Abstract
Purpose
This study aimed to analyze the overall incidence of cardiac abnormalities in patients with congenital scoliosis and the possible influencing factors.
Methods
PubMed, Embase, and Cochrane Library were searched for relevant studies. The quality of the studies was assessed independently by two authors using the methodological index for nonrandomized studies (MINORS) criteria. The following data were extracted from the included studies: bibliometric data, number of patients, number of patients with cardiac anomalies, gender, types of deformity, diagnostic method, type of cardiac anomaly, location, and other associated anomalies. The Review Manager 5.4 software was used to group and analyze all the extracted data.
Results
This meta-analysis included nine studies and identified that 487 of 2,910 patients with congenital vertebral deformity had cardiac anomalies diagnosed by ultrasound (21.05%, 95% CI of 16.85–25.25%). The mitral valve prolapse was the most frequent cardiac anomaly (48.45%) followed by an unspecified valvular anomaly (39.81) and an atrial septal defect (29.98). A diagnosis of cardiac anomalies was highest in Europe (28.93%), followed by USA (27.21%) and China (15.33%). Females and formation defects were factors significantly associated with increased incidence of cardiac anomalies: 57.37%, 95% CI of 50.48–64.27% and 40.76%, 95% CI of 28.63–52.89%, respectively. Finally, 27.11% presented associated intramedullary anomalies.
Conclusions
This meta-analysis revealed that the overall incidence of cardiac abnormalities detected in patients with congenital vertebral deformity was 22.56%. The incidence rate of cardiac anomalies was higher in females and those with formation defects. The study offers guidance for ultrasound practitioners to accurately identify and diagnose the most common cardiac anomalies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Congenital scoliosis is a spinal deformity present at birth and characterized by formation, segmentation, or mixed defects [1]. The spine is formed between four and six weeks—the crucial stage when associated anomalies could develop [2, 3]. Of these associated anomalies, intraspinal ones are characterized best, with no relationship with the type of spinal deformity, the level of hemivertebra, or gender [4].
Few studies have reported on the incidence of congenital heart disease associated with congenital scoliosis and whether there are risk factors that increase its incidence or whether it actually presents a risk in surgery. In addition, the studies include different populations. The knowledge of these data could lead to an “appropriate conversation with patients and families” and the establishment of a diagnostic algorithm showing the necessary imaging tests [5].
The diagnosis of cardiac anomalies could affect their prognosis. On the other hand, it has been observed that the diagnosis of intraspinal anomalies does not affect scoliosis correction, and there might not be an association between multiple intraspinal anomalies and previous correction surgery [6, 7].
In contrast, studies analyzing the risk of cardiac anomalies in spinal surgery tend to be case series and case reports showing high risk in patients undergoing Fontan or single ventricle surgery. Complications include pleural effusion, blood loss, and fluid management issues. There is a correlation between the high surgical risk and the magnitude of the curve, fused levels, surgery time, and cyanosis [8, 9]. This is why a diagnosis is crucial to optimize the patient’s condition before spinal correction surgery. Nowadays, there are more accurate diagnostic methods, such as echocardiography and magnetic resonance imaging (MRI), included in some cases as a diagnostic algorithm for patients with congenital scoliosis.
There is no meta-analysis describing the true incidence of cardiac anomalies in individuals with congenital scoliosis. Also, no meta-analysis indicates the most evidence-based risk factors. The present study aimed to investigate the incidence of cardiac anomalies in patients with congenital scoliosis and to assess which factors increase the occurrence of these abnormalities.
Material and methods
Eligibility criteria
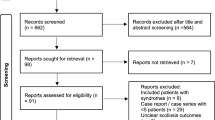
This meta-analysis followed the PRISMA guidelines (Fig. 1) [10]. The study selection was done by two reviewers, who reached an agreement by discussion. We followed the PICOS strategy: (P) Patients with congenital scoliosis were studied. (I) This meta-analysis analyzed incidences with no intervention. (C) This meta-analysis analyzed incidences without comparison. (O) The outcomes were incidence of cardiac anomalies. (S) The studies were cohort studies. The exclusion criteria were: prenatal ultrasound diagnosis, noncongenital scoliosis, and duplicate data.
Information sources and search strategy
The databases PubMed (National Library of Medicine) and the Cochrane Collaboration Library were searched from 2000 to 2020. The selected articles were about cardiac anomalies associated with congenital scoliosis. The search terms were “congenital scoliosis” or “congenital vertebral deformit*” and “heart anomalies” or “heart abnormalities” or “cardiac anomalies” or “cardiac abnormalities.” The references of the first studies included were reviewed.
Data extraction and data items
Data extraction was performed by two reviewers using an Excel spreadsheet. If an agreement was not achieved, a third reviewer was asked to complete the data extraction form. For each study that met the criteria, the following information was extracted: The primary pooled outcome measure was the incidence of cardiac anomalies in individuals with congenital scoliosis. Demographic variables were also collected: author, years of publication, region, age, gender of the overall population, number of patients, and diagnosis. Information on the gender of those who experienced cardiac anomalies, the type of malformation (formation, segmentation, or mixed), and other associated anomalies were gathered as well.
Risk of bias assessment
The quality of the included studies was assessed independently by two authors using the Methodological Index for Non-Randomized Studies (MINORS) criteria [11]. The maximum score is 24 for comparative studies and 16 for noncomparative studies. For noncomparative studies, scores of 0–4 corresponded to very low quality, 5–7 corresponded to low quality, 8–12 corresponded to fair quality, and ≥ 13 corresponded to high quality. For comparative studies, scores of 0–6 corresponded to very low quality, 7–10 corresponded to low quality, 11–15 corresponded to fair quality, and ≥ 16 corresponded to high quality.
Assessment of the results
The incidence of cardiac anomalies was calculated as the total number of patients with congenital cardiac anomalies divided by the total number of patients with congenital scoliosis. In studies in which the standard error (SE) was not reported, we calculated it from the prevalence using the following formula: SE = √p(1–p)/n and 95% CI = p ± 1.96xSE, where p = prevalence [12]. Pooled incidences with 95% confidence intervals (CIs) were calculated using a random-effects model. A fixed-effects model was used if heterogeneity was low (I2 < 50%). Otherwise, a random-effects model was used. All analyses were performed using the Review Manager 5.4 software package provided by the Cochrane Collaboration.
Additional analysis
Subgroup analyses were performed using the following variables: mean age and region of the studies. Funnel plots were used to examine the possibility of publication bias.
Results
Study selection
The initial search identified 48 results. After eliminating case reports and reviews, 13 articles were excluded. The titles and abstracts of the remaining 35 articles were then examined. Six studies met the inclusion criteria. After an in-depth analysis of these articles, three more were included based on the references cited in the six studies (Fig. 1).
Study characteristics
The main characteristics of the included articles are shown in Table 1 [5, 13,14,15,16,17,18,19,20]. A total of nine studies involving 2910 patients were included. The articles were published between 2002 and 2020. The age of the patients ranged from 3.5 to 14.9 years. The methodological index for nonrandomized studies (MINORS) assessment ranged between 10 and 12 points. According to the MINORS criteria, the studies were of fair quality.
Outcomes
The incidence rate of cardiac anomalies associated with congenital scoliosis was 21.05%, with 95% CI of 16.85–25.25% (Fig. 2). The incidence rates of these anomalies according to region were as follows: Europe, 28.93% (95% CI of 9.22–48.64%); USA, 27.21% (95% CI of 19.97–34.45%); and China, 15.33% (95% CI of 13.28–17.37%) (Fig. 3). Cardiac anomalies were diagnosed more frequently in patients over 10 years (24.29%, 95% CI of 19.02–29.57%) than in patients under 10 years (14.57%, 95% CI of 5.80–23.34%) (Fig. 4).
Table 2 shows the cardiac abnormalities. Mitral valve prolapse was the most frequent cardiac anomaly, occurring in 48.45% of patients. The second most frequent anomaly was nonspecific valvular anomalies, representing 29.98% of the patients. The third most frequent abnormality was atrial septal defect (ASD), found in 29.98% of the patients. The other anomalies found were atrial septal aneurysm (24.42%), ventricular septal defect (VSD) (21.08%), patent foramen ovale (13.95%), Fallot tetralogy (10.87%), PDA (10.63%), dilation coronary sinus (8.47%), and dextrocardia (3.77%).
With respect to gender, cardiac anomalies occurred more frequently in females than in males (57.37%, 95% CI of 50.48–64.27% vs. 42.65%, 95% CI of 36.05–49.25%) (Fig. 5). There were significant differences, with cardiac anomalies being more frequent in females. Regarding the type of malformation, the incidence rates of cardiac anomalies related to formation, segmentation, and mixed defects were 40.76% (95% CI of 28.63–52.89%), 20.20% (95% CI of 12.75–27.65%), and 24.33% (95% CI of 10.53–38.14%), respectively (Fig. 6). Patients with formation defects showed a significantly higher incidence of cardiac anomalies than those with segmentation defects. Finally, the incidence of intraspinal anomalies with cardiac anomalies was 27.11%, (95% CI of 3.24–50.98%) (Fig. 7).
Discussion
This meta-analysis showed that the overall incidence of cardiac anomalies in patients with congenital scoliosis was 21.05%. It was also observed that females presented a higher incidence of cardiac anomalies. Regarding the type of malformation, those with formation defects showed a higher incidence of cardiac abnormalities. The regions with the highest incidence were Europe and USA, followed by China. Intramedullary anomalies were present in almost one-third of the patients with cardiac anomalies. The quality of the studies was consistent.
Many studies presented diagnoses of new cardiac anomalies through the protocol [5]. Therefore, the incidence could be underestimated in retrospective studies. Some of the patients diagnosed during the study were treated for the anomalies [5]. This highlights the importance of the diagnosis of cardiac anomalies. In addition, all studies used echocardiography, so training in this procedure is crucial. Furdock et al. [5] proposed to perform echocardiography in patients with mixed defects and congenital kyphosis [5]. Intraspinal defects were also associated with congenital kyphosis [13]. In our study, the formation defects presented a higher risk for cardiac anomalies. On the other hand, Reckles et al. [21] performed echocardiography on patients who were going to undergo surgery and found cardiac anomalies in 10% of these patients [21]. In our analysis, only three studies discussed whether patients with congenital scoliosis underwent surgery [5, 15, 16]. Bozcali et al. [16] also strongly recommended routine echocardiography for patients with idiopathic and congenital scoliosis [16]. Regarding whether cardiac anomalies represent a risk, the literature supports intraoperative and postoperative risks. Severe correction has been associated with cardiopulmonary decompensation. Renal anomalies have also been associated with metabolic disturbances [22].
In our study, it was observed that the females presented a higher incidence of cardiac anomalies, and formation defects were the most frequent associated defect. In a meta-analysis of the incidence and characteristics of intraspinal anomalies, no differences were observed in terms of gender or type of malformation [4]. The location could not be analyzed because it was not reported in the articles. Bollini et al. [15] observed that the incidence of cardiac anomalies were greater when the location of the deformity was the thoracic region [15]. In addition, the relationship between cardiac and intraspinal anomalies was well established. Bollini et al. [15] also established the relationship between cardiac abnormalities and urogenital, gastrointestinal, and ocular anomalies [15]. Sevencan et al. [19] observed that up to 57.9% of patients had associated intraspinal anomalies [19]. On the other hand, cardiopulmonary mortality increased due to the progression of untreated curves [23]. These cardiopulmonary changes caused by deformity, such as right ventricular alteration and cor pulmonale, negatively affect patients with cardiac anomalies, especially those affecting the right heart [23]. Some articles specified the type of risk for each anomaly. Patients with Fontan circulation showed altered coagulation, and patients with single ventricle defects showed increased bleeding due to higher venous pressures [8, 24, 25].
A prenatal diagnosis of anomalies could also be done. The mean incidence found in these articles was 25.97% (95% CI of 7.36–44.58%) [26,27,28,29]. Further, the most frequent anomalies were an abnormal cardiac axis, double-outlet right ventricle, tetralogy of Fallot, ASD, and VSD [26,27,28,29]. The incidence of valvular anomalies was lower in the diagnosis of prenatal cardiac anomalies than in the postnatal diagnosis included in our study. Therefore, efforts in postnatal ultrasound could be made to find or focus on this type of anomalies, especially mitral valve prolapse.
This study had several limitations. Maternal or familial risk factors could not be analyzed because they were not collected in the individual studies. In addition, there was high heterogeneity. On the other hand, the incidence data is determined by the practitioner’s ultrasound experience. Also, it is to be expected that children with a severe heart disease may die earlier and the incidence may be underestimated. Moreover, not all studies presented diagnostic algorithms. Some performed ultrasound on all children, some on those who were going to undergo surgery, and some on those who fulfilled certain characteristics; other studies did not specify.
Conclusion
The incidence rate of cardiac anomalies in patients with congenital scoliosis was 21.05%, with mitral valve prolapse being the most frequent. The incidence was higher in Europe. Cardiac anomalies increased in females and in those with formation defects. Future studies should focus on whether cardiac abnormalities actually increase the risk of spinal surgery. Further studies are also needed to stratify by type of deformity, identify which factors lead to an increased risk, and study maternal risk factors by region or according to different biomarkers linked directly to risk factors. This study could provide guidance to ultrasound practitioners in identifying the most frequent cardiac anomalies, facilitating their detection and diagnosis with greater accuracy.
References
Weiss HR, Moramarco M (2016) Congenital scoliosis (mini-review). Curr Pediatr Rev 12(1):43–47. https://doi.org/10.2174/1573396312666151117121011
Pahys JM, Guille JT (2018) What’s new in congenital scoliosis? J Pediatr Orthop 38:e172–e179. https://doi.org/10.1097/BPO.0000000000000922
Hedequist D, Emans J (2007) Congenital scoliosis. A review and update. J Pediatr Orthop 27:106–116. https://doi.org/10.1097/BPO.0b013e31802b4993
Wang X, Yu Y, Yang N et al (2020) Incidence of intraspinal abnormalities in congenital scoliosis: a systematic review and meta-analysis. J Orthop Surg Res 15(1):485. https://doi.org/10.1186/s13018-020-02015-8
Furdock R, Brouillet K, Luhmann SJ (2019) Organ system anomalies associated with congenital scoliosis: a retrospective study of 305 patients. J Pediatr Orthop 39(3):e190–e194. https://doi.org/10.1097/BPO.0000000000001279
Yang N, Luo M, Zhao S et al (2021) Is it safe and effective to correct congenital scoliosis associated with multiple intraspinal anomalies without preliminary neurosurgical intervention? Medicine (Baltimore) 100(10):e24030. https://doi.org/10.1097/MD.0000000000024030
Zhao Q, Shi B, Sun X et al (2019) Do untreated intraspinal anomalies in congenital scoliosis impact the safety and efficacy of spinal correction surgery? A retrospective case-control study. J Neurosurg Spine 31(1):40–45. https://doi.org/10.3171/2019.1.SPINE181205
Cohen LL, Przybylski R, Marshall AC et al (2021) Surgical correction of scoliosis in children with severe congenital heart disease and palliated single ventricle physiology. Spine 46(14):791–796. https://doi.org/10.1097/BRS.0000000000003905
Przybylski R, Hedequist DJ, Nasr VG et al (2019) Adverse perioperative events in children with complex congenital heart disease undergoing operative scoliosis repair in the contemporary era. Pediatr Cardiol 40(7):1468–1475. https://doi.org/10.1007/s00246-019-02169-1
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6(7):e1000100. https://doi.org/10.1371/journal.pmed.1000100
Slim K, Nini E, Forestier D et al (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 73(9):712–716. https://doi.org/10.1046/j.1445-2197.2003.02748.x
Allagh KP, Shamanna BR, Murthy GV et al (2015) Wellcome Trust- PHFI Folic Acid project team. Birth prevalence of neural tube defects and orofacial clefts in india: a systematic review and meta-analysis. PLoS ONE 10(3):e0118961. https://doi.org/10.1371/journal.pone.0118961
Basu PS, Elsebaie H, Noordeen MH (2002) Congenital spinal deformity: a comprehensive assessment at presentation. Spine 27(20):2255–2259. https://doi.org/10.1097/00007632-200210150-00014
Beauregard-Lacroix E, Tardif J, Camurri MV et al (2017) retrospective analysis of congenital scoliosis: associated anomalies and genetic diagnoses. Spine 42(14):E841–E847. https://doi.org/10.1097/BRS.0000000000001983
Bollini G, Launay F, Docquier PL et al (2010) Congenital abnormalities associated with hemivertebrae in relation to hemivertebrae location. J Pediatr Orthop B 19(1):90–94. https://doi.org/10.1097/BPB.0b013e3283327f57
Bozcali E, Ucpunar H, Sevencan A et al (2016) A retrospective study of congenital cardiac abnormality associated with scoliosis. Asian Spine J 10(2):226–230. https://doi.org/10.4184/asj.2016.10.2.226
Lin G, Chai X, Wang S et al (2021) Cross-sectional analysis and trend of vertebral and associated anomalies in chinese congenital scoliosis population: a retrospective study of one thousand, two hundred and eighty nine surgical cases from 2010 to 2019. Int Orthop 45(8):2049–2059. https://doi.org/10.1007/s00264-021-05061-x
Liu YT, Guo LL, Tian Z et al (2011) A retrospective study of congenital scoliosis and associated cardiac and intraspinal abnormities in a Chinese population. Eur Spine J 20(12):2111–2114. https://doi.org/10.1007/s00586-011-1818-2
Sevencan A, Misir A, Ucpunar H et al (2019) The incidence and interrelationship of concomitant anomalies in congenital scoliosis. Turk Neurosurg 29(3):404–408. https://doi.org/10.5137/1019-5149.JTN.24429-18.2
Shen J, Wang Z, Liu J et al (2013) Abnormalities associated with congenital scoliosis: a retrospective study of 226 Chinese surgical cases. Spine 38(10):814–818. https://doi.org/10.1097/BRS.0b013e31827ed125
Reckles LN, Peterson HA, Weidman WH et al (1975) The association of scoliosis and congenital heart defects. J Bone Jt Surg Am 57:449–455
Dhuper S, Ehlers KH, Fatica NS et al (1997) Incidence and risk factors for mitral valve prolapse in severe adolescent idiopathic scoliosis. Pediatr Cardiol 18(6):425–428. https://doi.org/10.1007/s002469900220
Li XY, Li Z, Feng F et al (2016) Correlation between severity of adolescent idiopathic scoliosis and pulmonaryartery systolic pressure: a study of 338 patients. Eur Spine J 25(10):3180–3185. https://doi.org/10.1007/s00586-016-4471-y
Kadhim M, Spurrier E, Thacker D et al (2014) Scoliosis surgery in children with congenital heart disease. Spine 39(3):E211–E218. https://doi.org/10.1097/BRS.0000000000000083
Tsirikos AI, Augustithis GA, McKean G et al (2020) Cyanotic congenital cardiac disease and scoliosis: pre-operative assessment, surgical treatment, and outcomes. Med Princ Pract 29(1):46–53. https://doi.org/10.1159/000501840
Lemire GT, Beauregard-Lacroix É, Campeau PM et al (2020) Retrospective analysis of fetal vertebral defects: associated anomalies, etiologies, and outcome. Am J Med Genet A 182(4):664–672. https://doi.org/10.1002/ajmg.a.61468
Goldstein I, Makhoul IR, Weissman A et al (2005) Hemivertebra: prenatal diagnosis, incidence and characteristics. Fetal Diagn Ther 20(2):121-126. https://doi.org/10.1159/000082435
Wax JR, Watson WJ, Miller RC et al (2008) Prenatal sonographic diagnosis of hemivertebrae: associations and outcomes. J Ultrasound Med 27(7):1023–1027. https://doi.org/10.7863/jum.2008.27.7.1023
Basude S, McDermott L, Newell S et al (2015) Fetal hemivertebra: associations and perinatal outcome. Ultrasound Obstet Gynecol 45(4):434–438. https://doi.org/10.7863/jum.2008.27.7.1023
Funding
No funding was received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or nonfinancial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bas, J.L., Pérez, S., Rubio, P. et al. Incidence of cardiac anomalies in congenital vertebral deformity: systematic review and meta-analysis of 2910 patients. Eur Spine J 32, 2967–2974 (2023). https://doi.org/10.1007/s00586-023-07817-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07817-y