Abstract
Purpose
The thoracolumbar junction (TLJ) has not been explored in regard to its contribution to global sagittal alignment. This study aims to define novel sagittal parameters of the TLJ and to assess their roles within global sagittal alignment.
Methods
Included for cross-sectional, retrospective analysis were asymptomatic volunteers and symptomatic patients who had undergone operation for adult spinal deformity. Unique sagittal parameters of the TLJ were measured using the midline of the T12–L1 disk space: The TLJ orientation [TLJO; thoracolumbar tilt (TLT) and slope (TLS)]. Thoracic kyphosis (TK; T5–12), C7–S1 sagittal vertical axis (SVA), lumbar lordosis (LL; L1–S1), sacral slope (SS), pelvic tilt (PT), and pelvic incidence (PI) were measured. Continuous variables were compared using the independent t test. Pearson correlations examined relationships between the parameters in each group. The asymptomatic TK was calculated using the measurement of the asymptomatic volunteer’s TLJO by linear regression.
Results
One hundred fifteen asymptomatic volunteers and 127 symptomatic patients were included. Only LL among the lumbopelvic parameters correlated with TK (asymptomatic volunteers: r = − 0.42; symptomatic patients: r = − 0.40). All the pelvic parameters have no direct correlation with TK in both groups. TLJO had stronger correlation with TK [asymptomatic volunteers: r = − 0.68 (TLS), r = 0.41 (TLT); symptomatic patients: r = − 0.56 (TLS), r = 0.44 (TLT)] than the lumbopelvic parameters. TLS correlated with LL (asymptomatic volunteers: r = 0.78; symptomatic patients: r = 0.73). Most pelvic parameters correlated with TLJO except for PI. The asymptomatic TK was estimated by the derived formula: 20.847 + TLS × (− 1.198).
Conclusion
The TLJO integrates the status of the lumbopelvic sagittal parameters and simultaneously correlates with thoracic and global sagittal alignment.
Graphic abstract
These slides can be retrieved under Electronic Supplementary Material.

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
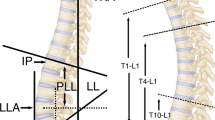
Pelvic alignment [pelvic tilt (PT), sacral slope (SS), and pelvic incidence (PI)] efficiently represents the orientation and foundation of sagittal alignment [1]. Based on pelvic alignment, sagittal balance has been described as reciprocal curves of lumbar lordosis (LL) and thoracic kyphosis (TK) [2,3,4]. In accordance with “the cone of economy,” the concept of tilt and slope might be maximally appropriate for describing the orientation of any specific alignment in sagittal balance [5]. The human body axis tends to be maintained in a certain range from the center of gravity to reduce energy expenditure. Tilt represents the distance of the starting point from the center, while slope represents the degree of inclination of the starting point. Consequently, the angle above a certain point in the human body axis may be influenced by these two values (Fig. 1).
Thoracolumbar junction tilt (TLT) and slope (TLS) in the concept of “Cone of Economy” of the human body’s axis. a TLT represents how far the vertebral body is as a starting point from the center of gravity. b TLS represents how much inclined the vertebral body is as a starting point from horizontal line. c The angle in the compensatory zone is determined by a and b since the human body’s axis tends to be maintained in the cone around the center of gravity to reduce energy expenditure. c will be high if a is high (the starting point of the thoracolumbar junction is far from center), or if b is high (the more inclined the starting point is from horizontal line)
The thoracolumbar junction (TLJ) is a transitional zone between TK and LL. The kyphotic position of the thoracic spine and the body’s center of gravity being located anterior to the spine causes compressive forces to be transmitted anterior to the vertebral body along with a tensile stretch or distraction of the posterior elements. In the lordotic region of the lower lumbar spine, forces are transferred more posteriorly relative to the spine, and thus, these compressive loads pass through the posterior elements [6]. Accordingly, severe posterior displacement (tilt) or inclination (slope) of TLJ may also create significant flexion moment on the thoracic spine. The significance of this biomechanical environment has been clinically emphasized in various pathologic situations that occur with greater frequency at the TLJ, including vertebral compression fractures with or without progressive kyphosis and proximal junctional kyphosis (PJK) following adult spinal deformity operations [7, 8].
Sagittal alignment of the thoracolumbar junction has traditionally been assessed using the thoracolumbar Cobb angle, which is measured from the cranial endplate of T10 to the caudal endplate of L2 [9]. While this radiographic assessment is well accepted, previous studies have failed to address or demonstrate a significant role to sagittal alignment or correlate it with other sagittal alignment parameters [7, 10]. This limitation may originate from the fact that this isolated angle dose not accurately or comprehensively represent the TLJ’s orientation with regard to sagittal balance.
As such, the present study’s aim is twofold: (1) to highlight radiographic sagittal parameters of the thoracolumbar junction, including thoracolumbar tilt (TLT) and thoracolumbar slope (TLS), to capture its sagittal orientation (thoracolumbar junction orientation; TLJO) (Fig. 2), and (2) to assess these parameters’ correlation with tradition sagittal radiographic parameters. We hypothesize that the TLJO will correlate with lumbopelvic alignment (PI, SS, PT, and LL) and determine thoracic kyphosis and overall sagittal plane alignment in both asymptomatic and symptomatic adults.
Thoracolumbar junction orientation—thoracolumbar tilt (TLT) and slope (TLS). a The TLT is the angle between the line connecting the midline of the T12–L1 disk space to the center axis of the femoral heads and a vertical reference line. TLT(a) is a positive value similar to pelvic tilt. b The TLS is the angle between the midline of the T12–L1 disk space and a horizontal reference line. TLS(b) is negative value similar to the sacral slope
Methods
Patient cohorts
After obtaining institutional review board approval, a retrospective analysis of patients with full-length spine radiographs evaluated in a single tertiary referral center’s spine clinic was conducted. Included for analysis were asymptomatic volunteers, 18–79 years, without axial neck or back pain and symptomatic patients who had undergone operative intervention for adult spinal deformity. Enrollment details for the cohort of the asymptomatic volunteers have been previously described [11]. Specifically, asymptomatic volunteers were included if they had no coronal deformities (Cobb angle > 10°), a history of prior spine surgery, history of hip or knee arthroplasty or any other realignment surgery of the lower extremities (osteotomy, trauma, etc.), complaints of back pain or neck pain that resulted in missed work, affected activities of daily living, participation in recreational activities or required narcotic pain medication, degenerative or pathologic condition of the spine that necessitated physician intervention (i.e., physician appointment or epidural steroid injections), non-ambulatory patients, history of neuromuscular disorders, inflammatory arthritis, or congenital anomalies, and pregnancy [11]. Institutional review board approval was obtained to analyze this cohort of asymptomatic volunteers retrospectively.
Patients within the cohort of the symptomatic patients underwent long construct posterior instrumented spinal fusions from the TLJ to the sacrum performed by two senior spinal surgeons from 2004 to 2014 for primary sagittal and coronal deformity. The radiological inclusion criteria was scoliosis angles of ≥ 20°, sagittal vertical axis (SVA) of ≥ 5 cm, PT angle of ≥ 25°, and/or TK angle of > 60°. The symptomatic patients all had a primary surgical deformity correction. Preoperative radiographic data were used for analysis for the symptomatic patients.
Radiographic assessments
Three unique sagittal parameters of the TLJ were measured (Fig. 2). The constellation of these two parameters make up the thoracolumbar junction orientation (TLJO).
-
(1)
Thoracolumbar Tilt (TLT, Fig. 2a): angle between the line perpendicular to the midline of the T12–L1 disk space at its midpoint and the line connecting this point to the midpoint of the femoral head axis. This is a positive value similar to pelvic tilt.
-
(2)
Thoracolumbar Slope (TLS, Fig. 2b): angle between the midline of the T12–L1 disk space and a horizontal reference line and the TLT as the angle between the line connecting the midline of the T12–L1 disk space to the center axis of the femoral heads and a vertical reference line. This is a negative value similar to sacral slope.
Additional sagittal radiographic parameters measured above and below the thoracolumbar junction included: thoracic kyphosis (TK; sagittal Cobb angle from cranial endplate of T5 to the caudal endplate of T12), global sagittal alignment (C7–S1 SVA; horizontal distance from the plumb line from the center of the C7 vertebral body to the posterior S1 prominence), lumbar lordosis (LL; sagittal Cobb angle between cranial endplate of L1 to the cranial endplate of S1) and pelvic alignment (SS, PT, and PI). All radiographic analyses were performed using Surgimap Spine (Nemaris, Inc., New York, NY) by two experienced spinal surgeons.
Statistical analysis
Statistical analyses were performed using IBM SPSS Statistics, version 22 (IBM Corp., Armonk, NY). Measured radiographic values were described as means with standard deviations. Continuous variables were compared using independent t test. Pearson correlations were used to determine relationships among radiographic parameters in each group. Asymptomatic TK was determined from asymptomatic volunteers’ TLJO using linear regression. P-values and correlation strengths were interpreted according to Evans [12] (r = 0.00–0.19: very weak; r = 0.20–0.39: weak; r = 0.40–0.59: moderate; r = 0.60–0.79: strong; and r = 0.80–1.00: very strong). Correlation of r ≥ 0.6 was highlighted to decrease the risk of statistical error. Analyses were exploratory, and significance was defined as p < 0.05 for all comparisons.
Results
Cohort comparisons (Table 1)
A total of 242 patients were included with 115 in the asymptomatic volunteers and 127 in the symptomatic patients. Asymptomatic volunteers were significantly younger than symptomatic patients. The groups were similar in regard to BMI. As expected, symptomatic patients had significantly higher average score for the Oswestry Disability Index and abnormal global and lumbopelvic sagittal parameters. Pelvic incidence was significantly greater in the symptomatic patients.
Descriptive statistics of the SVA and TK between the asymptomatic volunteers and symptomatic patients Symptomatic patients had greater forward SVA (asymptomatic volunteers: − 6.8 cm ± 34.8 cm; symptomatic patients: 5.4 cm ± 6.5 cm, p = 0.000). Asymptomatic volunteers had greater thoracic kyphosis (asymptomatic volunteers: 34.1° ± 12.6°; symptomatic patients: 23.5° ± 13.8°, p = 0.000).
Descriptive statistics of the TLJO between the asymptomatic volunteers and symptomatic patients The average TLS was − 21.0° ± 7.7° and − 3.5° ± 11.6° (p = 0.000), respectively. The average TLT was 9.9° ± 4.5° and 11.5° ± 7.2° (p = 0.041), respectively.
Descriptive statistics of the PT, SS, PI, and LL between the asymptomatic volunteers and symptomatic patients The average LL was − 57.2° ± 13.0° and − 33.4° ± 18.0° (p = 0.000), respectively. The average PT was 14.3° ± 8.6° and 24.6° ± 9.8° (p = 0.000), respectively. The average SS was 36.5° ± 9.3° and 30.7° ± 11.2° (p = 0.000), respectively. The average PI was 49.6° ± 12.1° and 55.3° ± 13.1° (p = 0.000), respectively.
Correlations of thoracic spine to sagittal alignment parameters without using the concept of TLJO
Asymptomatic volunteers (Fig. 3)
TK showed moderate correlation with LL (r = − 0.42, p = 0.000), but no direct correlation with SS (r = − 0.02, p = 0.877), PT (r = + 0.03, p = 0.728), and PI (r = − 0.03, p = 0.745). LL showed weak correlation with PI (r = − 0.38, p = 0.000) and strong one with SS (r= − 0.76, p = 0.000).
Symptomatic patients (Fig. 4)
TK showed moderate correlation with LL (r = − 0.40, p = 0.000), but no direct correlation with SS (r = − 0.02, p = 0.832), PT (r = + 0.03, p = 0.721), and PI (r = − 0.11, p = 0.244). LL showed weak correlation with PI (r = − 0.26, p = 0.000), strong one with SS (r = − 0.69, p = 0.000), and moderate one with PT (r = + 0.45, p = 0.000).
Correlations of thoracic spine to sagittal alignment parameters with inclusion of the concept of TLJO
Asymptomatic volunteers (Fig. 5)
The TLS and TLT were correlated with TK and SVA (all p = 0.000). The correlations were strong between TLS and TK (r= − 0.68); moderate between TLS and SVA (r = 0.55), TLT and TK (r = 0.41); and weak between TLT and SVA (r = − 0.28). Asymptomatic TK was determined from the asymptomatic volunteers’ TLS using the following formula: 20.847 + TLS × (− 1.198).
With regard to lumbopelvic parameters, the TLJO was not correlated with PI. TLS has strong correlation with LL (r= 0.78, p = 0.000) and weak correlation with SS (r = − 0.30, p = 0.000). TLT has moderate correlation with SS (r = − 0.44, p = 0.000) and weak correlation with PT (r = 0.37, p = 0.000).
Symptomatic patients (Fig. 6)
The TLS and TLT were correlated with TK and SVA (all p = 0.000). The correlations were strong between TLS and SVA (r = + 0.75); moderate between TLS and TK (r = − 0.56), TLT and TK (r = + 0.44), and TLT and SVA (r = − 0.56).
With regard to lumbopelvic parameters, TLS has strong correlation with LL (r = 0.73, p = 0.000) and weak correlation with PT (r = 0.37, p = 0.000). TLT has moderate correlation with PI (r = − 0.42, p = 0.000) and weak correlation with SS (r = − 0.38, p = 0.000).
Discussion
Reciprocal thoracic kyphosis is an important phenomenon to follow after long fusion surgery from thoracolumbar junction to the pelvis. As reciprocal thoracic kyphosis may lead to proximal junctional problems, sagittal decompensation, and deterioration of clinical outcomes after deformity correction surgery, [2,3,4, 13, 14] realignment of and inclusion of the thoracic spine in the instrumented fusion has been proposed. However, a detailed understanding and quantitative method to assess the phenomenon of reciprocal thoracic kyphosis are not available. The present study aims to address this by defining new radiographic sagittal parameters to describe the orientation of the TLJ and comparing these new parameters to the traditional global and lumbopelvic sagittal radiographic parameters.
That TLJO (TLT and TLS) is significantly correlated with both TK is one of major findings of our study. This suggests that the TLJO can determine sagittal alignment by reflecting the concept of “the cone of economy.” The correlations in both groups consistently showed that as the TLT increased (the further the TLJ was from the center) and as the TLS increases in magnitude (TLJ became more inclined), a higher TK angle was demanded to maintain body axis within the cone.
Lumbopelvic alignment can affect the overall sagittal balance. However, the previous studies consistently present that TK is not correlated with PT, SS, and PI [15,16,17], but has weak correlation (r = 0.35 [15], r = 0.27 [16], r = 0.35 [17]) with LL. The present study also confirmed that pelvic alignment had no direct influence on the TK in the both groups, although it might have some indirect influence on the TK through LL (Figs. 3 and 4). There has been clinical demand that can investigate how the TK could be changed in terms of proximal junctional kyphosis and reciprocal change in TK. The TLJO can be a “checkpoint” for sagittal alignment, since it integrates the status of the lumbopelvic alignment and simultaneously showed stronger correlations with TK than other lumbopelvic parameters (Figs. 5 and 6).
LL itself was also correlated with TK directly and main contributor to TLS (Figs. 3 and 4). However, the TLS might be a more reasonable parameter than LL for investigating TK, since it showed a “strong” correlation with TK (Figs. 5 and 6). This could be from the fact that TLJO include the distribution as well as the amount of lordosis. Since Boissière et al. [18] introduce the lumbar lordosis index as the critical parameter in sagittal alignment, the clinical importance of the distribution of lordosis has increased. For example, two lumbar spines with the same lordosis magnitude, but with varying regional distribution of lordosis, may be reflected by different TLS values. A lumbar spine with the majority of lordosis located in the lower lumbar levels would likely have a lower TLS than a lumbar spine with the majority of lordosis located in the mid- and/or upper lumbar levels. (Fig. 7) Moreover, as LL showed complex correlations with pelvic alignment parameters that were not correlated with TK, LL is not the ideal parameter to evaluate reciprocal changes in TK (Figs. 3 and 4).
Schematic drawing of different thoracolumbar slopes with the same amount of lordosis. Different thoracolumbar slopes depend on the distribution of lordosis. A lumbar spine with the majority of lordosis located in the lower lumbar levels will likely have a lower TLS than a lumbar spine with the majority of lordosis located in the mid- and/or upper lumbar levels
Symptomatic patients with spinal deformity who required surgical intervention had representative characteristics of sagittal imbalance and related compensatory features, including increased C7–S1 SVA, loss of LL, increased PT, decreased SS, and decreased TK compared to asymptomatic volunteers. The relatively higher PI in symptomatic patients is also consistent with findings of a previous study [19]. In the asymptomatic volunteers, the correlation between TLS/TLT and TK was stronger than the one between TLS/TLT and SVA. In contrast, the correlation between TLS/TLT and SVA was stronger than the one between TLS/TLT and TK in the symptomatic patients. This might be reasonable because TK in the asymptomatic volunteers has a better corresponding curve to TLS/TLT than the one in the symptomatic patients. The major difference that emerged in the symptomatic patients compared to the asymptomatic volunteers was that influence of the PT on the LL newly developed, which could make the correlations between the lumbopelvic alignments and TK more complicated (Figs. 5 and 6). However, as correlations between TLJO and pelvic alignment and between TK and TLJO were consistent in asymptomatic volunteers and symptomatic patients, the TLJO could consistently integrate complex relationships within the lumbopelvic alignment and transfer them to the sagittal alignment above the TLJ regardless of various compensatory mechanisms (Fig. 4b).
The present study also found that the asymptomatic TK angle can be calculated using linear regression based on strong and consistent correlations between TLJO parameters and TK. The TLS in asymptomatic volunteers may be the best parameters to calculate the asymptomatic TK angle, as it showed the strongest and most consistent correlation with sagittal alignment parameters above the TLJ (i.e., SVA and TK) in both the asymptomatic volunteers and symptomatic patients. While this parameter may be used individually to calculate the necessary TK angle for each patient to maintain asymptomatic sagittal alignment, it may not be ideal since our asymptomatic volunteers included those with advanced age and degenerative features.
Another important finding of this study is that LL was the main contributor to the TLJO in both the asymptomatic volunteers and symptomatic patients. This implies that TLJO can be a practical reference, since LL is a critical issue in any kind of pathologic condition and a major target of correction to restore sagittal balance. For example, excessive restoration of LL may lead to excessive increase in TLS and reciprocal TK. The permissive upper limit of restoration of LL can be proposed through the TLS to prevent against detrimental progression of TK after deformity correction surgery. Conversely, surgical considerations to avoid remarkable increases in TLS can also be addressed to maintain long-term sagittal balance when aggressive restoration of LL is mandatory.
The findings of this study should be considered within its limitations. Several limitations include its retrospective and cross-sectional design. In order to better evaluate the association of the TLJO parameters with other sagittal parameters, a consecutive series that includes larger cohorts would be essential. Another major concern consists in the fact that the location of TLJ can be changeable according to type of spinal alignment if it is considered as the inflection point between LL and TK [20, 21]. However, Roussouly et al. reported type 3 lordosis, the majority of normative data [20], had an inflection point at T12-L1, which is the location we chose to assign as the TLJ [21]. Furthermore, though the number of vertebral bodies in a lordotic orientation varied from 1 to 8, the mean value was 4 (type 1), 5 (type 2), 4.5 (type 3), and 5 (type 4) [20]. While the TLJ junction may vary by Roussouly subtype, we chose to standardize the location of the TLJ measurements at T12-L1, as determining an individualized inflection point and assigning a Roussouly subtype to each patient with a spinal deformity is likely not achievable.
Conclusion
In this single-center analysis focusing on thoracolumbar junction orientation, there are two important conclusions. The first is that SS, PT, and PI are not correlated with TK in both the symptomatic patients and asymptomatic volunteers. The second conclusion is that the TLJO integrates the status of the lumbopelvic sagittal parameters and simultaneously correlates with thoracic and global sagittal alignment. As such, the TLJO may have a role in understanding TK and overall sagittal balance beyond lumbopelvic parameters in various clinical situations. However, a future study that assesses the clinical application and effect of the TLJO on reciprocal changes in TK and PJK after thoracolumbar kyphosis correction is necessary to ultimately determine the utility of using the TLJO parameters to guide surgical correction of sagittal plane deformities. The data presented herein would ideally be used as the impetus for these future investigations.
References
Celestre PC, Dimar JR, Glassman SD (2018) Spinopelvic parameters: lumbar lordosis, pelvic incidence, pelvic tilt, and sacral slope—what does a spine surgeon need to know to plan a lumbar deformity correction? Neurosurg Clin N Am 29:323–329. https://doi.org/10.1016/j.nec.2018.03.003
Barrey C, Roussouly P, Perrin G, Le Huec JC (2011) Sagittal balance disorders in severe degenerative spine. Can we identify the compensatory mechanisms? Eur Spine J 20(Suppl 5):626–633. https://doi.org/10.1007/s00586-011-1930-3
Jang JS, Lee SH, Min JH, Maeng DH (2009) Influence of lumbar lordosis restoration on thoracic curve and sagittal position in lumbar degenerative kyphosis patients. Spine 34:280–284. https://doi.org/10.1097/BRS.0b013e318191e792
Lafage V, Ames C, Schwab F, Klineberg E, Akbarnia B, Smith J, Boachie-Adjei O, Burton D, Hart R, Hostin R, Shaffrey C, Wood K, Bess S (2012) Changes in thoracic kyphosis negatively impact sagittal alignment after lumbar pedicle subtraction osteotomy: a comprehensive radiographic analysis. Spine 37:E180–E187. https://doi.org/10.1097/BRS.0b013e318225b926
Dubousset J (1994) Three-dimensional analysis of the scoliotic deformity. The pediatric spine: principles and practice. Raven Press Ltd, New York
Smith HE, Anderson DG, Vaccaro AR, Albert TJ, Hilibrand AS, Harrop JS, Ratliff JK (2010) Anatomy, biomechanics, and classification of thoracolumbar injuries. Semin Spine Surg 22:2–7. https://doi.org/10.1053/j.semss.2009.10.001
Liu CJ, Zhu ZQ, Wang KF, Duan S, Xu S, Liu HY (2017) Radiological analysis of thoracolumbar junctional degenerative kyphosis in patients with lumbar degenerative kyphosis. Chin Med J (Engl) 130:2535–2540. https://doi.org/10.4103/0366-6999.217090
Cho KJ, Suk SI, Park SR, Kim JH, Jung JH (2013) Selection of proximal fusion level for adult degenerative lumbar scoliosis. Eur Spine J 22:394–401. https://doi.org/10.1007/s00586-012-2527-1
Michael F, O’Brien M, Kuklo TR, Blanke KM, Lenke LG (2008) Spinal deformity study group-radiographic measurement manual. Medtronic Sofamor Danek USA, Inc., Memphis
Jang JS, Lee SH, Min JH, Han KM (2007) Lumbar degenerative kyphosis: radiologic analysis and classifications. Spine 32:2694–2699. https://doi.org/10.1097/BRS.0b013e31815a590b
Iyer S, Lenke LG, Nemani VM, Albert TJ, Sides BA, Metz LN, Cunningham ME, Kim HJ (2016) Variations in sagittal alignment parameters based on age: a prospective study of asymptomatic volunteers using full-body radiographs. Spine 41:1826–1836. https://doi.org/10.1097/brs.0000000000001642
Evans JD (1996) Straightforward statistics for the behavioral sciences. Brooks/Cole Publishing, Pacific Grove
Kim YJ, Bridwell KH, Lenke LG, Rhim S, Cheh G (2006) Sagittal thoracic decompensation following long adult lumbar spinal instrumentation and fusion to L5 or S1: causes, prevalence, and risk factor analysis. Spine 31:2359–2366. https://doi.org/10.1097/01.brs.0000238969.59928.73
Newton PO, Yaszay B, Upasani VV, Pawelek JB, Bastrom TP, Lenke LG, Lowe T, Crawford A, Betz R, Lonner B (2010) Preservation of thoracic kyphosis is critical to maintain lumbar lordosis in the surgical treatment of adolescent idiopathic scoliosis. Spine 35:1365–1370. https://doi.org/10.1097/BRS.0b013e3181dccd63
Mac-Thiong JM, Labelle H, Berthonnaud E, Betz RR, Roussouly P (2007) Sagittal spinopelvic balance in normal children and adolescents. Eur Spine J 16:227–234. https://doi.org/10.1007/s00586-005-0013-8
Berthonnaud E, Dimnet J, Roussouly P, Labelle H (2005) Analysis of the sagittal balance of the spine and pelvis using shape and orientation parameters. J Spinal Disord Tech 18:40–47
Vialle R, Levassor N, Rillardon L, Templier A, Skalli W, Guigui P (2005) Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J Bone Jt Surg Am 87:260–267. https://doi.org/10.2106/jbjs.D.02043
Boissiere L, Bourghli A, Vital JM, Gille O, Obeid I (2013) The lumbar lordosis index: a new ratio to detect spinal malalignment with a therapeutic impact for sagittal balance correction decisions in adult scoliosis surgery. Eur Spine J 22:1339–1345. https://doi.org/10.1007/s00586-013-2711-y
Gottfried ON, Daubs MD, Patel AA, Dailey AT, Brodke DS (2009) Spinopelvic parameters in postfusion flatback deformity patients. Spine J 9:639–647. https://doi.org/10.1016/j.spinee.2009.04.008
Roussouly P, Gollogly S, Berthonnaud E, Dimnet J (2005) Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine 30:346–353
Roussouly P, Nnadi C (2010) Sagittal plane deformity: an overview of interpretation and management. Eur Spine J 19:1824–1836. https://doi.org/10.1007/s00586-010-1476-9
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has any potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Moon, H.J., Bridwell, K.H., Theologis, A.A. et al. Thoracolumbar junction orientation: its impact on thoracic kyphosis and sagittal alignment in both asymptomatic volunteers and symptomatic patients. Eur Spine J 28, 1937–1947 (2019). https://doi.org/10.1007/s00586-019-06078-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-019-06078-y