Abstract
Background
The growth and development of the atlas in children has not been studied to date using a large sample size.
Objective
To study whether a 3.5-mm screw is suitable for the atlas in children, to explore the anatomical size and development of the atlas in 0–14-year-old children, and to provide morphological basis for lateral mass screw internal fixation.
Methods
A Computed Tomography (CT) morphometric analysis was performed on 420 pediatric atlases. In the atlas, D1, D2, D3, D4, and α of the atlas lateral mass were measured. Statistical analysis was performed using one-way ANOVA and Students’ t test. The least square method was used for the regression analysis of the change trend in anatomical structure. The curve with the greatest goodness of fit was used as the anatomic trend regression curve.
Results
D1, D2, D3, and D4 generally showed an increasing trend with age. The ranges of averages of D1, D2, D3, D4, and α in 0–14 year-old children were as follows: 4.576–9.202 mm, 9.560–25.100 mm, 3.414–10.554 mm, 11.150–27.895, and 12.41°–20.97°, respectively. The trends of the fitting curves of L1 and L3 were power functions, and those of L2 and L4 were logarithmic curves.
Conclusions
CT examination could help in preoperative decision-making, and 3.5-mm screw was found to be suitable for lateral mass screw internal fixation in children aging 2 years and older. D1–D4 increased with age. This provided a certain reference to perform posterior atlantoaxial fusion in children and is of great significance to design posterior atlantoaxial screw in children.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The cervical vertebra 1 (C1) is also called as the atlas. Atlantoaxial fusion internal fixation usually consists of atlas lateral pedicle mass screw and C2 pedicle screw. Because of its good biomechanical properties and wide range of surgical indications, it has been widely used in clinical practice [1,2,3,4,5]. However, the anatomical structure of the atlas is complex, and there is a risk of damaging the surrounding important nerves and blood vessels when the lateral pedicle mass screw is inserted, which can lead to serious complications.
Adult C1 is mature and relatively stable. Previous studies have explained the complex anatomy of C1 in adults in detail [6,7,8]. Children’s cervical spine is in the stage of continuous growth and development, and various anatomical diameters are much smaller than those of adults. No particular screw fixation device is used for children in south China. The currently available pedicle screw with the smallest diameter is a screw rod system for adult cervical spine lateral mass or pedicle fixation, and the screw diameters are 3.2, 3.5, and 4.0 mm. The age from which the atlas lateral mass screw can be inserted in children and the screw sizes and their suitability for a particular age of children have been some unanswered questions and are concerns for clinicians.
In this study, we measured the anatomical size of the atlas lateral mass in south Chinese children aging 0–14 years, assessed whether 3.5-mm screw is suitable for the atlas in children, and studied the development of the atlas in children. This could provide a guidance for designing screws for children and a morphological basis for lateral mass screw internal fixation.
Methods
Overall, 64-slice CT scans (Somatom Sensation 64, Siemens, Germany) of the neck in the outpatient and inpatient clinics at the First Affiliated Hospital of Guangxi Medical University were retrospectively analyzed. This included children who needed neck examination due to trauma, oesophageal foreign body, headache, or other cervical examinations. Cases of cervical spine osteophytes, deformities, tumors, fractures, and other anatomical abnormalities were excluded. Age of children ranged from 0 to 14 years, regardless of sex. Finally, 30 cases of each age were randomly selected, and data from a total of 420 children were selected for the further assessments. Because of the retrospective nature of the study, informed consent was waived. The study was approved by the Ethics Committee of the First Affiliated Hospital of Guangxi Medical University.
Based on the method descript in previous studies [9,10,11] and the Picture Archiving and Communication Systems [12], lines a and b were determined after selecting horizontal and coronal planes, respectively: line a represents the line between two points lateral to the spinal canal. whereas line b represents the line passing through the inner wall of the foramina and is parallel to line a. A total of five parameters, namely D1, D2, D3, D4, and α, were measured. The definition of these parameters is as follows: (1) D1: the shortest distance from the inner wall of the vertebral artery foramen to the outer wall of the spinal canal, that is, the distance between lines a and b. (2) D2: the distance between the midline of the long axis of the lateral mass and the inner cortex of the front and rear edges of the lateral mass, that is, the distance between the midline between lines a and b and the intersection point of the front and rear edge of the lateral mass. (3) D3: the height of the lateral mass, that is, the distance between the inner cortex in the middle of the lateral mass. (4) D4: the distance from the midpoint of the pedicle to the medial cortex of the anterior edge of the lateral mass. (5) α: the inclination angle of the lateral mass, that is, the angle between D2 and the sagittal plane. Both sides were measured simultaneously, and ‘L’ and ‘R’ were marked on the left and right, respectively (Fig. 1, Supplement 1). All parameters were measured by three senior personnel simultaneously, and the average was taken. Finally, a 3.5-mm screw simulation was placed on the atlas using Mimics Research 19.0.
Computed tomography (CT) image of a child aging 12 years and 3 months. A, localization of coronal plane in the horizontal plane. B, localization of horizontal plane in the coronal plane. C–E, schematic diagram of the measurement of anatomical indices. Line a, the line between two points lateral to the spinal canal. Line b, the line passing through the inner wall of the foramina and parallel to line a. D1, the distance between lines a and b. D2, the distance between the midline between lines a and b and intersection point of the front and rear edge of the atlas lateral mass. D3, the distance between the midpoint of the upper and lower edges of the lateral mass. D4, the distance between the anterior margin of the lateral mass and midpoint behind the pedicle
Statistical analysis was performed using one-way ANOVA and students’ t test, and the regression analysis was conducted using the least-square method. These tests were performed using Statistical Package for Social Sciences (SPSS, version 22). The average, standard deviation of each index, and fitting analysis were obtained. P < 0.05 was considered significant. The regression analysis figures were drawn using GraphPad v8.0.2. In addition, the lengths of each indicator in each age group were displayed by drawing violin plots in R × 64 4.0.5.
Results
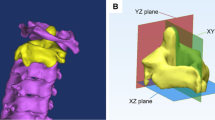
In this study, we measured C1 anatomical data in south Chinese children aging 0–14 years. Overall, 30 children from each age group were randomly selected, and data from a total of 420 children were assessed, irrespective of sex. We measured the mean and standard deviation of each indicator parameter on the left, right, and bilateral sides. The measures of D1, D2, D3, D4, and α are shown in Supplement 2. Except for some anatomical indicators that were different between the left and right in individual age groups, most of the indicators were not significantly different in all age groups. From 0 to 14 years, the averages of D1, D2, D3, and D4 ranged from 4.576 to 9.202, 9.560 to 25.100, 3.414 to 10.554, and 11.150 to 27.895 mm, respectively. The range of α was from 12.41° to 20.97°. The changing trends of D1–D4 with age were fitted to the relevant curve using the least-square method (Fig. 2). The changing trends of D1 and D3 with age conformed to the Power function curve, whereas the those of D2 and D4 conformed to the logarithmic function curve. However, α did not fit with any suitable curve (Not shown). The violin plots clearly showed the range of fluctuations of these parameters and their trends with age (Fig. 3). In addition, to verify the measured data and conclusions, the three-dimensional atlas of a child aged 2 years and 3 months was reconstructed with CT DICOM data in Mimics Research 19.0, and a screw sized 3.5 × 19 mm was simulated and inserted into the lateral mass of the atlas (Fig. 4). The simulated images showed that the insertion of a 3.5-mm screw into the lateral mass of the atlas could perform well.
Clinical case presentation
After the imaging studies, we performed atlantoaxial fusion on two children with atlantoaxial dislocation, and the symptoms of the patients disappeared gradually after the operation. The first patient, a female (7 years and 9 months old), was admitted to the hospital because of torticollis of the neck with limited mobility for more than 2 months. The second patient, a male (9 years and 1 month old), was admitted to the hospital because of neck pain and limited activity caused by high fall injury for 3 months. The preoperative and postoperative cervical imaging examinations of these two pediatric patients are shown in Figs. 5, 6.
The CT images of the cervical spine of a child aging 7 years and 9 months. A, preoperative sagittal CT image of the cervical spine; B, preoperative horizontal CT images of the cervical spine; C, preoperative 3D reconstruction of the cervical spine; D, postoperative sagittal CT images of the cervical spine; E, postoperative image of atlas level; F, postoperative horizontal image of the axis
The CT images of the cervical spine of a child aging 9 years and 1 month. A, preoperative sagittal CT image of cervical spine; B, preoperative horizontal CT images of the cervical spine; C, preoperative 3D reconstruction of the cervical spine; D, postoperative sagittal CT images of the cervical spine; E, postoperative image of atlas level; F, postoperative horizontal image of the axis
Discussion
The upper cervical spine includes the atlas and axial vertebrae. Fusion surgery for the upper cervical spine has undergone many changes over a long period. Previous posterior cable [3, 13] and lamina clamp [14] techniques were abandoned because of space occupation in the spinal canal and compression of the spinal cord. With the advent of the Magerl screw fixation technique [15], fusion rates and biomechanics have been greatly improved [16, 17]; however, the incidence of vertebral artery injury is relatively high. In 1994, Goel et al. [18] reported the technique of posterior atlantoaxial fusion. Harms [19] and Resnick [20] improved the posterior atlantoaxial fusion technique, and it is still widely used. The atlas pedicle screw is another screw fixation technique following the atlas lateral mass screw [21, 22].
The children in the age group of 0–14 years are in the stage of growth and development, and their cervical activity is much different from that of adults. The cervical ligamentous laxity and incomplete develop articular process of joint can easily lead to cervical spine injury [23]. Children being active and having immature bones further increases their risk of having cervical injuries, such as cervical spine fracture and dislocation, which mainly occur in the supper cervical spine [23, 24]. In addition, because of the effects of Down syndrome, Griesel syndrome, joint dislocation, and ligament injury, some children require upper cervical spine surgery [25,26,27]. For surgical treatment of the upper cervical spine in children, good treatment options are still unavailable. The current approach is to use posterior pedicle lateral mass screws and cervical screws for adults. However, no screws have been developed specifically for the atlas in children from south China, and the reports on posterior atlas surgery in children are limited. The purpose of this study was to provide a certain anatomical basis for posterior atlantoaxial fusion in children, ideas for the design of the surgical plan, and a reference for designing pedicle screw specifications for children.
Numerous studies have measured the anatomy of the lateral mass of the atlas in children. However, there were some limitations such as undetailed age groups, small age span, or a small number of cases studied [9, 10, 28,29,30], and their conclusions were not consistent with each other. Thus, to further study the anatomies of atlas lateral mass, we analyzed CT images of atlas lateral mass in children aged 0–14 years in south China. Our study showed that D1–D4 increased at a slower rate with age, and they increased most rapidly between 0 and 2 years. The growth trends of D2 and D4 were conformed to the logarithmic curve, whereas those of D1 and D3 conformed to the power curve, whose growth rate did not change much. In our measurements, no significant difference was observed in most of the indicators between the left and right sides. However, the right side of D1, D2, and D4 was significantly greater than the left side in 6–7, 4–5, and 8–9 year old children, respectively. Other studies have reported no significant difference between the two sides [9, 10, 29]. However, Chamoun [9] reported that partial anatomical parameters of the atlas were different between the two sides. Not excluding measurement errors, the differences may be related to sex, growing environment, and different ethnic groups. Further studies are needed with a higher sample size in these age groups.
The difference between atlas lateral mass screws and pedicle screws lies in the entry point and direction of the screw [31, 32]. Because the bones of children are still small, it is difficult to implant simple atlas lateral mass screws or pedicle screws with a screws of 3.5-mm diameter in younger children [6, 9, 11]. However, the inferior C1 arch notching technique can provide more space for screw placement than simple lateral mass screw [11]. That is, D2 intersects the posterior edge of the pedicle by inserting a screw slightly laterally from the pedicle, as shown in this study.
In our study, the height of the atlas lateral mass was less than the width, so the height of lateral mass affected the diameter of the screw. The length of the lateral mass determines the length of the screw. According to the results of the lateral mass height, the lateral mass height of children aged 0–1 year did not reach 3.5 mm. Thus, atlantoaxial screw fusion was not feasible with conventional 3.5-mm screws available in the market. At the age of 1–2 years, the height of the lateral mass reaches more than 3.5 mm; therefore, theoretically, screws with a diameter of 3.5 mm can be used. However, the two layers of cortical bone inside and outside the lateral mass also occupy a certain spatial distance, which can be challenging for a 3.5-mm screw. We suggested that the lateral mass of the atlas screws can be directly used with a 3.5-mm thick screw in children of age 2 years or older. For children younger than 2 years of age, we can design screws with a diameter of 3.0 or even 2.5 mm, when a surgery is necessary. Previous studies [29, 33, 34] have indicated that 3.5-mm screw insertion of the lateral mass of the atlas can be performed in 2-year-old children. However, Chamoun [9] reported that the lateral mass of the atlas in a 1.5-year-old child could be placed with a 3.5-mm screw through measuring CT images of 76 children aged 1.5–16 years.
The distance between the midline of the long axis of the lateral mass and inner cortex of the front and rear edges of the lateral mass (D2) was 9.560 ± 2.328, 16.500 ± 1.509, 23.446 ± 2.107, and 23.963 ± 2.112 mm at 0–1, 1–2, 6–7, and 7–8 years, respectively; these dimensions were smaller than those measured by Deng [10]. This could be because the CT window measured by Deng was not in the sub-bone window measurement according to the figure in their article. D2 was found to be 25.100 ± 1.83 mm at 13–14 years. However, the distance between the midline of the long axis of the lateral mass and the inner cortex of the front and rear edges of the lateral mass (D5) measured by Chinese studier Ma [35] in fresh male adult caddies was larger than D2 of 13–14-year-old children in our study. Previous studies have shown that the lateral anatomic structure of the atlas at age of 8 years is similar to that of adults [9, 36, 37]. Our trend curve showed that the atlas continues to grow from the age 8 to 14 years, though at a slower rate. Further studies are needed to assess whether the atlas continues to grow after 14 years. When the pedicle screw reached 80% of its entire length, the holding force of the screw was sufficient. There was no significant change in the holding force if the screw insertion depth was further increased [38]. To date, ‘in-out-in’ technique has been performed in the axis [39]. In our study, the distance between the midpoint behind the pedicle and anterior edge of the lateral mass (D4) was measured. It provided a longer nail path in younger children if ‘in-out-in’ technique could be suitable for the atlas.
In our study, there was no significant change in inclination of the atlas lateral mass with age. α, the average inclination angle ranged from 12.41° to 20.97°, which was similar to that reported by Rocha and Chamoun [9, 40] but was larger than that measured by Deng [10] and smaller than that measured by Wang [41]. A screw with a very large inclination angle can easily enter in the spinal canal, whereas that with a very small inclination angle can easily injure the vertebral artery. However, it is necessary to perform a preoperative CT examination to ensure that the screw is inside the lateral mass.
As mentioned above, previous studies have had a small age span, less detailed subgroups, and a relatively small number of cases. In our study, children from each age group (0–14 years) were considered. The age span from 0 to 14 years old could help in analyzing the growth and development of children’s atlas in a better way, which is the biggest highlight of this study. However, similarly to the study by Geck [29], we did not analyze the differences as per sex. Chamoun [9] found that a few anatomical indicators were different between males and females. There may be differences in the atlas development between sexes. We considered the difference between sexes significant only when reaching a certain age, and there will be no sex differences in younger children. There is incomplete ossification of the atlas in 0–2-year-old children, especially in 0–1-year-old ones. Further studies are needed to clarify whether atlas ossification be affected if lateral mass screws are used in 0–2-year-old children.
Conclusion
By assessing the CT images of the atlas in children aged 0–14 years, we concluded that the atlas grew faster in 0–2-year-old children. Posterior lateral mass screw placement could be performed in children older than 2 years by designing 3.5-, 3.0-, or even 2.5-mm screws. Screw length of 10.0 mm can be designed for 0–1-year-old children, and that of 15.0 mm can be used for children aging 1 year and older. Preoperative thin-layer cervical CT is necessary for designing the surgical plan and selection of screws.
Data availability
The data of this study were derived from cervical CT data of outpatients and inpatients who underwent CT examinations in the First Affiliated Hospital of Guangxi Medical University from June 2018 to June 2020.
Code availability
SPSS, PACS, and MIMICS.
References
Lee SH, Park DH, Kim MH, Huh DS, Kang KC, Lee JH, Suk KS, Kim KT (2016) Assessment of the C1 lateral mass screw trajectory and position using plain radiographs: a comparison with computed tomography. Clin Spine Surg 29:E112–E119. https://doi.org/10.1097/bsd.0000000000000113
Yin YH, Yu XG, Qiao GY, Guo SL, Zhang JN (2014) C1 lateral mass screw placement in occipitalization with atlantoaxial dislocation and basilar invagination: a report of 146 cases. Spine 39:2013–2018. https://doi.org/10.1097/brs.0000000000000611
Brooks AL, Jenkins EB (1978) Atlanto-axial arthrodesis by the wedge compression method. J Bone Jt Surg Am 60:279–284
Lee SH, Kim ES, Eoh W (2013) Modified C1 lateral mass screw insertion using a high entry point to avoid postoperative occipital neuralgia. J Clin Neurosci Off J Neurosurg Soc Australas 20:162–167. https://doi.org/10.1016/j.jocn.2012.01.045
Fiore AJ, Haid RW, Rodts GE, Subach BR, Mummaneni PV, Riedel CJ, Birch BD (2002) Atlantal lateral mass screws for posterior spinal reconstruction: technical note and case series. Neurosurg Focus 12:E5. https://doi.org/10.3171/foc.2002.12.1.6
Simsek S, Yigitkanli K, Seçkin H, Comert A, Acar HI, Belen D, Tekdemir I, Elhan A (2009) Ideal screw entry point and projection angles for posterior lateral mass fixation of the atlas: an anatomical study. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 18:1321–1325. https://doi.org/10.1007/s00586-009-1105-7
Hong X, Dong Y, Yunbing C, Qingshui Y, Shizheng Z, Jingfa L (2004) Posterior screw placement on the lateral mass of atlas: an anatomic study. Spine 29:500–503. https://doi.org/10.1097/01.brs.0000113874.82587.33
Dong Y, Hong MX, Jianyi L, Lin MY (2003) Quantitative anatomy of the lateral mass of the atlas. Spine 28:860–863. https://doi.org/10.1097/01.Brs.0000058724.95657.55
Chamoun RB, Whitehead WE, Curry DJ, Luerssen TG, Jea A (2009) Computed tomography morphometric analysis for C-1 lateral mass screw placement in children. Clin Artic J Neurosurg Pediatr 3:20–23. https://doi.org/10.3171/2008.10.Peds08224
Deng XW, Min ZH, Lin B, Zhang FH (2010) Anatomic and radiological study on posterior pedicle screw fixation in the atlantoaxial vertebrae of children. Chin J Traumatol 13:229–233
Lee H, Hong JT, Kim IS, Kim MS, Sung JH, Lee SW (2014) Anatomic feasibility of posterior cervical pedicle screw placement in children: computerized tomographic analysis of children under 10 years old. J Korean Neurosurg Soc 56:475–481. https://doi.org/10.3340/jkns.2014.56.6.475
Huang HK (2003) Some historical remarks on picture archiving and communication systems. Comput Med Imaging Graph Off J Comput Med Imaging Soc 27:93–99. https://doi.org/10.1016/s0895-6111(02)00082-4
Gallie WE (1937) Skeletal traction in the treatment of fractures and dislocations of the cervical spine. Ann Surg 106:770–776. https://doi.org/10.1097/00000658-193710000-00026
Holness RO, Huestis WS, Howes WJ, Langille RA (1984) Posterior stabilization with an interlaminar clamp in cervical injuries: technical note and review of the long term experience with the method. Neurosurgery 14:318–322. https://doi.org/10.1227/00006123-198403000-00010
Jeanneret B, Magerl F, Stanisic M (1986) Thrombosis of the vertebral artery. A rare complication following traumatic spondylolisthesis of the second cervical vertebra. Spine (Phila Pa 1976) 11(2):179–182
Naderi S, Crawford NR, Song GS, Sonntag VK, Dickman CA (1998) Biomechanical comparison of C1-C2 posterior fixations. Cable, graft, and screw combinations. Spine 23:1946–1955. https://doi.org/10.1097/00007632-199809150-00005
Mitchell TC, Sadasivan KK, Ogden AL, Mayeux RH, Mukherjee DP, Albright JA (1999) Biomechanical study of atlantoaxial arthrodesis: transarticular screw fixation versus modified Brooks posterior wiring. J Orthop Trauma 13:483–489. https://doi.org/10.1097/00005131-199909000-00004
Goel A, Laheri V (1994) Plate and screw fixation for atlanto-axial subluxation. Acta Neurochir 129:47–53. https://doi.org/10.1007/bf01400872
Harms J, Melcher RP (2001) Posterior C1-C2 fusion with polyaxial screw and rod fixation. Spine 26:2467–2471. https://doi.org/10.1097/00007632-200111150-00014
Goel A (2002) C1-C2 pedicle screw fixation with rigid cantilever beam construct: case report and technical note. Neurosurgery 51:853–854
Resnick DK, Benzel EC (2002) C1-C2 pedicle screw fixation with rigid cantilever beam construct: case report and technical note. Neurosurgery 50:426–428. https://doi.org/10.1097/00006123-200202000-00039
Tan M, Wang H, Wang Y, Zhang G, Yi P, Li Z, Wei H, Yang F (2003) Morphometric evaluation of screw fixation in atlas via posterior arch and lateral mass. Spine 28:888–895. https://doi.org/10.1097/01.Brs.0000058719.48596.Cc
McAllister AS, Nagaraj U, Radhakrishnan R (2019) Emergent imaging of pediatric cervical spine trauma. Radiogr Rev Publ Radiol Soc N Am Inc 39:1126–1142. https://doi.org/10.1148/rg.2019180100
Platzer P, Jaindl M, Thalhammer G, Dittrich S, Kutscha-Lissberg F, Vecsei V, Gaebler C (2007) Cervical spine injuries in pediatric patients. J Trauma 62:389–396. https://doi.org/10.1097/01.ta.0000221802.83549.46
d’Amato C (2005) Pediatric spinal trauma: injuries in very young children. Clin Orthop Relat Res 432:34–40
Park SW, Cho KH, Shin YS, Kim SH, Ahn YH, Cho KG, Huh JS, Yoon SH (2005) Successful reduction for a pediatric chronic atlantoaxial rotatory fixation (Grisel syndrome) with long-term halter traction: case report. Spine 30:E444–E449. https://doi.org/10.1097/01.brs.0000172226.35474.fe
Hicazi A, Acaroglu E, Alanay A, Yazici M, Surat A (2002) Atlantoaxial rotatory fixation-subluxation revisited: a computed tomographic analysis of acute torticollis in pediatric patients. Spine 27:2771–2775. https://doi.org/10.1097/01.Brs.0000035723.17327.49
Cristante AF, Torelli AG, Kohlmann RB, Dias da Rocha I, Biraghi OL, Iutaka AS, Marcon RM, Oliveira RP, de Pessoa Barros Filho TE (2012) Feasibility of intralaminar, lateral mass, or pedicle axis vertebra screws in children under 10 years of age: a tomographic study. Neurosurgery 70:835–838. https://doi.org/10.1227/NEU.0b013e3182367417
Geck MJ, Truumees E, Hawthorne D, Singh D, Stokes JK, Flynn A (2014) Feasibility of rigid upper cervical instrumentation in children: tomographic analysis of children aged 2–6. J Spinal Disord Tech 27:E110–E117. https://doi.org/10.1097/BSD.0b013e318291ce46
Ferri-de-Barros F, Little DG, Bridge C, Cummine J, Cree AK (2010) Atlantoaxial and craniocervical arthrodesis in children: a tomographic study comparing suitability of C2 pedicles and C2 laminae for screw fixation. Spine 35:291–293. https://doi.org/10.1097/BRS.0b013e3181afea7d
Zhang XL, Huang DG, Wang XD, Zhu JW, Li YB, He BR, Hao DJ (2017) The feasibility of inserting a C1 pedicle screw in patients with ponticulus posticus: a retrospective analysis of eleven patients. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 26:1058–1063. https://doi.org/10.1007/s00586-016-4589-y
Xu G, Wang D, Chen J, Hong Q, Zhuang H (2021) Spiral CT measurement for atlantoaxial pedicle screw trajectory and its clinical application. Am J Transl Res 13:2555–2562
Jea A, Taylor MD, Dirks PB, Kulkarni AV, Rutka JT, Drake JM (2007) Incorporation of C-1 lateral mass screws in occipitocervical and atlantoaxial fusions for children 8 years of age or younger. Technical note. J Neurosurg 107:178–183. https://doi.org/10.3171/ped-07/08/178
Ranade A, Samdani AF, Williams R, Barne K, McGirt MJ, Ramos G, Betz RR (2009) Feasibility and accuracy of pedicle screws in children younger than eight years of age. Spine 34:2907–2911. https://doi.org/10.1097/BRS.0b013e3181b77af3
Ma XY, Yin QS, Liu JF, Zhong SZ, Xia H, Wu ZH (2005) Anatomic and biomechanical comparison between C1 pedicle screw and C1 lateral mass screw. Chin J Bone Jt Inj
Baker C, Kadish H, Schunk JE (1999) Evaluation of pediatric cervical spine injuries. Am J Emerg Med 17:230–234. https://doi.org/10.1016/s0735-6757(99)90111-0
Kokoska ER, Keller MS, Rallo MC, Weber TR (2001) Characteristics of pediatric cervical spine injuries. J Pediatr Surg 36:100–105. https://doi.org/10.1053/jpsu.2001.20022
Brantley AG, Mayfield JK, Koeneman JB, Clark KR (1994) The effects of pedicle screw fit. Vitro Study Spine 19:1752–1758. https://doi.org/10.1097/00007632-199408000-00016
Du YQ, Yin YH, Qiao GY, Yu XG (2020) C2 medial pedicle screw: a novel “in-out-in” technique as an alternative option for posterior C2 fixation in cases with a narrow C2 isthmus. J Neurosurg Spine. https://doi.org/10.3171/2020.2.Spine191517
Rocha R, Safavi-Abbasi S, Reis C, Theodore N, Bambakidis N, de Oliveira E, Sonntag VK, Crawford NR (2007) Working area, safety zones, and angles of approach for posterior C-1 lateral mass screw placement: a quantitative anatomical and morphometric evaluation. J Neurosurg Spine 6:247–254. https://doi.org/10.3171/spi.2007.6.3.247
Wang MY, Samudrala S (2004) Cadaveric morphometric analysis for atlantal lateral mass screw placement. Neurosurgery 54:1436–1439. https://doi.org/10.1227/01.neu.0000124753.74864.07
Funding
Our research was supported by the National Natural Science Foundation of China (No. 81560359, No. 81860393).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no conflict of interest to declare that are relevant to the content of this article.
Ethical approval
Due to the retrospective nature of the study, informed consent was waived. And this study was approved by the Ethics Committee of the First Affiliated Hospital of Guangxi Medical University.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chen, J., Liang, T., Hu, Y. et al. Suitability of 3.5-mm screw for the atlas in children: a retrospective computed tomography analysis. Eur Spine J 31, 1241–1250 (2022). https://doi.org/10.1007/s00586-022-07136-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-022-07136-8