Abstract
Purpose
To present a novel set of Left–Right Trunk Asymmetry (LRTA) indices and use them to assess the postoperative appearance of the trunk in Adolescent Idiopathic Scoliosis (AIS) patients.
Methods
We hypothesize that LRTA measurements provide complementary information to existing trunk asymmetry indices when documenting the outcome of scoliosis surgery. Forty-nine AIS patients with thoracic curves who underwent posterior spinal fusion were included. All had surface topography scans taken preoperatively and at least 6 months postoperatively. We documented spinal curvature using Radiographic Cobb angles, scoliometer readings and coronal balance. To evaluate Global Trunk Asymmetry (GTA), we used the standard measures of Back Surface Rotation (BSR) and Trunk Lateral Shift (TLS). To measure LRTA, we identified asymmetry areas as regions of significant deviation between the left and right sides of the 3D back surface. New parameters called Deformation Rate (DR) and Maximum Asymmetry (MA) were measured in different regions based on the asymmetry areas. We compared the GTA and LRTA changes with those in spinal curvature before and after surgery.
Results
The GTA indices, mainly TLS, showed improvement for more than 75% of patients. There was significant improvement of LRTA in the shoulder blades and waist regions (95% and 80% of patients respectively).
Conclusion
We report positive outcomes for LRTA in the majority of patients, specifically in the shoulder blades and waist, even when no reduction of BSR is observed. The proposed indices can evaluate local trunk asymmetries and the degree to which they are improved or worsened after scoliosis surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Adolescent Idiopathic Scoliosis (AIS) is a three-dimensional deformation of the spine leading to asymmetry of external trunk shape [1]. AIS is diagnosed in adolescents aged 10–18 years and can progress rapidly. The external deformations involve trunk imbalance and asymmetries in the shoulders, scapulae, waist, hips, and chest. Severe scoliosis can cause functional problems, e.g. cardiac and pulmonary dysfunction, and backaches [2]. Therefore, a surgical correction becomes necessary to stop progression and improve patients’ quality of life [3]. However, persistence of residual trunk asymmetry is frequent and difficult to predict by clinicians, even though correcting the apparent deformity is a major concern for patients [4].
Many studies measured trunk asymmetry at the global level (Global Trunk Asymmetry or GTA) to evaluate trunk deformity [5,6,7,8,9,10,11,12]. Research using surface topography scans documented the deformity in the coronal plane by assessing the back valley line [6] and trunk cross-sections centroid line [7]. Score and index-based methods [8, 9] were proposed, but most of them suffer from poor reproducibility as they require manual identification of landmarks on the back. Also, these works reduce the entire measurement profiles to single values, often the maxima, to indicate deformation severity. To capture local surface deformations, it is important to consider the whole measurement profiles.
Various approaches computed functional asymmetry indices from trunk cross-sections [11,12,13]. Multi-level indices were computed in [13] from the Back Surface Rotation (BSR), Trunk Rotation (TR), and coronal and sagittal trunk deviation to assess global changes between two acquisitions. To evaluate Left–Right Trunk Asymmetry (LRTA), [14] reflected a set of fixed surface points around the sagittal plane. Asss an adaptation to the scoliotic trunk, [15, 16] first computed a plane of symmetry, then evaluated LRTA by reflecting the 3D back surface points around the plane. This markerless approach visualizes the asymmetry on the whole torso instead of using 2D indices limited to specific areas, although it only provides a qualitative assessment. To analyse surgery outcome, both GTA and LRTA measurements are needed to accurately compare preoperative and postoperative trunk surfaces [17].
The objective of this study is to quantitatively assess the postoperative appearance of the trunk by using a novel set of LRTA indices combined with GTA indices, in a retrospective cohort of surgical AIS patients. We first describe the measurements used, then apply them to trunk surface data to document the outcomes in terms of trunk asymmetry.
Materials and methods
Patient data
We included a total of 49 patients who underwent posterior spinal fusion from 2009 to 2018 at our hospital by one of three orthopaedic surgeons. Inclusion criteria were: Lenke 1A main thoracic curve type, full pre-operative and post-operative trunk acquisitions taken at most 6 months before and at least 6 months after surgery. We also included 26 non-scoliotic subjects to determine a threshold value for the LRTA measurements. Our study protocol was approved by the hospital’s Research Ethics Committee. The two groups are summarized in Table 1.
Each patient was scanned using a non-invasive optical system with an accuracy of 1.1 mm [18]. Patient-specific trunk geometric models were then reconstructed using an automated method in three steps: pre-processing, registering, and merging the acquired data (Fig. 1) [19].
2D spinal measurements
We obtained 2D spinal measurements including Cobb angles for the proximal thoracic (Cobb PT), main thoracic (Cobb MT), and thoracolumbar/lumbar (Cobb TLL) spine regions in the frontal plane from each patient’s X-rays. In addition, scoliometer values in the thoracic and lumbar regions (Scoliometer_T and Scoliometer_L) and coronal balance (CB) were collected.
Global trunk asymmetry measurements
From each trunk surface model, 300 horizontal cross-sections are extracted between the L5/S1 and C7/T1 levels. Then, GTA measurements, namely BSR, TR and Trunk Lateral Shift (TLS), are computed as in [13]. To provide continuous smooth representations, cubic B-splines are fitted to these measurements.
Left–right trunk asymmetry measurements
To perform left–right asymmetry analysis, we first identify the best symmetry plane. The latter is defined as the plane that minimizes the distance between the points of the 3D trunk shape (called original trunk shape) and its reflection [15, 16] (see Fig. 2). Principal Component Analysis is applied to estimate the principal directions of the shape, then compute the symmetry plane. All points of the original shape are reflected to create a new surface on top of the original one.
Computing distance map
To encode the gap between the original trunk shape (O) and its reflection (R), a distance map is calculated as a set of local deviations. To this end, the k-d tree algorithm is used to find the nearest neighbour to each point from O on R. The deviation between the two points PO (xO, yO, zO) and PR (xR, yR, zR) is simply the Euclidean distance: \(\sqrt {\left( {x_{O} - x_{R} } \right)^{2} + \left( {y_{O} - y_{R} } \right)^{2} + \left( {z_{O} - z_{R} } \right)^{2} }\) the value is signed to indicate which surface (O or R) lies outward at that location. Different deviation ranges are visualized using a colourmap to show LRTA areas (see Fig. 3a).
Threshold for deviation maps
Because the resolution of the acquisition system is high and the acquired surfaces are noisy, and because non-scoliotic controls can also exhibit some asymmetry, we need to filter the distance maps by setting a significance threshold for the asymmetry data. We examined the range of absolute deviation values for the 26 controls at their initial and 6-month monitoring visits. These were compared to thresholds in the range 3 mm (≤ −3 mm inward and ≥ 3 mm outward) to 15 mm (≤ − 15 mm inward and ≥ 15 mm outward) (see Fig. 4). We selected a distance of 9 mm such that the majority of controls are considered non-scoliotic, while not being too high, thereby providing an adequate compromise between sensitivity and specificity.
Deformation rate
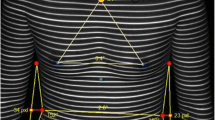
Asymmetry regions are defined as regions of the back surface where the deviation (outward or inward) between left and right sides is greater than the threshold. In Fig. 3b, left–right pairs of asymmetry regions are apparent (areas in orange or blue).
We divide the back surface into a set of slices delimited by consecutive cross-sections along the trunk. (Note that the density of slices is lower than for computing the GTA measures, as explained below.) We then define the Deformation Rate (DR) for each slice as the proportion of 3D surface points belonging to asymmetry regions:
Quantitative measurement of LRTA
We compute LRTA measurements that reveal the deformity of different areas of the back, from cervical level C6 down to lumbar level L4. This area is divided into 48 consecutive cross-sections, thus 47 slices. This number was determined experimentally to yield surgical outcome results in terms of LRTA most coherent with those from spinal measurements.
We propose the following definitions for specific regions which are of interest to researchers and clinicians. These regions correspond to the different anatomical segments seen in Fig. 5.
Region definitions
-
Waist/Lumbar: Sections 1 to 11, corresponding to vertebral levels L4 to L1;
-
Shoulder Blades/Main Thoracic: Sections 11 to 35 (T12 to T4);
-
Shoulder–Neck/Cervical & Proximal Thoracic (PT): Sections 35s to 48, (T3 to C6).
We now propose the following LRTA measurements for each region:
-
Deformation Rate (DR)
-
1.
The DR is computed for all slices in the region.
-
2.
The average DR value is also kept.
-
1.
-
Maximum Deformity (MD)
-
1.
Defined as the maximum of the DR values over all slices.
-
1.
-
Maximum Asymmetry (MA)
-
1.
For each pair of points (PO, PR) from O and R with deviation greater than the threshold, three asymmetry measures are computed: Offset =|xO|-|xR|, Height =|yO|-|yR|, and Depth =|zO|-|zR|.
-
2.
The maximum values of Offset, Height, and Depth over all slices are computed as MA of Offset, MA of Height, and MA of Depth.
-
1.
Results
AIS surgical outcome with respect to GTA and LRTA measurements
We compared 2D spinal deformity measurements with 3D trunk deformity measurements by computing GTA and LRTA indices at the preoperative and postoperative visits. To quantify changes in GTA and LRTA, we used the correction rate (CR) proposed by Seoud et al. [1]:
where \({f}_{pre}^{index}\) and \({f}_{post}^{index}\) refer to the preoperative and postoperative functional measurements of a given index. The latter can be the BSR, TR, TLS, or any of the LRTA measurements computed on individual slices. Similarly, a correction rate is defined for single measurements (Cobb angle, scoliometer, and coronal balance):
A positive (resp. negative) value of CR indicates an improvement (resp. worsening) of the deformity after surgery.
In Table 2, three clusters are identified: (1) Decreased; (2) Stable; (3) Increased deformity. At the 6-month follow-up, the Cobb MT of all 49 patients has decreased. For a majority of patients, the Cobb PT and TLL also decreased. The GTA parameters likewise decreased for most patients, but increased for several patients. For the LRTA, for most patients the DR increased in shoulder–neck but decreased in the shoulder blades and waist.
Figure 6 displays violin plots for spinal, GTA and LRTA corrections. The distributions of all Cobb angles decreased significantly. Among the GTA and LRTA corrections, TLS, DR waist and DR shoulder blades decreased, while DR shoulder–neck increased slightly.
GTA and LRTA: two example cases
We selected two patients to evaluate changes in their GTA and LRTA measurements. Figures 7 and 8 show the surgery outcome for the two exemplars. The first patient exhibits good trunk correction. The 3D trunk surface illustrates an improvement of more than 50% in CR of DR for shoulder blades and waist. Moreover, the BSR and TR curves decrease substantially (see functional plots and angular ranges at bottom of Fig. 7). By contrast, the second patient reveals poor GTA correction. In this case, the BSR and TR functional curves both increase in postop. The 3D trunk surface shows an improvement of less than 50% of DR in all regions.
The LRTA corrections are illustrated in Fig. 8 as superimposed deformation maps from the preop (light grey) and postop (dark grey) trunk shapes for the three regions. These plots display a decrease in size of the asymmetry areas from pre- to post-operative in all regions and for both cases. Thus, although the 2nd patient exhibits poor asymmetry correction in terms of GTA, the LRTA assessment indicates satisfactory surgical outcome.
Discussion
Standard spinal deformity measurements indicate good surgical correction in the MT region, while the PT and TLL Cobb angles improved for most patients but remained stable in some cases. This is as expected given that the main focus of surgery is to correct spinal deformity, and the main thoracic curvatures in our Lenke 1A cohort were all well corrected.
By contrast, the outcomes in terms of trunk deformity are mixed. Indeed, all three GTA indices increased (deteriorated) for significant subsets of patients (22%, 16% and 12% of patients for BSR, TR and TLS respectively). However, the LRTA measurements provide a more nuanced picture. In the shoulder–neck region, the DR increased for 61% of patients, but in the other two regions, the DR decreased for the vast majority (at least 80%). Thus, existing trunk asymmetry indices (BSR, TR and TLS) don’t offer a complete assessment of surgical outcome. The proposed LRTA measurements allow clinicians to document more precisely the locations where external asymmetries were corrected (or not), and to what extent.
This is illustrated by the two exemplars. For the first patient, the GTA and LRTA measures are largely in agreement. But for the second patient, despite the worsening of GTA implied by the BSR and TR functional curves, the depth maps show that in fact the asymmetry areas have diminished in the shoulders–neck and waist, and diminished somewhat in the shoulder blades.
Our findings are generally consistent with the previous study in [1]. In a similar cohort of Lenke 1A AIS patients, the authors also found that despite good spinal curvature reduction evidenced by radiographic measures and TLS, reduction of BSR was much less pronounced. This emphasizes both the difficulty in achieving good asymmetry correction in the transverse plane, and the importance of documenting treatment outcome with regard to external asymmetry.
Conclusion
We have proposed a novel set of Left–Right Trunk Asymmetry (LRTA) measurements and employed them to document the outcome of spinal surgery in a retrospective cohort of scoliosis patients. We report positive outcomes for LRTA in the majority of patients, specifically in the shoulder blades and waist regions, even when no reduction of back surface rotation is observed. The proposed method is useful to measure the effect of scoliosis surgery on local regions of the trunk. As future work, we will analyse patient self-assessment questionnaires using the LRTA measurements. This will allow surgeons to quantify the aspects of trunk appearance of most concern to patients and how the actual surgical results compare with patients’ perceptions and expectations.
References
Seoud L, Cheriet F, Labelle H, Parent S (2015) Changes in trunk appearance after scoliosis spinal surgery and their relation to changes in spinal measurements. Spine Deform 3:595–603. https://doi.org/10.1016/j.jspd.2015.05.001
Hawes M (2006) Impact of spine surgery on signs and symptoms of spinal deformity. Pediatric Rehabil 9:318–339. https://doi.org/10.1080/13638490500402264
Tones M, Moss N, Polly DW Jr (2006) A review of quality of life and psychosocial issues in scoliosis. Spine 31:3027–3038. https://doi.org/10.1097/01.brs.0000249555.87601.fc
Pratt RK, Burwell RG, Cole AA, Webb JK (2002) Patient and parental perception of adolescent idiopathic scoliosis before and after surgery in comparison with surface and radiographic measurements. Spine 27:1543–1550. https://doi.org/10.1097/00007632-200207150-00012
Patias P, Grivas TB, Kaspiris A, Aggouris C, Drakoutos E (2010) A review of the trunk surface metrics used as scoliosis and other deformities evaluation indices. Scoliosis. https://doi.org/10.1186/1748-7161-5-12
Stokes IA, Armstrong JG (1988) Spinal deformity and back surface asymmetry in idiopathic scoliosis. J Orthop Res 6:129–137. https://doi.org/10.1002/jor.1100060117
Jaremko JL, Poncet P, Ronsky J et al (2001) Estimation of spinal deformity in scoliosis from torso surface cross sections. Spine 26:1583–1591. https://doi.org/10.1097/00007632-200107150-00017
Minguez M, Buendia M, Cibrian R et al (2007) Quantifier variables of the back surface deformity obtained with a noninvasive structured light method: evaluation of their usefulness in idiopathic scoliosis diagnosis. Eur Spine J 16:73–82. https://doi.org/10.1007/s00586-006-0079-y
Suzuki N, Inami K, Ono T et al (1999) Analysis of posterior trunk symmetry index (POTSI) in scoliosis. Stud Health Technol Inform. https://doi.org/10.3233/978-1-60750-903-5-81
Pazos V, Cheriet F, Danserau J et al (2007) Reliability of trunk shape measurements based on 3-D surface reconstructions. Eur Spine J 16:1882–1891. https://doi.org/10.1007/s00586-007-0457-0
Jaremko JL, Poncet P, Ronsky J et al (2002) Indices of torso asymmetry related to spinal deformity in scoliosis. Clin Biomech 17:559–568. https://doi.org/10.1016/s0268-0033(02)00099-2
Ajemba PO, Durdle N, Raso VJ (2009) Characterizing torso shape deformity in scoliosis using structured splines models. IEEE Trans Biomed Eng 56:1652–1662. https://doi.org/10.1109/TBME.2009.2020333
Seoud L, Dansereau J, Labelle H, Cheriet F (2012) Multilevel analysis of trunk surface measurements for non-invasive assessment of scoliosis deformities. Spine 37:1045–1053. https://doi.org/10.1097/BRS.0b013e3182575938
Goldberg CJ, Grove D, Moore DP et al (2006) Surface topography and vectors: a new measure for the three-dimensional quantification of scoliotic deformity. Stud Health Technol Inform 123:449–455
Komeili A et al (2014) Surface topography asymmetry maps categorizing external deformity in scoliosis. Spine J: Off J North Am Spine Soc 14:973–983. https://doi.org/10.1016/j.spinee.2013.09.032
Komeili A et al (2015) Monitoring for idiopathic scoliosis curve progression using surface topography asymmetry analysis of the torso in adolescents. Spine J 15:743–751. https://doi.org/10.1016/j.spinee.2015.01.018
Ahmad O, Lombaert H, Parent S, Labelle H, Cheriet F (2018) Spectral shape analysis of human torsos: application to the evaluation of scoliosis surgery outcome. IEEE J Biomed Health Inform 22:1552–1560. https://doi.org/10.1109/JBHI.2017.2759804
Pazos V, Cheriet F, Song L et al (2005) Accuracy assessment of human trunk surface 3D reconstructions from an optical digitising system. Med Biol Eng Comput 43:11–15. https://doi.org/10.1007/BF02345117
Adankon M, Chihab N, Dansereau J, Labelle H, Cheriet F (2013) Scoliosis follow-up using noninvasive trunk surface acquisition. IEEE Trans Biomed Eng 60:2262–2270. https://doi.org/10.1109/TBME.2013.2251466
Acknowledgements
This work was funded by the Canadian Institutes of Health Research (CIHR) and the TransMedTech Institute. The authors thank the personnel of the Orthopaedics Research Clinical Unit (URCO, CHU Sainte-Justine) for their help with collecting clinical data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Khani, M., Debanné, P., Guibault, F. et al. Automatic assessment of scoliosis surgery outcome on trunk shape using left–right trunk asymmetry. Eur Spine J 33, 1691–1699 (2024). https://doi.org/10.1007/s00586-023-08122-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-08122-4