (range, 24–72 months) and in TGR group 94.2 months (range, 35–132 months). The demographic data is summarized in Table 1.
All the constructs in MCGR and TGR group were dual rod construct except one patient in MCGR where only single rod was put. The upper foundation levels lie between T1–T4 and lower foundation levels were between L1–L3 both the groups. One patient in MCGR group required lower level at Ilium as the pedicles were hypoplastic in Lumbar spine.
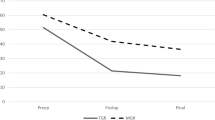
Cobb correction
The mean pre-operative Cobb angle in coronal plane was 65.4° (range, 42°–91°) in MCGR group and 70.5° (range, 28°–103°) in TGR group. The pre-operative Cobb angle was comparable in both groups (p = 0.38). The percentage correction after index surgery was 51.6% in MCGR and 58% in TGR group. On analysis, there was no statistical difference in percentage correction among the 2 groups due to index surgery (p = 0.11). On final follow-up, the percentage correction was 43% in MCGR group and 40.4% in TGR group. Though the correction obtained at final follow-up in MCGR appears to be slightly more but there was no statistical difference between 2 groups (p = 0.90). There was loss of correction in both groups between index surgery and final follow-up, but more in TGR group which can be explained with more frequent lengthening with MCGR (Table 2).
Kyphosis correction
The mean pre-operative kyphosis was 35.3° (range, 5°–87°) in TGR group and 39.2° (18°–72°) in MCGR group. The pre-operative values were comparable with no statistical difference (p = 0.22). The mean kyphosis angle in TGR group at immediate post-op and at final follow-up was 23.4° and 38.1° respectively. The difference within the group was found to be statistically significant (p = 0.0004). In MCGR group, these values were 22.1° and 10.2° respectively and was statistically significant (p < 0.00001). Hence, the difference in kyphosis at final follow-up between both groups were statistically significant.
Sagittal balance
The mean pre-op Sagittal balance in TGR group was + 1.5 cm (range, + 4.8 cm–1.3 cm). Then immediate post-op and at final follow-up, they were + 0.6 cm and + 0.9 cm.
(range, + 2.7 cm–0 cm) respectively. Similarly, in MCGR group, the mean pre-op value was + 2.9 cm (range, + 7.0 cm– − 2.8 cm). The mean immediate and final follow-up value were + 0.7 cm and + 1.1 cm (range, + 3.8 cm– − 2.4 cm) respectively. In both the groups, the overall sagittal balance tends to improve at final follow-up, better seen in TGR as compared to MCGR.
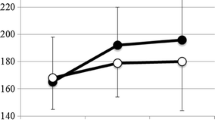
T1–S1 length
The mean pre-operative T1-S1 length in MCGR group was 25.8 cms and in TGR group was 27.6 cms (p = 0.22). When this is compared immediately after index surgery, the mean length was 30.6 cms in MCGR group and 31.6 cms in TGR group (p = 0.46). This length was again compared at final follow-up. The final follow-up is taken when the distraction of growth rods was stopped. It was 36.1 cms in MCGR and 35.2 cms in TGR (p = 0.18). The annual T1–S1 growth (obtained for the duration in which lengthening is done) was 1.1 cm/year in MCGR and 1.3 cm/year in TGR with p value > 0.05.
Unplanned return to OT and complications
At final follow-up, the 20 MCGR patients have undergone 20 index surgeries and 180 non-invasive lengthening (Table 3). Overall, there were 7 complications in MCGR group. These include 4 proximal anchor pull-outs in 3 patients, 1 distal anchor failure, and 1 patient had intra-operative respiratory complication due to which the procedure was aborted and implant was applied on an elective basis after the patient became medically fit. 1 patient had failure to distract the MCGR by the External Remote Controller. Out of these 7, there were only 4 unplanned returns to OT. In 1 patient with Neurofibromatosis, the proximal anchor was revised twice. One other patient with congenital aetiology required proximal anchor revision due to pull-out and 1 patient was taken to OT for distraction under general anaesthesia as there was failure to distract with external remote controller in OPD. Out of the 3 patients developed proximal anchor pull-out, there was development of PJK in one patient. Second patient is still under follow-up, distractions are stopped and planned for final fusion and in third patient, as mentioned above, the proximal screws were repositioned and no PJK was noticed on follow-up radiographs.
In TGR group with 28 patients, there were a total of 214 surgeries including 28 index surgeries and 186 lengthening procedures. Most of the complications were managed at the time of open lengthening. Twenty out of 28 patients experienced at least 1 complication. These include 6 proximal or distal anchor failure, 1 patient having breakage of both rods and 2 patients developing superficial infection at the proximal screw site. Two patients developed wound dehiscence and one of which required multiple plastic surgery procedures and was finally converted to Magnetic rod to avoid scar related complications (not included in MCGR group). Though most of the implant related complications were addressed during routine lengthening, there were 11 unplanned returns to OT in this group. These include 3 plastic surgery procedures in a single patient. 6 procedures were done to change or reinforce the anchors, and 2 patients required superficial debridement for infection.
Discussion
The MCGR was introduced outside USA in 2009 and was later on cleared by Food and Drug Administration (FDA) in 2014 after successful pre-clinical trials [7]. The principles of application in MCGR were same as of TGR with an advantage that the distraction can be done as an OPD procedure on awake patient without need of repeated anaesthesia. Therefore, MCGR became the choice of implant among surgeons and patients for treatment of EOS [10].
The first study of MCGR comprising of 2 cases was published by Cheung et al [11] in 2012. In it, single MCGR was applied to one patient and dual MCGR to the second. The duration of follow-up was 24 months. The cobb angle improved from 74° to 26° in first patient and 60° to 31° in second patient. The mean monthly increase in T1–T12 and T1–S1 was more than predicted natural growth. There was no intra-operative complication noted. The patient with single MCGR had loss of distraction which was attributed to implant design. Later in 2021, Cheung et al. [12] published the final outcome of same case. The patient underwent dual MCGR implantation at the age of 9 years due to suboptimal overall balance. Thereafter, successful distractions were done but she developed distal add-on in lumbar spine and final fusion was done at the age of 15 years.
Bouthors et al. [13] in 2019 published long-term results of TGR in 34 patients. The median follow-up was 6.5 years and children of idiopathic (n = 15), congenital (n = 5) and syndromic (n = 9), neuromuscular (n = 4) and dystrophic (n = 1) aetiologies were included. Only single rod was applied in all children. There was increase in T1–S1 distance by 116 mm and mean Cobb angle corrected from 55° pre-operatively to 30° at final follow-up. Since, single rod was used in all cases, hence number of complications were more in their study which includes 26 cases of rod fracture, 4 proximal junctional kyphosis, 2 proximal hook dislodgements, 2 wound infections and 1 implant prominence.
In 2014, Akbarnia et al. [14] compared 2-year follow-up of MCGR and TGR. They included 12 case matched patients in each group with neuromuscular, syndromic, idiopathic and congenital aetiology. The mean Cobb angle, T1–S1 height and T1–T12 height in MCGR group was 59°, 270 mm and 158 mm respectively which was corrected to 38° (32% correction), 307 mm and 189 mm. Similarly, in TGR group, pre-operative values were 64°, 257 mm and 158 mm which was corrected to 42° (31% correction), 342 mm and 210 mm respectively. There was no statistical difference between 2 groups pre-operatively and post-operatively (Table 4).
Our study includes 20 patients in MCGR group and 28 patients in TGR group. The patients included were sequential with overlap. Initially when MCGR was not available, all patients were managed with TGR. But later on, all patients were given options of both TGR and MCGR considering the limitations of MCGR in short stature and severe sagittal plane deformity. The mean pre-operative Cobb angle and T1–S1 length in MCGR group was 65.4° and 25.8 cms. The values in TGR group were 70.5° and 27.6 cms respectively. The aetiology included in our study were congenital, syndromic and idiopathic and both the groups were comparable. The mean follow-up in our study was 50.9 months (approx. 4.2 years) in MCGR and 94.2 months (approx. 7.9 years) in TGR group. The long duration of follow-up of TGR is obvious as we have been doing TGR even before the inception of MCGR. To the best of our knowledge, not many studies [14, 15] are available in the literature comparing the outcomes of these distraction-based techniques. The mean Cobb angle at final follow-up in MCGR group was 28.1° which is 43% correction compared to initial Cobb and in TGR it was 28.5° which amounts to 40.4% correction. The correction obtained after index surgery was 51.6% in MCGR and 58% in TGR. The possible explanation for better correction after index surgery in our series is our novel technique of using Harrington Outrigger for internal spine distraction [16]. The final mean T1–S1 length in MGCR group was 36.1 cms and in TGR was 35.2 cms. The annual T1–S1 growth in MCGR was 1.1 cm/year and in TGR 1.3 cm/year. The results were comparable in both groups.
Our study had an annual growth of 1.1 cm/year as compared to 0.81 cm/year mentioned in the study by Akbarnia et al. [14] in MCGR group. Similarly, it was 1.3 cm/year in our study and 0.97 cm/year in Akbarnia study in TGR group. Our study has growth rate similar to natural growth of spine as mentioned by Dimeglio et al. [17] which is 1 cm/year from 5 to 10 years age group. The correction achieved in TGR group in our study was lower as compared to Bouthors et al. [13]. The possible explanation could be inclusion of more congenital cases in our study which are considered stiffer compared to rest of the aetiologies. This is evident with the study published by Cengiz et al. [18] (2021) which has 14 congenital cases (Total number of cases included were 27) and the growth rate during distraction phase was similar as our study.
The sagittal parameters in growth rod implantation and during lengthening is not adequately mentioned in the literature. In study of Shah et al. [19] (2014), 43 patients were included with single or dual TGR and thoracic kyphosis and sagittal parameters were included at pre-op, after index surgery and at 2-years follow-up. The mean thoracic kyphosis pre-op was 59° which improved to 36° after index surgery. The kyphosis again increased to 51° after distraction at 2 years follow-up. There was improvement in Sagittal balance in most of the patients in the study.
Similarly, in a comparative study by Ilharreborde et al. [20] (2022), effect of MCGR on sagittal alignment was studied in 37 patients. Maximum thoracic kyphosis (− 17°, p = 0.02) and maximum lumbar lordosis (− 15°, p = 0.001) have significantly reduced. In their study, there was 40.5% incidence of mechanical failure and radiological PJK was observed in 43% of patients. They concluded that overall MCGR flattened the spine in EOS and rate of complication remained high.
Our study is concordant with literature, the mean thoracic kyphosis in pre-op was comparable in both groups. After index surgery, the mean thoracic kyphosis was reduced in both groups. Thereafter, the kyphosis was increased in TGR group and reduced significantly in MCGR group at final follow-up. In our TGR cases, we use small domino connector on each side at thoracolumbar region, where repeated lengthening is done. On the other hand, the MCGR has long actuator spanning more length of thoracic/thoracolumbar region (compared to dominos in TGR). Therefore, kyphosis of thoracic spine is better achieved in TGR as compared to MCGR after repeated lengthening. Similar results were expected with sagittal balance, but in the growing spine, the lumbar lordosis balances the thoracic kyphosis, resulting in shifting of sagittal balance to normal. Our results are concordant with the current literature, as seen in study by Erdogan et al. [21] (2019) comparing effects of sagittal parameters among TGR and MCGR where they concluded MCGR causes hypokyphosis and PJK in their 2-year follow-up.
Most of the complications in our study were implant related and by virtue of its technique, many of them were handled during planned lengthening in TGR group. Out of 28 patients in TGR, 20 patients developed at least 1 complication at the last follow-up. Majority of the complications were anchor failures, other complications being breakage of rods, superficial infection and wound related complications. There were 11 unplanned returns to OT in which one patient required multiple plastic surgery procedure to manage wound dehiscence. In MCGR group, anchor failures too make the majority of overall complications. Wound dehiscence seen in TGR was not seen in MCGR. There were 4 unplanned returns to OT of which 1 patient had distraction failure. Due to high BMI of the patient, distraction was tried under general anaesthesia so that External Remote Controller can be applied with extra force against the back. The distraction was not achieved even after that possibly due to actuator pin fracture [22, 23] or failure of internal magnet to rotate [24]. The patient was kept in regular follow-up and was converted to final fusion at skeletal maturity.
The lengthening in TGR is done mechanically because of which ‘law of diminishing results’ is valid to it. The reason behind this is that the spine becomes stiffer between proximal and distal anchor which could be because of 6-monthly lengthening protocol [25]. In MCGR, the ‘law of diminishing results’ do not apply significantly, as the lengthening frequency is more in a year which mimics the natural growth of the spine [26] Though we haven’t included data of follow-ups during lengthening period, but we observed more length gain during the initial phase in TGR which subsequently reduced on future lengthening. Whereas, the length gain in MCGR was more constant throughout which is concordant with ‘Law of diminishing results’.
There are several limitations in our study due to its retrospective nature. There is disparity in the duration of follow-up between the two groups. The overall complications are more in TGR group which may be due to its long duration of follow-up. The T1–T12 height was not taken into consideration which is a measurement for thoracic height. The sample size is also small in both the groups as this is the single surgeon study. There are more congenital cases in TGR group which may have impact when comparing final outcomes between 2 groups.
Conclusion
The MCGR and TGR can be used to manage EOS effectively and long-term results of both the techniques are comparable. The advantage of MCGR is non-invasive lengthening which reduces the need for repeated surgery on the child and has less implant related complications and less unplanned return to OT when compared to TGR. However, the MCGR causes reduction in thoracic kyphosis which results in poor sagittal balance when compared to TGR.
References
Yang S, Andras LM, Redding GJ et al (2016) Early-onset scoliosis: a review of history, current treatment, and future directions. Pediatrics 137(1):e20150709
Smith JR, Samdani AF, Pahys J et al (2009) The role of bracing, casting, and vertical expandable prosthetic titanium rib for the treatment of infantile idiopathic scoliosis: a single-institution experience with 31 consecutive patients. Clinical article J Neurosurg Spine 11(1):3–8
Moe JH, Kharrat K, Winter RB et al (1984) Harrington instrumentation without fusion plus external orthotic support for the treatment of difficult curvature problems in young children. Clin Orthop Relat Res 185:35–45
Goldberg CJ, Gillic I, Connaughton O et al (2003) Respiratory function and cosmesis at maturity in infantile-onset scoliosis. Spine 28(20):2397–2406
Skaggs DL, Akbarnia BA, Flynn JM et al (2014) Chest wall and spine deformity study group; growing spine study group; pediatric orthopaedic society of north america; scoliosis research society growing spine study committee. A classification of growth friendly spine implants. J Pediatr Orthop 34(3):260–274
Varley ES, Pawelek JB, Mundis GM Jr, Oetgen ME, Sturm PF, Akbarnia BA (2021) Pediatric spine study group; Yaszay B. The role of traditional growing rods in the era of magnetically controlled growing rods for the treatment of early-onset scoliosis. Spine Deform 9(5):1465–1472. https://doi.org/10.1007/s43390-021-00332-4
Akbarnia BA, Mundis GM (2019) Magnetically controlled growing rods in early onset scoliosis. Indications, timing and treatment. Orthopäde 48:477–485. https://doi.org/10.1007/s00132-019-03755-0
Guiroy A, Sícoli A, Masanés NG et al (2018) How to perform the Wiltse posterolateral spinal approach: technical note. Surg Neurol Int 14(9):38. https://doi.org/10.4103/sni.sni_344_17
Williams BA, Matsumoto H, McCalla DJ et al (2014) Development and initial validation of the classification of early-onset scoliosis (C-EOS). J Bone Joint Surg Am 96:1359e67
Klyce W, Mitchell SL, Pawelek J et al (2020) Characterizing use of growth-friendly implants for early-onset scoliosis: a 10-year update. J Pediatr Orthop 40(8):e740–e746. https://doi.org/10.1097/BPO.0000000000001594
Cheung KM, Cheung JP, Samartzis D et al (2012) Magnetically controlled growing rods for severe spinal curvature in young children: a prospective case series. Lancet 379(9830):1967–1974. https://doi.org/10.1016/S0140-6736(12)60112-3
Cheung JPY, Sze KY, Cheung KMC et al (2021) The first magnetically controlled growing rod (MCGR) in the world—lessons learned and how the identified complications helped to develop the implant in the past decade: case report. BMC Musculoskelet Disord 22(1):319. https://doi.org/10.1186/s12891-021-04181-0.PMID:33794851;PMCID:PMC8015050
Bouthors C, Gaume M, Glorion C et al (2019) Outcomes at skeletal maturity of 34 children with scoliosis treated with a traditional single growing rod. Spine 44(23):1630–1637. https://doi.org/10.1097/BRS.0000000000003148
Akbarnia BA, Pawelek JB, Cheung KM et al (2014) Traditional growing rods versus magnetically controlled growing rods for the surgical treatment of early-onset scoliosis: a case-matched 2-year study. Spine Deform 2(6):493–497. https://doi.org/10.1016/j.jspd.2014.09.050
Helenius IJ (2020) Standard and magnetically controlled growing rods for the treatment of early onset scoliosis. Ann Transl Med 8(2):26. https://doi.org/10.21037/atm.2019.09.72
Srivastava A, Pandita N, Gupta A et al (2023) Use of intra-operative internal distraction for the application of magnetically controlled growth rods (MCGR): a technique for maximizing correction in the rigid immature spine during index surgery. Spine Deform 11(1):225–235. https://doi.org/10.1007/s43390-022-00579-5
Dimeglio A, Canavese F (2012) The growing spine: how spinal deformities influence normal spine and thoracic cage growth. Eur Spine J 21(1):64–70. https://doi.org/10.1007/s00586-011-1983-3
Cengiz B, Ozdemir H, Sakaogullari A et al (2021) Traditional dual growing rod technique in the management of early onset scoliosis and its effects on spinal growth and lung development: the mid-term prospective results. Cureus 13(4):e14422. https://doi.org/10.7759/cureus.14422
Shah SA, Karatas AF, Dhawale AA et al (2014) The effect of serial growing rod lengthening on the sagittal profile and pelvic parameters in early-onset scoliosis. Spine 39(22):E1311-7. https://doi.org/10.1097/BRS.0000000000000565
Ilharreborde B, Ponchelet L, Sales de Gauzy J et al (2022) How does magnetically controlled growing rods insertion affect sagittal alignment in ambulatory early onset scoliosis patients? Eur Spine J 31(4):1036–1044. https://doi.org/10.1007/s00586-021-07071-0
Erdoğan S, Polat B, Atıcı Y et al (2019) Comparison of the effects of magnetically controlled growing rod and tradiotinal growing rod techniques on the sagittal plane in the treatment of early-onset scoliosis. J Korean Neurosurg Soc 62(5):577–585. https://doi.org/10.3340/jkns.2019.0094
Kwan KYH, Alanay A, Yazici M et al (2017) Unplanned reoperations in magnetically controlled growing rod surgery for early onset scoliosis with a minimum of two-year follow-up. Spine 42(24):E1410–E1414. https://doi.org/10.1097/BRS.0000000000002297
Jones CS, Stokes OM, Patel SB et al (2015) Actuator pin fracture in magnetically controlled growing rods: two cases. Spine J 16(4):e287-291. https://doi.org/10.1016/j.spinee.2015.12.020
Cheung JPY, Yiu KKL, Samartzis D et al (2017) Rod lengthening with the magnetically controlled growing rod: factors influencing rod slippage and reduced gains during distractions. Spine 43(7):E399–E405. https://doi.org/10.1097/BRS.0000000000002358
Akbarnia BA, Breakwell LM, Marks DS et al (2008) Dual growing rod technique followed for three to eleven years until final fusion: the effect of frequency of lengthening. Spine 33:984–90
Gardner A, Beaven A, Marks D et al (2017) Does the law of diminishing returns apply to the lengthening of the MCGR rod in early onset scoliosis with reference to growth velocity? J Spine Surg 3(4):525–530. https://doi.org/10.21037/jss.2017.08.16
Lampe LP, Schulze Bövingloh A, Gosheger G et al (2019) Magnetically controlled growing rods in treatment of early-onset scoliosis: a single center study with a minimum of 2-year-follow up and preliminary results after converting surgery. Spine 44(17):1201–1210. https://doi.org/10.1097/BRS.0000000000003048
Obid P, Yiu K, Cheung K et al (2021) Magnetically controlled growing rods in early onset scoliosis: radiological results, outcome, and complications in a series of 22 patients. Arch Orthop Trauma Surg 141(7):1163–1174. https://doi.org/10.1007/s00402-020-03518-z
Funding
The author did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gupta, A., Srivastava, A., Pandita, N. et al. Comparison of traditional growth rods and magnetically controlled growing rods in early-onset scoliosis: a case-matched mid term follow-up study. Eur Spine J 33, 2704–2712 (2024). https://doi.org/10.1007/s00586-024-08301-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-024-08301-x