Abstract
Purpose
The purpose of this study was to find out additional indications for multi-positional MRI in cervical degenerative spondylosis (CDS) patients.
Material and methods
A total of 63 patients with cervical spondylotic myelopathy that underwent multi-positional MRI and X-ray were included. Muhle’s grade, C2-7 angle, and C7 slope were measured. Patients were assigned to the stenosis group (Group S) when Muhle’s grades were increased by more than two or maximum grade was reached. Other patients were assigned to the maintenance group (Group M). Receiver operating characteristic (ROC) analysis was performed. Statistical significance was accepted for p values of < 0.05.
Results
A total of 24 patients were assigned to the S group and 39 patients to the M group. Mean C2-7 angle difference in extension (eC27A) between S and M groups was 10.97° (p = 0.002). The mean inter-group difference between C2-7 angle in extension and neutral positions (e-nC27A) was 14.39° (p = 0.000). Mean C7 slope difference in neutral position was − 6.53° (p = 0.002). Based on areas under ROC curves (AUCs), e-nC27A, eC27A, and negative C7 slope had AUCs of 0.934 (95% CI 0.876–0.992), 0.752 (95% CI 0.624–0.880), and 0.720 (95% CI 0.588–0.851), respectively. The optimal cutoff value of e-nC27A was 15.4 degrees, which had a diagnostic accuracy of 88.9%.
Conclusion
Multi-positional MRI helps to find dynamic cord compressive lesion in CDS patients. The higher eC27A, e-nC27A values and smaller C7 slope were found to increase the likelihood of cervical dynamic stenosis. Among other factors, we recommend multi-positional MRI before surgery especially when a patient’s e-nC27A is > 15.4 degrees.
Level of evidence I
Diagnostic: individual cross-sectional studies with the consistently applied reference standard and blinding.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cervical spondylotic myelopathy (CSM) can be caused by various pathologies, such as disc herniation, spondylosis, congenital canal stenosis, and ossification of the posterior longitudinal ligament (OPLL), which may all result in spinal cord impairment and neurological dysfunction [1,2,3,4,5].
Previous studies have demonstrated several important advantages of multi-positional (flexion–extension) MRI, for example, it enables the identification of hidden pathologies, improves diagnostic accuracies, and facilitates understanding of the true natures and extents of pathologies [6, 7].
In a previous study, we showed that spinal canal narrowing, LF thickening, and degree of cervical stenosis are dependent on neck position, cervical spine level, and pathology. These results indicate that dynamic morphometric evaluations are more meaningful in cervical degenerative spondylosis (CDS) than in OPLL, and significant changes occur in CDS patients on moving from neutral to extension positions, especially from the C3-4 to the C6-7 level [6]. And, reliable recommendations have been regarding the use of multi-positional MRI in CDS patients. The purpose of this study was to evaluate the influence of dynamic neck motion on the clinical utility of multi-positional MRI and to find out additional indications for multi-positional MRI in CDS patients.
Materials and methods
During the period February 2014 to July 2017, 112 patients underwent cervical multi-positional MRI and X-ray at our department due to symptoms of CSM but no clear diagnosis after neutral MRI. In all cases, MRI was performed using a 1.5-T or a 3.0-T superconducting MR unit in neutral, flexion, and extension positions. Multi-positional MRI was performed with as much neck flexion and extension as patients were able to achieve unassisted. The extension and flexion were accomplished by a self-designed posture cushion (Fig. 1). The angle of extension and flexion was as can be tolerated for the patient during the imaging time. For the multi-positional MRI, the surface coil was removed in order to allow complete flexibility of the neck and of the head in a sagittal plane between flexion (Fig. 1a) and extension (Fig. 1b).
T1- and T2-weighted sequences were obtained in sagittal and axial planes by neutral MRI, but only T2-weighted images were obtained by multi-positional MRI.
Patients with a congenital anomaly, OPLL, trauma, instability, tumor, previous history of cervical fusion, or ankylosing spondylitis were excluded [6, 8,9,10,11].
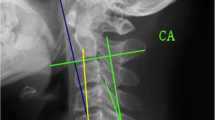
Morphometric analysis was performed in three different positions: neutral, flexion, and extension. Muhle’s grades were determined in neutral and multi-positional MR images from C2-3 to C7-T1. The four-stage Muhle’s classification (Table 1) was used to assess degree of cervical stenosis on axial and sagittal T2-weighted MR images [12]. Preoperative lateral standing plain radiographs were obtained in neutral, flexion, and extension positions. The following parameters were evaluated (Fig. 2): C2-7 angle (the angle created by a line parallel to the inferior end plate of the C2 body and a line parallel to that of the C7 body was measured on neutral, flexion, and extension position), and C7 slope (the angle between a horizontal line and the superior end plate of C7) [13]. C2-7 angle was measured in the neutral position (nC27A), in the flexion position (fC27A), and in the extension position (eC27A). Difference between C2-7 angles in extension and neutral positions was calculated (e-nC27A).
All parameters were measured and classified using INFINIT PACS (INFINIT Healthcare Co. Ltd., Seoul).
Patients were divided into two groups based on multi-positional MRI findings. Patients were assigned to the stenosis group (Group S) when an increase of more than two Muhle’s grades was observed or when maximum Muhle’s grade was reached on multi-positional MRI. Other patients were assigned to the maintenance group (Group M). The statistical analysis was performed using SPSS Version 18.0.0 (SPSS Inc, Chicago, IL, USA), and results are presented as means ± SDs. The independent sample’s t test and the paired t test were used to analyze normally distributed data, and the Mann–Whitney rank test was used for non-normally distributed data. Receiver operating characteristic (ROC) analysis was performed in order to determine the influence of dynamic neck motion on the clinical utility of multi-positional MRI. The area under the ROC curve (AUC) was subsequently calculated where a value of 1 represents a perfect fit. Based on these AUCs, the abilities of imaging studies to predict the need for multi-positional MRI were classified as follows: 0.9–1.0 (excellent), 0.8–0.9 (good), 0.7–0.8 (fair), 0.6–0.7 (poor), and 0.5–0.6 (fail) [14]. To measure the diagnostic accuracy, we estimated several kinds of values, sensitivity, specificity, positive and negative predicative values (PPV, NPV) [15]. Diagnostic accuracy (effectiveness) provides another global measure of diagnostic accuracy and is expressed as the proportion of correctly classified subjects (true positive + true negative) among all subjects [15].
Statistical significance was accepted for p values of < 0.05.
Results
After exclusions, 63 of the initially considered 112 patients were included in the study. Overall mean age was 68.0 ± 11.4 years (range 44–87 years). There were 39 males (61.9%) and 24 females (38.1%) enrolled in this study (Table 2). There was no statistical difference in age and sex between two groups.
The interobserver reliabilities of morphometric measurements were determined by subjecting the results of 63 patients obtained by two spine surgeons, and the intraobserver reliabilities of morphometric measurements were determined 2 month later by one spine surgeon to interrater correlation coefficient analysis. ICCs for inter- (0.852, 95% CI; 0.824 ~ 0.875) and intra- (0.872, 95% CI; 0.848 ~ 0.892) observer agreements for measured Muhle’s grades were “excellent.” And then, we enrolled 24 patients in the S (stenosis) group by Muhle’s grade change on multi-positional MRI. (Fig. 3).
In the S group, mean plain radiograph preoperative C2-7 angle was 10.49° ± 11.33° in the neutral position (nC27A) and was 33.23° ± 12.19° while in the extension position (eC27A). Mean difference between preoperative C2-7 angles in extension and neutral positions was 22.74° ± 9.32° (e-nC27A), and mean plain radiograph preoperative C7 slope was 18.06° ± 7.83°.
In the M group, the mean nC27A was 14.01° ± 12.73°, mean eC27A was 22.26° ± 13.42°, mean e-nC27A was 8.35° ± 5.07°, and mean plain radiograph preoperative C7 slope was 24.59° ± 7.45°.
Mean eC27A difference between the S and M groups was 10.97° (p = 0.002), mean preoperative e-nC27A difference was 14.39° (p = 0.000), and mean preoperative C7 slope in the neutral position difference was − 6.53° (p = 0.002, Table 3).
C2-7 angle differences between plain radiography and MRI in neutral and extension positions were observed in both groups but were not statistically significant (Table 4).
On increasing eC27A and e-nC27A, C7 slope reduced, and the change in stenosis grade in neutral and extension MR images increased. ROC analysis was used to compare the abilities of C2-7 angle and C7 slope to predict the need for multi-positional MRI. Based on areas under ROC curves (AUCs), e-nC27A had an AUC of 0.934 (95% CI; 0.876–0.992), eC27A had an AUC of 0.752 (95% CI; 0.624–0.880), and a negative C7 slope had an AUC of 0.720 (95% CI; 0.588–0.851) (Fig. 4).
We calculated optimal cutoff values derived from maximum sensitivity and specificity values, and we checked the diagnostic accuracies of cervical parameters. The optimal cutoff value for e-nC27A was 15.4 degrees, which had a sensitivity of 75.0%, a specificity of 97.4%, a positive predictive value of 94.7%, a negative predictive value of 86.3%, and a diagnostic accuracy of 88.9%. The optimal cutoff value of eC27A was 29.1 degrees, which had a sensitivity of 70.8%, a specificity of 76.9%, a positive predictive value of 65.4%, a negative predictive value of 81.1%, and a diagnostic accuracy of 74.6%. Optimal cutoff value of a negative C7 slope was − 22.8 degrees, which had a sensitivity of 75.0%, a specificity of 59.0%, a positive predictive value of 52.9%, a negative predictive value of 79.3%, and a diagnostic accuracy of 65.1% (Table 5).
Discussion
Degenerative spinal changes occur over time in all individuals, and it has been reported that spinal canal size decreases with age [16]. This reduction increases the likelihood of CSM, which is the most common cause of cervical spinal cord dysfunction in the elderly population. Therefore, it is imperative that degrees of canal stenosis and cord compression can be assessed when evaluating CSM patients. In this context, the degenerative causes of spinal cord compression may be more exacerbated under cervical dynamic motion, and multi-positional MRI has recently been reported to be diagnostically useful in CSM patients. [17]
In a previous study, mean LF thickness in the CDS patients increased significantly on moving from neutral to extension at C3-4, C4-5, and C5-6. Thus, it would appear differences between segmental motions in CSD patients may explain observed differences in spinal Muhle`s grades and LF thicknesses, especially in extension. [6] Furthermore, it has also been reported extension MRI revealed a higher rate of cervical stenosis possibly associated with LF buckling and reductions in subarachnoid space and spinal canal diameter. [18]
Although multi-positional MRI is being increasingly used to evaluate cervical spine pathologies, it has not been universally accepted. Moreover, little consensus exists regarding the routine application of preoperative multi-positional MRI in clinical situations or its indications [19].
We previously reported that morphologic changes of the stenotic cervical spine differ in patients with CDS and OPLL. [17] Changes in canal diameter and ligamentum flavum thickness were significantly greater and segmental motion ranges were wider in CDS patients, which may have been caused by segmental immobility due to OPLL progression. Restricted segmental motion in the OPLL group might have explained the smaller changes in LF thickness and canal diameter observed in this group. However, no study has addressed the relationship between dynamic changes in canal stenosis and cervical alignment, and no consensus has been reached on the indications for multi-positional MRI in CDS patients.
The present study provides data on the influences of dynamic neck motion and cervical alignment on morphometric changes of the cervical spinal canal based on MR images acquired in the routine neutral, flexion, and extension positions. We observed that grades of stenosis in extension were significantly higher than grades in other positions (Fig. 3), and that morphologic changes were significantly greater in the S group. In addition, higher eC27A and e-nC27A values and smaller C7 slopes were found to be associated with greater changes in stenosis grades between the neutral and extension positions. These findings suggest that the clinical usefulness of multi-positional MRI is patient dependent and provides clues regarding the precise indications for multi-positional MRI in CDS patients.
Case illustrations show representative differences between the S group (Fig. 5) and M group (Fig. 6) with respect to morphologic changes in cervical spinal canals. When the neck was extended in the S group patient, the upper and subaxial cervical spine were generally extended and cervical stenosis increased. Muhle’s grade changes were as follows; C4-5 (G0 = > G2), C5-6 (G2 = > G3), and C6-7 (G1 = > G3). In addition, spinal cord signal intensity changes were marked. For this S group patient, the surgical level should have included C4-5–6-7. In contrast, in the M group patient, when the neck was extended, the upper cervical spine was largely extended, and little change of subaxial motion was observed. So, there were no Muhler’s grade changes in this M group patient. The present study shows that performing multi-positional MRI is clinically indicated especially for CDS patients with higher eC27A, e-nC27A and smaller C7 slope angles.
Case illustrations of S group patient. a and b lateral X-rays show C2-7 angle increased from neutral to extension position. And all parameters (e-nC27A, eC27A and negative C7 slope) were included to derived cutoff values. As a result, cervical stenosis was progressed. c Neutral MRI shows canal stenosis and cord signal change at the level of C5 and C6. (white arrow) d Extension MRI shows the degree and levels of canal stenosis are aggravated. (blue arrow)
Case illustrations of M group patient. a and b lateral X-rays show C2-7 angle change is not prominent from neutral to extension position. c and d Cervical stenosis was not progressed. Neutral and extension MRIs demonstrate that when 45,232 neck was extended, the upper cervical angle was mainly changed and changes in subaxial cervical spine are rarely observed
Morphologic changes in CDS patients encompass osteoarthritic degeneration (i.e., cervical spondylosis) and ligamentous aberrations (i.e., hypertrophy of the ligamentum flavum) [20]. Accordingly, if C7 slope is increased by congenital or degenerative spinal alignment changes, resulting forward bending pressure of neck posture increases and promotes cervical spondylosis progression and the rigidity of subaxial cervical extension muscle. As a result, neck extension mobility is reduced, and as shown by our results, eC27A and e-nC27A are decreased.
Based on our ROC analysis, e-nC27A, eC27A, and a negative C7 slope had AUCs of 0.934 (95% CI 0.876–0.992), 0.752 (95% CI 0.624–0.880), and 0.720 (95% CI 0.588–0.851), respectively. These findings suggest that multi-positional cervical MRI has greater ability to find a hidden pathology or accurately determine the number of levels required for surgical decompression especially when the patient’s e-nC27A value is > 15.4 degrees. These results provide background data that can be used to determine when to use multi-positional MRI in cervical spine patients.
The present study has several limitations that warrant consideration. First, this was a single-center study conducted with a small sample size, so further larger-scale studies are needed to clarify differences in characteristics and amounts of dynamic changes in patients with different cervical alignments and dynamic neck motions. Second, the dynamic movement in recumbent position does not always reproduce the real dynamic pathology. Care must be taken to interpret the findings of MRI in recumbent position that cannot always represent the real pathology. The dynamic upright MRI could give some additional information of the actual pathophysiology with gravitational effects of the head. Third, the study was retrospective and non-blinded. Fourth, we only included elderly patients, and thus, our results cannot be generalized. Fifth, we did not analyze signal change and functional change of spinal cord, which may be dependent on each different cervical position.
Conclusion
We investigated the cervical stenosis changes between neutral MR and multi-positional MR images according to several radiographic parameters. The higher eC27A, e-nC27A values and smaller C7 slope were found to be associated with the risk of cervical dynamic stenosis and of morphological changes of the spinal canal. Our findings lead us to recommend multi-positional MRI before surgery especially when a patient’s e-nC27A value is > 15.4 degrees.
References
Nouri A, Tetreault L, Singh A, Karadimas SK, Fehlings MG (2015) Degenerative cervical myelopathy: epidemiology, genetics, and pathogenesis. Spine 40:E675-693. https://doi.org/10.1097/brs.0000000000000913
Lee HJ, Kim IS, Sung JH, Lee SW, Hong JT (2016) Significance of multimodal intraoperative monitoring for the posterior cervical spine surgery. ClinNeurolNeurosurg 143:9–14. https://doi.org/10.1016/j.clineuro.2016.02.007
Kim JY, Kwon JY, Kim MS, Lee JJ, Kim IS, Hong JT (2018) Comparison of morphological characteristics of the subaxial cervical spine between athetoid cerebral palsy and normal control. J Korean NeurosurgSoc 61:243–250. https://doi.org/10.3340/jkns.2017.0303.011
Lee HJ, Kim JH, Kim IS, Hong JT (2018) Anatomical evaluation of the vertebral artery (V2) and its influence in cervical spine surgery. ClinNeurolNeurosurg 174:80–85. https://doi.org/10.1016/j.clineuro.2018.09.002
Lee HJ, Kim JH, Kim IS, Hong JT (2019) Physiologic cervical alignment change between whole spine radiographs and normal standing cervical radiographs. World Neurosurg 122:e1222–e1227. https://doi.org/10.1016/j.wneu.2018.11.019
Lee JB, Kim IS, Kwon JY, Lee JJ, Park JH, Cho CB, Yang SH, Sung JH, Hong JT (2018) Difference of dynamic morphometric changes between in patients with ossification of posterior longitudinal ligament and patients with cervical spondylosis: assessment by cervical dynamic magnetic resonance imaging. World Neurosurg. https://doi.org/10.1016/j.wneu.2018.11.213
Nigro L, Donnarumma P, Tarantino R, Rullo M, Santoro A, Delfini R (2017) Static and dynamic cervical MRI: two useful exams in cervical myelopathy. J Spine Surg 3:212–216. https://doi.org/10.21037/jss.2017.06.01
Hong JT, Sung JH, Son BC, Lee SW, Park CK (2008) Significance of laminar screw fixation in the subaxial cervical spine. Spine 33:1739–1743. https://doi.org/10.1097/BRS.0b013e31817d2aa2
Hong JT, Kim IS, Kim JY, Lee HJ, Kwon JY, Kim MS, Sung JH (2016) Risk factor analysis and decision-making of surgical strategy for V3 segment anomaly: significance of preoperative CT angiography for posterior C1 instrumentation. Spine J 16:1055–1061. https://doi.org/10.1016/j.spinee.2016.04.019
Kim IS, Hong JT, Lee JJ, Lee JB, Cho CB, Yang SH, Sung JH (2018) A novel technique for cervical laminoplasty fusion: simultaneously enhancing stabilization and decompression in various cervical myelopathies: a technical note and outcomes. World Neurosurg 111:361–366. https://doi.org/10.1016/j.wneu.2018.01.018
Kim IS, Hong JT, Jang WY, Yang SH, Sung JH, Son BC, Lee SW (2011) Surgical treatment of osodontoideum. J ClinNeurosci 18:481–484. https://doi.org/10.1016/j.jocn.2010.07.114
Muhle C, Metzner J, Weinert D, Falliner A, Brinkmann G, Mehdorn MH, Heller M, Resnick D (1998) Classification system based on kinematic MR imaging in cervical spondylitic myelopathy. AJNR Am J Neuroradiol 19:1763–1771
Hyun SJ, Kim KJ, Jahng TA, Kim HJ (2016) Relationship between T1 slope and cervical alignment following multilevel posterior cervical fusion surgery: impact of T1 slope minus cervical lordosis. Spine 41:E396-402. https://doi.org/10.1097/brs.0000000000001264
Hanley JA, McNeil BJ (1982) The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology 143:29–36. https://doi.org/10.1148/radiology.143.1.7063747
Simundic AM (2009) Measures of diagnostic accuracy: basic definitions. Ejifcc 19:203–211
Nagata K, Yoshimura N, Hashizume H, Muraki S, Ishimoto Y, Yamada H, Takiguchi N, Nakagawa Y, Minamide A, Oka H, Kawaguchi H, Nakamura K, Akune T, Yoshida M (2014) The prevalence of cervical myelopathy among subjects with narrow cervical spinal canal in a population-based magnetic resonance imaging study: the Wakayama Spine Study. Spine J 14:2811–2817. https://doi.org/10.1016/j.spinee.2014.03.051
Lee JB, Kim IS, Kwon JY, Lee JJ, Park JH, Cho CB, Yang SH, Sung JH, Hong JT (2019) Difference of dynamic morphometric changes between in patients with ossification of posterior longitudinal ligament and patients with cervical spondylosis: assessment by cervical dynamic magnetic resonance imaging. World Neurosurg 123:e566–e573. https://doi.org/10.1016/j.wneu.2018.11.213
Tykocki T, du Plessis J, Wynne-Jones G (2018) Correlation between the severity of myelopathy and cervical morphometric parameters on dynamic magnetic resonance imaging. ActaNeurochir (Wien) 160:1251–1258. https://doi.org/10.1007/s00701-018-3540-x
Kolcun JP, Chieng LO, Madhavan K, Wang MY (2017) The role of dynamic magnetic resonance imaging in cervical spondylotic myelopathy. Asian Spine J 11:1008–1015. https://doi.org/10.4184/asj.2017.11.6.1008
Badhiwala JH, Wilson JR (2018) The Natural history of degenerative cervical myelopathy. NeurosurgClin N Am 29:21–32. https://doi.org/10.1016/j.nec.2017.09.002
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has any potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lee, J.B., Park, J.H., Lee, J.J. et al. Influence of dynamic neck motion on the clinical usefulness of multi-positional MRI in cervical degenerative spondylosis. Eur Spine J 30, 1542–1550 (2021). https://doi.org/10.1007/s00586-021-06760-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-021-06760-0