Abstract
Introduction
We investigated a new metric for assessing the quality of motion of the cervical segments over the arc of extension-to-flexion motion after cervical disc arthroplasty (CDA). We quantified: (1) the amount of motion contributed by individual spinal segments to the total cervical spine motion, termed segmental motion fraction, and its variation throughout the arc of extension-to-flexion motion and (2) how cervical disc arthroplasty using two distinct prosthesis designs may influence the segmental motion contributions.
Materials and methods
We tested 16 human C3–T1 spine specimens under physiologic loads; first intact, after CDA at C5–C6, and then at C5–C6 and C6–C7. The M6-C (Orthofix, USA) and Mobi-C (Zimmer, USA) disc prostheses were used in eight specimens each.
Results and conclusions
The designs of the cervical disc prostheses tested significantly influenced the variation in segmental motion fraction as the spine underwent motion between the endpoints of extension and flexion. While the mean segmental motion contribution to the total cervical motion was not influenced by prosthesis design, the way the motion took place between the extension and flexion endpoints was significantly influenced. The M6-C artificial disc restored physiologic motion quality such that implanted segments continued to function in harmony with other segments of the cervical spine as measured before arthroplasty. Conversely, the Mobi-C prosthesis, while maintaining average motion contributions similar to the pre-implantation values, demonstrated large deviations in motion contribution over the extension-to-flexion arc motion in ten of 16 implanted segments. Such non-physiologic implant kinematics could cause excessive prosthesis wear and motion and stress shielding at adjacent segments.
Graphical abstract
These slides can be retrieved under Electronic Supplementary Material.

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Several clinical studies have shown cervical disc arthroplasty (CDA) to be a viable alternative to anterior cervical discectomy and fusion for the treatment of radiculopathy and myelopathy [1,2,3,4,5,6]. The proposed advantages of disc arthroplasty are based on the premise that preservation of physiologic motions and load sharing at the treated level would mitigate the risk of adjacent segment degeneration. A cervical disc prosthesis can accomplish this goal by restoring physiologic quantity and quality of motion at the treated level.
Clinical studies of cervical spine motion after CDA have focused on range of motion (ROM) using radiographs taken at the two endpoints of the extension-to-flexion arc of motion [7]. Biomechanical studies have also investigated the ROM after CDA for various disc prostheses designs [8,9,10,11,12,13,14]. The results of these clinical and biomechanical studies suggest the ROM by itself does not have the discriminatory ability to distinguish between the motion quality of various prostheses designs.
Individual motion segments of a healthy cervical spine move synchronously throughout the extension-to-flexion arc of motion. Segmental contribution to total cervical spine motion depends on the segment’s bending stiffness and moments applied to the segment. Hypermobility, indicative of an unstable motion segment, may cause a segment’s contribution to vary widely over the arc of motion, thereby disrupting the physiologic load-sharing characteristics of the index segment and the harmony among its neighbouring segments. Segmental motion contribution to total cervical motion was studied by Anderst et al. [15] in control subjects and fusion patients. In the present study, we used this metric to assess the quality of extension-to-flexion motion after CDA. The purpose of our study was to investigate the influence of CDA on the amount of motion contributed by the index segment to the total cervical spine motion and its variation throughout the arc of extension-to-flexion motion.
Materials and methods
Specimens and experimental set-up
The experiments were performed using 16 fresh-frozen human cervical spine specimens (C3–T1) from male and female donors aged 18–60 years with no previous spine surgery and no evidence of vertebral fractures, disc ossification or bridging osteophytes. Spines were assigned to two groups of eight specimens each, with the two groups matched based on age, gender distribution, preoperative C5–C6 and C6–C7 disc heights, and ROM (Table 1).
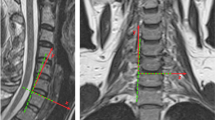
Cervical intervertebral motions were measured using an optoelectronic motion measurement system (Certus, Optotrak®, Northern Digital, Waterloo, Ontario). A six-component load cell placed under the specimen measured the applied compressive preload and moments. Fluoroscopic imaging was used during surgery for implant sizing and placement. Sequential fluoroscopic images were taken from extension to flexion to document any bone–metal interface motions.
The follower load technique [16] was used to apply compressive preloads to the C3–T1 cervical spine during the ROM experiments in flexion–extension since the cervical spine is always under some level of compressive preload due to muscle tone/activity and weight bearing. Details of this methodology are described elsewhere [11, 14].
Cervical disc prostheses
Mobi-C cervical artificial disc
This mobile-core cervical disc prosthesis (Mobi-C, Zimmer-BioMet, Warsaw, Indiana, USA) has three components that form two bearings (joints) (Fig. 1) [17]. The joint formed by the polyethylene mobile core with the superior prosthetic endplate is spherical, which allows three independent angular motions. The core forms a planar joint with the inferior prosthetic endplate, which allows translational motions (up to 1.25 mm) in the sagittal and coronal planes. Thus, the Mobi-C prosthesis allows two degrees of freedom (DOF) in the sagittal plane. In three-dimensional space, the Mobi-C prosthesis allows three independent angular motions and independent translational motions in A–P and lateral directions, yielding a total of five DOF.
M6-C cervical artificial disc
The M6-C (Orthofix, Louisville, Texas, USA) is a non-articulating disc with a polycarbonate–polyurethane (PCU) core that allows compression of the disc prosthesis height [18]. This allows the disc to have all six DOF (Fig. 2). The M6-C disc has an artificial annulus made of polyethylene fibres woven through holes in the two inner metal endplates of the disc. The fibre annulus provides added bending stiffness to the disc.
Experimental protocol
Specimens were first tested in its intact (native) state in flexion–extension ( ± 1.5 Nm) with a compressive preload of 150 N. Subsequently, a C5–C6 disc arthroplasty was performed using either the Mobi-C or the M6-C cervical disc prosthesis (Figs. 3, 4). An anterior discectomy that preserved the structural integrity of the endplates was performed at C5–C6. The posterior longitudinal ligament was transected to facilitate more parallel disc space distraction and proper placement of the prosthesis [11]. Trial sizing was performed to select the prosthesis footprint that maximized the endplate coverage without removing the uncinate processes. The appropriate prosthesis height was selected based on the tightness of the fit, the preoperative intervertebral height at the index level, and the heights of the unaffected adjacent levels. The specimen with a C5–C6 disc arthroplasty then underwent kinematic testing in flexion and extension. In the final step, disc arthroplasty was performed at C6–C7, resulting in two-level disc replacement. Kinematic testing was repeated.
Data analysis
Segmental contribution to total C3–T1 motion (termed, segmental motion fraction)
Vertebral motion data were analysed to calculate segmental motion fractions as the ratios of motion contributions made by C5–C6 and C6–C7 segments to the motion of the C3–T1 spine at each of the approximately 500 data points collected over the extension-to-flexion arc of motion. The segmental motion fraction data were filtered to obtain a smooth curve depicting the contribution of each cervical segment as a fraction of C3–T1 motion throughout the extension-to-flexion motion. The extension-to-flexion motion in degrees was scaled to 0–100% of the arc of motion (Fig. 5). As the specimens had different total C3–T1 ROMs, this allowed us to combine data from all specimens for statistical analysis.
Segmental contribution to C3–T1 motion (termed segmental motion fraction). The extension-to-flexion motion of the C3–T1 spine in degrees was scaled to 0% to 100% of the arc of motion. The variation in the segmental motion fraction over the arc of motion is quantified using the following entities: mean, peak, and RMS error of segmental motion fraction. The average values and standard deviations of these entities were calculated over the eight specimens from each prosthesis group and are presented in Tables 3, 4, and 5
Variability in segmental contribution to total C3–T1 motion
For each cervical spine specimen, we calculated the mean values of segmental (C5–C6 and C6–C7) contributions to the total C3–T1 motion, averaged over the segments’ arc of motion before and after disc arthroplasty (Fig. 5). We also assessed how each segment’s motion contribution varied from its mean over the arc of motion. The variation from mean contribution was evaluated using two metrics:
-
1)
Peak value of segmental motion fraction (Fig. 5).
-
2)
Variance of segmental motion fraction (Fig. 5). Variance was calculated using the following formula:
$$\sigma^{2} = \left[ {\sum \left( {X_{i} - \mu } \right)^{2} } \right]/N$$where σ2 = variance, N = number of data points ( ~ 500) collected over the arc of extension-to-flexion motion, Xi = segmental contribution as a fraction of C3–T1 motion at the ith data point, i = 1, …, N, µ = mean segmental motion fraction calculated over the arc of extension-to-flexion motion, and ∑ = sum calculated over the N number of data points.
A positive square root of the variance was defined as the root mean squared error (RMS error), which is mathematically equivalent to calculating the standard deviation of the segmental motion fraction of an individual segment over the extension-to-flexion motion arc.
Statistical analysis
The segmental motion contributions of C5–C6 and C6–C7 to total C3–T1 motion (segmental motion fractions) were compared before and after disc arthroplasty using paired comparisons (paired t tests). This was done separately for the Mobi-C and M6-C groups. The results of Mobi-C were compared to the M6-C using two-sample comparisons (t-tests). The level of significance was set as alpha = 0.05.
Results
Range of motion (ROM) (Table 2)
The ROM values for the full arc of extension-to-flexion motion were calculated using the extreme flexion and extreme extension positions of the spine segments corresponding to ± 1.5 Nm applied moments. The preoperative ROM values were very comparable between the M6-C and Mobi-C groups across C3–T1 (P = 0.73), C5–C6 (P = 0.70), and C6–C7 (P = 0.68).
The C3–T1 ROM in the M6-C group remained nearly constant after one-level and two-level CDA (57.4° vs. 56.2° vs. 56.8°; P > 0.49). The C5–C6 ROM changed from 14.6° preoperatively to 11.7° after C5–C6 CDA using the M6-C disc (P = 0.13), while the C6–C7 ROM changed from 11.9° to 12.5° after C6–C7 CDA using the M6-C disc (P = 0.54).
Arthroplasty using the Mobi-C disc had a significant effect on the ROM across C3–T1 (54.7° vs. 60.5° vs. 64.7°, P < 0.05), C5–C6 (13.8° vs. 16.8°, P < 0.05), and C6–C7 (12.7° vs. 16.7°, P < 0.05) (Table 2). The C3–T1 ROM increased by about 5° with each disc arthroplasty, resulting in an increase of about 10° in the ROM of C3–T1 after two-level CDA.
Segmental motion fractions: mean, peak, and RMS error (Tables 3, 4, 5)
Preoperatively, the mean segmental motion fraction of the C5–C6 segment during the arc of extension-to-flexion motion was very similar between the M6-C and Mobi-C groups (23.9% vs. 23.0%, P = 0.51) (Table 3). This was also true of the C6–C7 segments (20.1% vs. 21.8%, P = 0.25). The average segmental motion fraction of the C5–C6 and C6–C7 segments did not significantly change after disc arthroplasty using the M6-C disc (C5–C6: 23.9% vs. 22.6%, P = 0.39; C6–C7: 20.1% vs. 22.1%, P = 0.11). Similarly, arthroplasty using the Mobi-C prosthesis did not significantly alter the average contributions made by the C5–C6 and C6–C7 segments to the motion of the C3–T1 spine (C5–C6: 23.0% vs. 22.8%, P = 0.93; C6–C7: 21.8% vs. 19.2%, P = 0.26) (Table 3).
Preoperatively, the peak segmental motion fractions of C5–C6 and C6–C7 segments during the arc of extension-to-flexion motion were similar between the M6-C and Mobi-C groups (C5–C6: 36.1% vs. 33.3%, P = 0.42; C6–C7: 29.3% vs. 32.0%, P = 0.37) (Table 4). CDA using the M6-C prosthesis changed the peak contribution from 36.1 to 38.1% at C5–C6 (P = 0.49) and from 29.3 to 35.3% at C6–C7 (P < 0.05). However, CDA using the Mobi-C prosthesis caused larger increases in the peak segmental motion fractions at C5–C6 and C6–C7 segments (C5–C6: 33.3% vs. 58.6%, P < 0.01; C6–C7: 32% vs. 71.9%, P < 0.01) (Table 4). The peak segmental motion fractions after CDA using Mobi-C were significantly greater than those after CDA using the M6-C disc prosthesis (P < 0.05).
Preoperatively, the RMS error in segmental motion fractions of C5–C6 and C6–C7 segments during the arc of extension-to-flexion motion was similar between the M6-C and Mobi-C groups (C5–C6: 6.4% vs. 4.7%, P = 0.25; C6–C7: 5.1% vs. 4.6%, P = 0.61) (Table 5). CDA using the M6-C prosthesis caused small increases in the RMS error in C5–C6 and C6–C7 segments (C5–C6: 6.4% vs. 8.3%, P = 0.04; C6–C7: 5.1% vs. 7.9%, P = 0.02). However, CDA using the Mobi-C prosthesis caused larger increases in the RMS error of segmental motion fractions at C5–C6 and C6–C7 segments (C5–C6: 4.7% vs. 16.7%, P < 0.01; C6–C7: 4.6% vs. 16.1%, P < 0.01) (Table 5). The RMS error in segmental motion fractions after CDA using Mobi-C was significantly greater than those after CDA using the M6-C disc prosthesis (P < 0.05).
Discussion
In experiments on human cervical spine specimens, we quantified: (1) the amount of motion contributed by individual spinal segments to the total cervical spine motion (segmental motion fraction) and its variation throughout the arc of extension-to-flexion motion and (2) how cervical disc arthroplasty using two distinct prosthesis designs may influence the segmental motion fractions. The designs of the cervical disc prostheses tested in this study (Mobi-C and M6-C) significantly influenced the variation in segmental motion fraction as the spine underwent motion between the endpoints of extension and flexion. While the mean segmental motion contributions to the total cervical motion were not influenced by prosthesis design, the way the motion took place between the extension and flexion endpoints was significantly influenced.
Segmental motion fraction, that is, the contribution of a cervical segment to the motion of the cervical spine, would depend on the stiffness of the segment and the moments acting on the segment (segmental angular motion = applied moment divided by segmental stiffness). Preoperatively, the two specimen groups were nearly identical in the ROM values of C5–C6 and C6–C7 segments (Table 2) and had comparable quality of extension-to-flexion motion as measured by average and peak segmental motion fraction values and RMS errors (Tables 3, 4, 5). Disc arthroplasty using the Mobi-C prosthesis resulted in segmental stiffness that varied substantially over the arc of extension-to-flexion motion in several (10 of 16) implanted segments. This was apparent in the moment versus angular displacement curves (e.g. Fig. 6a), where the slope of the angular displacement versus moment curve after disc arthroplasty was very steep over a small portion of the applied moment, suggesting hypermobility and yielding large variability in the segmental motion fraction of this segment during the spine’s arc of motion (Fig. 6b). This behaviour was not seen in cervical segments that were implanted with the M6-C disc, which showed only small variabilities from the mean segmental motion fractions as reflected in the relatively small peak values of motion fraction and small RMS errors around the mean (Fig. 7a, b). The M6-C design with a compliant core and artificial fibre annulus provides progressive resistance to angular motion, which allows the implanted segment to have physiologic ROM while maintaining stability.
The concepts of segmental motion fraction and its variability during an arc of motion are complements to the segmental angular motion versus applied moment curve. The moment versus angular motion curve (i.e., kinematic signature) of a healthy cervical segment is sigmoidal (see, e.g. Figs. 6a, 7a) and is the net result of progressive resistance offered by the intervertebral disc and ligaments as the segment undergoes gradual angular motion in response to gradually increasing applied moment. It is characterized by a high-flexibility region around the neutral posture, which is capped at both ends by a region of high stiffness due in part to nonlinearly increasing resistance of the disc, tightened ligaments, and load sharing by the facets and facet capsules. One of the clinically relevant measures of quality of motion can be derived from the response of a spinal segment in this region of high flexibility (laxity) around the neutral posture of the spine. Panjabi postulated that an increased laxity, as demonstrated by a substantially decreased stiffness around the neutral posture of the spine (see Fig 6a, curve for Mobi-C), would put increased demand on the spinal musculature to provide the stability needed during activities of daily living [19]. Increased spinal muscle forces would, in turn, increase stresses in the spinal components and may contribute to pain. The variation in segmental motion fraction over the arc of extension-to-flexion motion is a normalized version of the segmental kinematic signature, normalized by the C3–T1 kinematic signature. Since knowledge of applied moment is not needed to calculate segmental motion fraction, it represents a bridge between clinical and laboratory assessments of quality of motion after cervical disc arthroplasty.
In this experiment, each segment of the spine specimen was subjected to equal moments superimposed on a constant compressive preload. Since the segmental motion fractions and their variation are influenced by the type of loading that acts on the spine, the values reported in this article may not be generalized for all activities of daily living. The actual loads acting on the cervical spine in vivo may be different as compared to the laboratory scenario, depending on the activities of daily living. Nevertheless, the methodology presented here offers a standardized way to assess quality of motion (in vivo and in vitro) in implanted segments after CDA.
Change history
22 February 2021
A Correction to this paper has been published: https://doi.org/10.1007/s00586-020-06569-3
References
Sasso R, Anderson P, Riew K et al (2011) Results of cervical arthroplasty compared with anterior discectomy and fusion: four-year clinical outcomes in a prospective, randomized, controlled trial. J Bone Joint Surg Am 93:1684–1692
Coric D, Nunley PD, Guyer RD, Musante D, Carmody CN, Gordon CR et al (2011) Prospective, randomized, multicenter study of cervical arthroplasty: 269 patients from the Kineflex C artificial disc investigational device exemption study with a minimum 2-year follow-up. J Neurosurg Spine 15(4):348–358
Zigler JE, Delamarter R, Murrey D, Spivak J, Janssen M (2013) ProDisc-C and anterior cervical discectomy and fusion as surgical treatment for single-level cervical symptomatic degenerative disc disease: five-year results of a Food and Drug Administration study. Spine 38(3):203–209
Davis RJ, Kim KD, Hisey MS, Hoffman GA, Bae HW, Gaede SE et al (2013) Cervical total disc replacement with the Mobi-C cervical artificial disc compared with anterior discectomy and fusion for treatment of 2-level symptomatic degenerative disc disease: a prospective, randomized, controlled multicenter clinical trial. J Neurosurg Spine 19(5):532–545
Gornet MF, Burkus JK, Shaffrey ME, Argires PJ, Nian H, Harrell FE (2015) Cervical disc arthroplasty with PRESTIGE LP disc versus anterior cervical discectomy and fusion: a prospective, multicenter investigational device exemption study. J Neurosurg Spine 23(5):558–573
Hisey MS, Zigler JE, Jackson R, Nunley PD, Bae HW, Kim KD, Ohnmeiss DD (2016) Prospective, randomized comparison of one-level Mobi-C cervical total disc replacement vs. anterior cervical discectomy and fusion: results at 5-year follow-up. Int J Spine Surg 10:10
Hipp JA, Wharton ND (2008) Quantitative motion analysis (QMA) of motion-preserving and fusion technologies for the spine. In: Motion preservation surgery of the spine. Philadeplhia, Saunders, pp 85–96
Puttlitz CM, Rousseau MA, Xu Z, Hu S, Tay BK, Lotz JC (2004) Intervertebral disc replacement maintains cervical spine kinetics. Spine (Phila Pa 1976) 29:2809–2814
Patwardhan AG, Voronov L, Havey RM, Tzermiadianos M, Carandang G, McIntosh B et al (2009) P152. Limited restoration of primary and coupled motions in lateral bending and axial rotation after total disc replacement: a common finding in cervical disc prostheses. Spine J 9(10):192S–193S (Abstract)
Finn MA, Brodke DS, Daubs M, Patel A, Bachus KN (2009) Local and global subaxial cervical spine biomechanics after single-level fusion or cervical arthroplasty. Eur Spine J 18:1520–1527. https://doi.org/10.1007/s00586-009-1085-7
Patwardhan AG, Tzermiadianos MN, Tsitsopoulos PP, Voronov LI, Renner SM, Reo ML et al (2012) Primary and coupled motions after cervical total disc replacement using a compressible six-degree-of-freedom prosthesis. Eur Spine J 21(5):618–629
Lee MJ, Dumonski M, Phillips FM, Voronov LI, Renner SM, Carandang G et al (2011) Disc replacement adjacent to cervical fusion: a biomechanical comparison of hybrid construct versus two-level fusion. Spine 36(23):1932–1939
Martin S, Ghanayem AJ, Tzermiadianos MN, Voronov LI, Havey RM, Renner SM et al (2011) Kinematics of cervical total disc replacement adjacent to a two-level, straight versus lordotic fusion. Spine 36(17):1359–1366
Havey RM, Khayatzadeh S, Voronov LI, Blank KR, Carandang G, Harding DP, Patwardhan AG (2019) Motion response of a polycrystalline diamond adaptive axis of rotation cervical total disc arthroplasty. Clin Biomech 62:34–41
Anderst WJ, Donaldson WF III, Lee JY, Kang JD (2013) Cervical motion segment percent contributions to flexion-extension during continuous functional movement in control subjects and arthrodesis patients. Spine 38(9):E533
Patwardhan AG, Havey RM, Ghanayem AJ, Diener H, Meade KP, Dunlap B, Hodges SD (2000) Load carrying capacity of the human cervical spine in compression is increased under a follower load. Spine 25(12):1548–1554
Beaurain J, Bernard P, Dufour T, Fuentes JM, Hovorka I, Huppert J et al (2008) Mobi-C. Motion preservation surgery of the spine: advanced techniques and controversies (Part III), pp 231–237
Reyes-Sanchez A, Patwardhan AG, Block JE (2008) The M6 artificial cervical disc. Motion preservation surgery of the spine, Saunders Elsevier, Philadelphia
Panjabi MM (1992) The stabilizing system of the spine. Part II. Neutral zone and instability hypothesis. J Spinal Disord 5:390–396
Acknowledgements
This work was supported in part by research funding from the Department of Veterans Affairs and Chicago Association for Research and Education in Science, Hines, Illinois.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
AG. Patwardhan is a consultant to Orthofix Inc., Lewisville TX, USA. RM. Havey has no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Patwardhan, A.G., Havey, R.M. Prosthesis design influences segmental contribution to total cervical motion after cervical disc arthroplasty. Eur Spine J 29, 2713–2721 (2020). https://doi.org/10.1007/s00586-019-06064-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-019-06064-4