Abstract
Purpose
This study aims to assess the nerve function deficient recovery in surgically treated patients with cervical trauma with spinal cord injury (SCI) in chronic stage and figure out prognostic predictors of improvement in impairment and function.
Methods
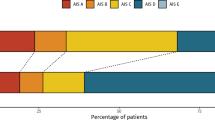
We reviewed the clinical and radiological data of 143 cervical SCI patients in chronic stage and divided into non-operative group (n = 61) and operative group (n = 82). The severity of neurological involvement was assessed using the ASIA motor score (AMS) and Functional Independence Measure Motor Score (FIM MS). The health-related quality of life was measured using the SF-36 questionnaire. Correspondence between the clinical and radiological findings and the neurological outcome was investigated.
Results
At 2-year follow-up, surgery resulted in greater improvement in AMS and FIM MS than non-operative group. Regression analysis revealed that lower initial AMS (P = 0.000), longer duration after injury (P = 0.022) and injury above C4 level (P = 0.022) were factors predictive of lower final AMS. Longer duration (P = 0.020) and injury above C4 level (P = 0.010) were associated with a lower FIM MS. SF-36 scores were significantly lower in higher age (P = 0.015), female patients (P = 0.009) and patients with longer duration (P = 0.001).
Conclusion
It is reasonable to consider surgical decompression in patients with cervical SCI in chronic stage and persistent spinal cord compression and/or gross cervical instability. Initial AMS, longer duration, injury above C4 level, higher age and female patients are the five major relevant factors of functional recovery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cervical trauma with spinal cord injury (SCI) is common in China. It is usually seen in patients with cervical stenosis or spondylosis who sustain a hyperextended or complicated force to the cervical spine, it can also present in patients with acute traumatic cervical disk herniations or acute fractures and fracture/dislocations of the cervical spine with instability [1]. Cervical SCI can lead to paralysis, sensory impairment and bowel, bladder and sexual dysfunction. It has an immense social and financial impact on society.
The efficacy and timing of surgical decompression after an acute cervical SCI remain one controversial topic, especially for the patients without acute fractures and fracture/dislocations. Conservative treatment does have some effect on the recovery of nerve function, but most of patients still suffer from persistent neurological deficits that interfere with activities of daily living. Several authors have suggested potential benefits of early surgical intervention [2, 3]. More recently, a large prospective multicenter study showed that decompression prior to 24 h after SCI can be performed safely and is associated with improved neurologic outcome defined as at least a 2 grades American Spinal Injury Association (ASIA) improvement. Other studies reported similar findings [4,5,6,7].
The present status of treatment for acute cervical SCI is more complicated in China. Some of the patients did not undergo early surgery after injury due to iatrogenic factors such as misdiagnosis and severe comorbidities. However, social factors such as deficient emergency patients transport and care system, lacking of hospitalizing compliance and economic reasons also hindered early surgery for acute cervical SCI patients. As SCI changed in the progression from the acute to chronic stages, part of patients would seek further treatment because of unsatisfied neurological recovery with conservative treatment. Surgical decompression would be adopted on a delayed basis, but the surgical efficacy is still uncertain. The purpose of this study was to assess the nerve function deficient recovery in surgically treated patients with cervical SCI in chronic phase and identify prognostic predictors of improvement in impairment and function.
Material and methods
Study population
From April 1999 through March 2017, one hundred and fifty-five patients with cervical SCI in chronic stage (later than 2 months after cervical injury) were included in the study. The data were divided into two groups according to therapy method: Operative group underwent surgery, and non-operative group refused surgery and insisted on conservative treatment. Diagnosis of cervical SCI will be made on the patient’s history, including physical and neurological examinations, and the results of imaging studies, including plain radiographs, magnetic resonance imaging (MRI) and computed tomography (CT). The surgical indications for chronic spinal cord injury include spinal instability and spinal cord compressions such as osteophytes, disk herniation and hypertrophied ligaments. In order to evaluate the surgical efficacy better, we only included the patients with incomplete SCI (AIS grade C–D). The exclusion criteria were as follow: pre-injury major neurologic deficits or disease (i.e., ischemic stroke, Parkinson’s disease); patients with severe spinal fracture or dislocation; less than 1 months after initial injury.
Surgical treatment
All surgeries were performed by one single surgical team who were all experienced with cervical spine surgery. The choice of the operation was dependent on the characteristics of cord compression. Large osteophyte and disk complexes extending posterior to the vertebral body were decompressed by corpectomy with instrumentation. If compression was caused by anterior degenerative disk, discectomy with instrumentation was performed. The standard Smith-Robinson approach was used to expose the anterior cervical disk. Cervical fusion was performed with PEEK interbody cage and/or titanium mesh cage (DePuy Spine, New Brunswick, New Jersey) combined with locking plate fixation (DePuy Spine, New Brunswick, New Jersey). Posterior laminectomy with instrumentation would be performed for cervical canal stenosis patients. For laminectomy, a midline incision and standard subperiosteal dissection were made to expose the posterior elements of cervical spine. Cervical lateral mass and pedicle screws were inserted and contoured titanium rods were attached to the screws. Laminectomy of affected segments was performed by using a rongeur and high-speed bur. Autogenous bone grafts from the lamina were placed adjacent to the joints to enhance posterior fusion. All patients received hyperbaric oxygen treatments and intensive rehabilitation and wore Philadelphia collars for an average of 10 weeks after operation.
Conservative treatment
All the patients who refused operation would receive appropriate treatment measures, including rehabilitation physiotherapy and oral intake of mecobalamin 500 mg tid for 3 months. Patients were instructed to wear neck collars for 3 months.
Clinical assessment
Operative patients would be evaluated two weeks, three months, 6 months, 1 year and 2 years after operation. While non-operative patients would be followed 2 weeks, 3 months, 6 months, 1-year and 2 years after their first clinic visit. The severity of neurological involvement and functional recovery was assessed using the ASIA motor score (AMS) and Functional Independence Measure Motor Score (FIM MS). The health-related quality of life was measured using the SF-36 questionnaire. Complications rates and mortality were also assessed in this study. The following data were also recorded for each patient: history; symptoms at admission; duration of symptoms; physical and neurological findings at presentation; intraoperative spinal observations; and preoperative and postoperative radiological findings.
Statistical analysis
Data were analyzed using Microsoft Excel 2010 (Microsoft, Redmond, Washington) and SPSS version 19.0 software (SPSS, Inc, Chicago, Illinois). The quantitative data such as age and AMS are presented as the mean ± sd. Inter-group comparisons were made by t test. Chi-square test was used for categorical data. Regression modeling was performed using the following dependent variables: final AMS, FIM MS and SF-36. Independent variables analyzed include age, gender, duration after injury, injury level, head injury, stenosis, intramedullary increased signal intensity (ISI) on T2WI of MRI and ossification of posterior longitudinal ligaments (OPLL). A P value less than 0.05 was considered statistically significant.
Results
Patients data
Seven patients were excluded because they did not complete 2-year follow-up. Five patients were excluded because they changed with operation during follow-up. The study group comprised of 31 women and 112 men. According to the treatment options, these patients were divided into two groups, operative group and non-operative group. Eighty-two patients who underwent operation were classified as the operative group, and 61 patients who insisted on conservative treatment were categorized as the non-operative group. Table 1 summarizes the demographics of the patients, imaging results and clinical therapeutic effects of the two groups. There was no significant difference in age or duration between the two groups. In all two groups, the majority of patients were male.
Reasons that patients miss their chance of early surgical treatment including: fear of surgery (51 cases, 35.7%), medical expenses (32 cases, 22.4%), other surgical contraindications (22 cases 15.4%), distrust in doctors (18 cases, 12.6%), misdiagnosis (12 cases, 8.4%) and others (8 cases, 5.6%). Reasons making chronic cervical SCI patients agree to surgery include: poor efficacy of conservative treatment (49 cases, 59.8%), surgical contraindication eliminated (15 cases, 18.3%), misdiagnosis (11 cases, 13.4%) and others (7 cases, 8.5%).
Operation versus conservative treatment
AMS and FIM MS were statistically different between pre-operation and post-operation in operative group. As compared with the non-operative group, significant improvement of post-op AIS score and FIM MS was shown in operative group. There was significant difference in clinical effects between the two groups.
Analysis of factors associated with surgery results
At the time of first clinic visit, initial AMS was an average of 49.59 ± 11.21. At follow-up, the final AMS was a mean of 67.63 ± 12.37; regression analysis revealed that final AMS was most strongly predicted by the initial AMS (P = 0.0000), duration (P = 0.022) and injury above C4 level (P = 0.022). In operative group of 82 patients, the mean FIM MS was 72.16 ± 16.69. Regression analysis revealed a higher FIM MS with shorter duration after injury (P = 0.020), suggesting a higher level of function in patients. Injury above C4 level was associated with a lower FIM MS (P = 0.010). Regression analysis revealed that the SF-36 scores were significantly lower in higher age, female patients and patients with long duration after injury. (P = 0.015, 0.009 and 0.001). (Table 2).
Discussion
Although some studies showed no benefit to early decompression [8], most spine surgeons favor early decompression to avoid missing the potential therapeutic window in the acute phase [3, 5,6,7]. With incomplete SCI, there is the greatest evidence for improved neurological function with early surgery [9]. However, patients with acute cervical SCI are commonly managed with delayed surgical intervention [10, 11]. Samuel et al. [12] found that the majority of patients with SCI did not undergo surgery within the first 24 h after injury, and the majority of delays occurred after inpatient admission. Most of them could get surgical treatment in 83.1 h. Few patients could not be treated in time. In our study, we found deficient emergency patients transport might not be the main cause for delaying treatment, and the delay time is longer either in China. Social factors resulting in delayed surgical intervention should not be ignored. Fear of surgery risks and medical expenses are two leading causes of rejecting surgery in acute period. The individual healthcare financial impact remains an important determinant for people making medical decisions. An opinion piece recently published in the Lancet argued that increased out-of-pocket health care costs are a major cause of patient dissatisfaction [13, 14]. Indeed, insufficient propaganda of medical knowledge and asymmetry of information have prompted fears of surgery and risk. The third-ranked reason was distrust in medical staff. Shan et al. found that trust was the most important factor contributing to patient satisfaction. A wide range of factors (poor facilities, cumbersome procedures, empathic staff attitudes ward environment, etc.) complicates patient’s distrust in health providers in China, and hence, reinstating and maintaining patient trust is a great challenge in China. Nevertheless, 59.8% of cervical SCI patients in chronic phase sought surgery because of unsatisfied functional recovery with conservative treatment in our study.
Although missed the best time for surgical treatment, we found operation in chronic stage still had clinical significance. Current concepts of the pathophysiology of acute SCI indicate that there are both primary and secondary mechanisms that lead to neurologic injury. The primary injury usually results from rapid spinal cord compression and contusion. Secondary injury is a cascade of pathophysiological events including edema, ischemia, inflammation and apoptosis following the initial impact, which develops within minutes to hours following the trauma. Laboratory evidences support the theory that early decompression might alleviates ‘secondary injury’ and results in enhanced neurological and functional recovery [15]. Neurological functions of patients receiving conservative treatment were partly recovered, but only reached a therapeutic plate with different degrees of myelopathy, radiculopathy or both. Nerve compression and instability of cervical spine could be observed in imaging examinations. In our study, we found clinical outcomes of surgical patients were superior to patients insist on conservative treatment. Surgery combined with internal fixation can decompress the spinal cord and obtain the stability for the injured cervical spine. It might be beneficial for the function recovery of nerve and reverses the loss of neurological function.
Significant improvements of Post-op AMS and FIM MS were shown in the operative group, some risk factors might affect the prognosis of the operation. Severity of SCI and duration of ischemia still are the main decisive factors. We found initial AMS and long duration were associated with less functional recovery. For severe obsolete injury patients with low initial AMS, SCI may have caused severe irreversible pathological changes. Even if decompression is thorough, recovery of nerve function is not obvious. Other studies also have found that low initial AMS indicated poor functional recovery [16,17,18]. Vidal et al. [19] demonstrated that patients with longer duration exhibited smaller functional improvements in functional recovery. Their data demonstrate that longer duration exacerbates reperfusion injury and is associated with ongoing enhanced levels of cytokine expression, microglia activation, and astrogliosis and paralleled with poorer neurological recovery. Meanwhile, SCI in the upper cervical region (levels C1–C4) was associated with less functional recovery. It might be related to greater associated deficits after injury (neurological dysfunction, blood pressure lability with unopposed vagal signaling and pulmonary infection) [12].
There have only been a few studies that have reported gender disparities in reported satisfaction measures. Most of the studies have associated the female gender with poorer postoperative satisfaction scores across surgical specialties [20], including after spinal surgery [21,22,23]. In a previous national EQ-5D survey, women had significantly lower scores than men. Women suffered more from anxiety and depression and felt more painful [24]. Shabat et al. concluded that the reasons were multifactorial and not related to the surgery. Women also had a 15% higher risk of undergoing further surgery [24]. Similarly, our reported satisfaction scores demonstrated that male patients tended to be satisfied with their outcomes compared with female patients.
The present investigation has several limitations. First, our study is limited because of the relatively small number of patients. Second, different pathologies found in MRI, including edema, contusion and hemorrhage, to some extent, correlate with the neurologic deficit. We recognized that our patient group was heterogeneous, and the cases involved different kinds of pathology. Third, we did not endeavor to compare different surgical techniques. This area has been examined in the literature without conclusive evidence and is an important area of further research. Prospective randomized trials will be imperative to compare outcomes associated with surgical versus medical management.
Conclusion
In conclusion, we suggest that surgical intervention can be safely applied for obsolete cervical SCI patients with persistent spinal cord compression and/or gross cervical instability. The overall improvement in AMS and FIM MS was relatively satisfactory. The improvements in the AMS and FIM MS were negatively correlated with severe SCI (lower initial AMS), longer duration and injury above C4 level. Women tend to have less satisfactory results than men. Carefully examination of clinical and radiological findings may provide an important basis for selection of the appropriate treatment method.
References
Lenehan B, Fisher CG, Vaccaro A, Fehlings M, Aarabi B, Dvorak MF (2010) The urgency of surgical decompression in acute central cord injuries with spondylosis and without instability. Spine 35:S180-186. https://doi.org/10.1097/BRS.0b013e3181f32a44
Guest J, Eleraky MA, Apostolides PJ, Dickman CA, Sonntag VK (2002) Traumatic central cord syndrome: results of surgical management. J Neurosurg 97:25–32. https://doi.org/10.3171/spi.2002.97.1.0025
Chen L, Yang H, Yang T, Xu Y, Bao Z, Tang T (2009) Effectiveness of surgical treatment for traumatic central cord syndrome. J Neurosurg Spine 10:3–8. https://doi.org/10.3171/2008.9.spi0822
La Rosa G, Conti A, Cardali S, Cacciola F, Tomasello F (2004) Does early decompression improve neurological outcome of spinal cord injured patients? appraisal of the literature using a meta-analytical approach. Spinal Cord 42:503–512. https://doi.org/10.1038/sj.sc.3101627
Umerani MS, Abbas A, Sharif S (2014) Clinical outcome in patients with early versus delayed decompression in cervical spine trauma. Asian Spine J 8:427–434. https://doi.org/10.4184/asj.2014.8.4.427
Mattei TA (2012) Surgical decompression after spinal cord injury: the earlier, the better! World Neurosurg 78:384–387. https://doi.org/10.1016/j.wneu.2012.09.004
Fehlings MG, Rabin D, Sears W, Cadotte DW, Aarabi B (2010) Current practice in the timing of surgical intervention in spinal cord injury. Spine 35:S166-173. https://doi.org/10.1097/BRS.0b013e3181f386f6
Park MS, Moon SH, Lee HM, Kim TH, Oh JK, Suh BK, Lee SJ, Riew KD (2015) Delayed surgical intervention in central cord syndrome with cervical stenosis. Glob Spine J 5:69–72. https://doi.org/10.1055/s-0034-1395785
Dvorak MF, Noonan VK, Fallah N, Fisher CG, Finkelstein J, Kwon BK, Rivers CS, Ahn H, Paquet J, Tsai EC, Townson A, Attabib N, Bailey CS, Christie SD, Drew B, Fourney DR, Fox R, Hurlbert RJ, Johnson MG, Linassi AG, Parent S, Fehlings MG (2015) The influence of time from injury to surgery on motor recovery and length of hospital stay in acute traumatic spinal cord injury: an observational Canadian cohort study. J Neurotrauma 32:645–654. https://doi.org/10.1089/neu.2014.3632
Stevens EA, Marsh R, Wilson JA, Sweasey TA, Branch CL Jr, Powers AK (2010) A review of surgical intervention in the setting of traumatic central cord syndrome. Spine J Off J North Am Spine Soc 10:874–880. https://doi.org/10.1016/j.spinee.2010.07.388
Yoshihara H, Yoneoka D (2013) Trends in the treatment for traumatic central cord syndrome without bone injury in the United States from 2000 to 2009. J Trauma Acute Care Surg 75:453–458. https://doi.org/10.1097/TA.0b013e31829cfd7f
Samuel AM, Bohl DD, Basques BA, Diaz-Collado PJ, Lukasiewicz AM, Webb ML, Grauer JN (2015) Analysis of delays to surgery for cervical spinal cord injuries. Spine 40:992–1000. https://doi.org/10.1097/brs.0000000000000883
Xu W (2014) Violence against doctors in China. Lancet (London, England) 384:745. https://doi.org/10.1016/s0140-6736(14)61438-0
Huang SL, Ding XY (2011) Violence against Chinese health-care workers. Lancet (London, England) 377:1747. https://doi.org/10.1016/s0140-6736(11)60732-0
Carlson GD, Gorden CD, Oliff HS, Pillai JJ, LaManna JC (2003) Sustained spinal cord compression: part I: time-dependent effect on long-term pathophysiology. J Bone Jt Surg Am 85:86–94
Dvorak MF, Fisher CG, Hoekema J, Boyd M, Noonan V, Wing PC, Kwon BK (2005) Factors predicting motor recovery and functional outcome after traumatic central cord syndrome: a long-term follow-up. Spine 30:2303–2311. https://doi.org/10.1097/01.brs.0000182304.35949.11
Kaminski L, Cordemans V, Cernat E, M’Bra KI, Mac-Thiong JM (2017) Functional outcome prediction after traumatic spinal cord injury based on acute clinical factors. J Neurotrauma 34:2027–2033. https://doi.org/10.1089/neu.2016.4955
Montoto-Marqués A, Trillo-Dono N, Ferreiro-Velasco ME, Salvador-de la Barrera S, Rodriguez-Sotillo A, Mourelo-Fariña M, Galeiras-Vázquez R, Meijide-Failde R (2018) Risks factors of mechanical ventilation in acute traumatic cervical spinal cord injured patients. Spinal Cord 56:206–211. https://doi.org/10.1038/s41393-017-0005-7
Vidal PM, Karadimas SK, Ulndreaj A, Laliberte AM, Tetreault L, Forner S, Wang J, Foltz WD, Fehlings MG (2017) Delayed decompression exacerbates ischemia-reperfusion injury in cervical compressive myelopathy. JCI Insight. https://doi.org/10.1172/jci.insight.92512
Baker PN, van der Meulen JH, Lewsey J, Gregg PJ (2007) The role of pain and function in determining patient satisfaction after total knee replacement. Data from the national joint registry for England and Wales. J Bone Jt Surg Br 89:893–900. https://doi.org/10.1302/0301-620x.89b7.19091
Shabat S, Folman Y, Arinzon Z, Adunsky A, Catz A, Gepstein R (2005) Gender differences as an influence on patients’ satisfaction rates in spinal surgery of elderly patients. Euro Spine J Off Publ Euro Spine Soc Euro Spinal Deform Soc Euro Sect Cerv Spine Res Soc 14:1027–1032. https://doi.org/10.1007/s00586-004-0808-z
Jansson KA, Németh G, Granath F, Jönsson B, Blomqvist P (2009) Health-related quality of life (EQ-5D) before and one year after surgery for lumbar spinal stenosis. J Bone Jt Surg Br 91:210–216. https://doi.org/10.1302/0301-620x.91b2.21119
Elsamadicy AA, Reddy GB, Nayar G, Sergesketter A, Zakare-Fagbamila R, Karikari IO, Gottfried ON (2017) Impact of gender disparities on short-term and long-term patient reported outcomes and satisfaction measures after elective lumbar spine surgery: a single institutional study of 384 patients. World Neurosurg 107:952–958. https://doi.org/10.1016/j.wneu.2017.07.082
Burström K, Johannesson M, Diderichsen F (2001) Health-related quality of life by disease and socio-economic group in the general population in Sweden. Health Policy (Amsterdam, Netherlands) 55:51–69. https://doi.org/10.1016/s0168-8510(00)00111-1
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ji, C., Rong, Y., Jia, H. et al. Surgical outcome and risk factors for cervical spinal cord injury patients in chronic stage: a 2-year follow-up study. Eur Spine J 30, 1495–1500 (2021). https://doi.org/10.1007/s00586-020-06703-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-020-06703-1